Acute Crit Care.
2024 May;39(2):304-311. 10.4266/acc.2023.01361.
Mortality rates among adult critical care patients with unusual or extreme values of vital signs and other physiological parameters: a retrospective study
- Affiliations
-
- 1Harding Research, LLC, Seattle, WA, USA
- 2Exergen Corp., Watertown, WA, USA
- 3Independent Researcher, Waltham, WA, USA
- KMID: 2557247
- DOI: http://doi.org/10.4266/acc.2023.01361
Abstract
- Background
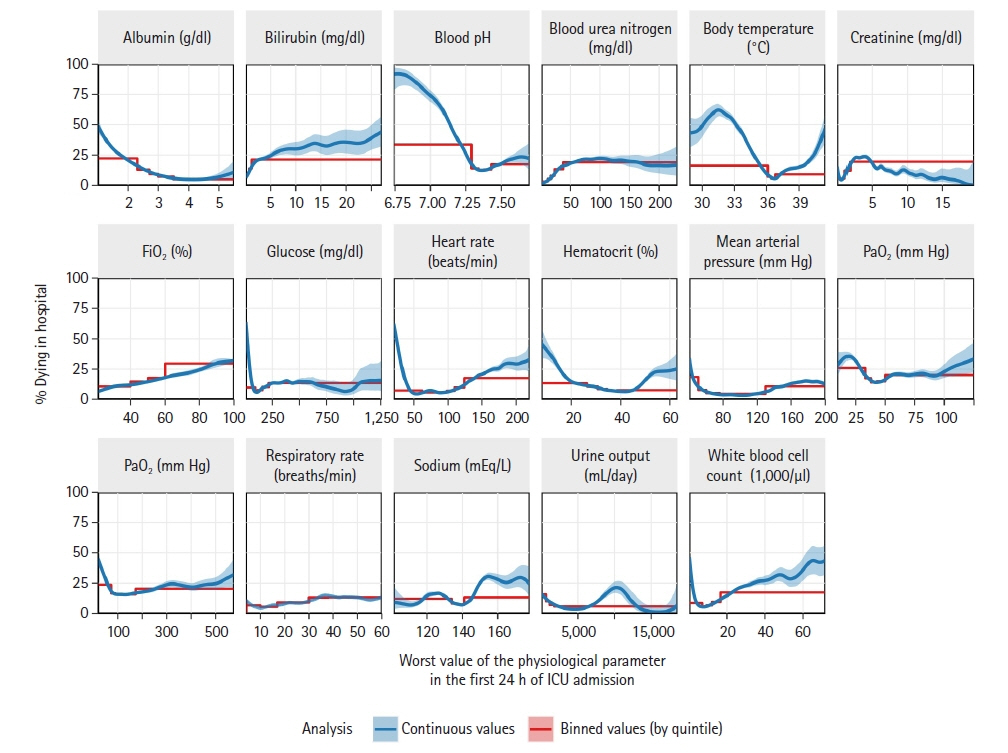
We evaluated relationships of vital signs and laboratory-tested physiological parameters with in-hospital mortality, focusing on values that are unusual or extreme even in critical care settings. Methods: We retrospectively studied Philips Healthcare–MIT eICU data (207 U.S. hospitals, 20142015), including 166,959 adult-patient critical care admissions. Analyzing most-deranged (worst) value measured in the first admission day, we investigated vital signs (body temperature, heart rate, mean arterial pressure, and respiratory rate) as well as albumin, bilirubin, blood pH via arterial blood gas (ABG), blood urea nitrogen, creatinine, FiO2 ABG, glucose, hematocrit, PaO2 ABG, PaCO2 ABG, sodium, 24-hour urine output, and white blood cell count (WBC). Results: In-hospital mortality was ≥50% at extremes of low blood pH, low and high body temperature, low albumin, low glucose, and low heart rate. Near extremes of blood pH, temperature, glucose, heart rate, PaO2 , and WBC, relatively. Small changes in measured values correlated with several-fold mortality rate increases. However, high mortality rates and abrupt mortality increases were often hidden by the common practice of thresholding or binning physiological parameters. The best predictors of in-hospital mortality were blood pH, temperature, and FiO2 (scaled Brier scores: 0.084, 0.063, and 0.049, respectively). Conclusions: In-hospital mortality is high and sharply increasing at extremes of blood pH, body temperature, and other parameters. Common-practice thresholding obscures these associations. In practice, vital signs are sometimes treated more casually than laboratory-tested parameters. Yet, vitals are easier to obtain and we found they are often the best mortality predictors, supporting perspectives that vitals are undervalued.
Figure
Reference
-
1. Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991; 100:1619–36.2. Zimmerman JE, Kramer AA, McNair DS, Malila FM. Acute Physiology and Chronic Health Evaluation (APACHE) IV: hospital mortality assessment for today's critically ill patients. Crit Care Med. 2006; 34:1297–310.
Article3. Higgins TL, Teres D, Copes WS, Nathanson BH, Stark M, Kramer AA. Assessing contemporary intensive care unit outcome: an updated Mortality Probability Admission Model (MPM0-III). Crit Care Med. 2007; 35:827–35.
Article4. Metnitz PG, Moreno RP, Almeida E, Jordan B, Bauer P, Campos RA, et al. SAPS 3: from evaluation of the patient to evaluation of the intensive care unit. Part 1: objectives, methods and cohort description. Intensive Care Med. 2005; 31:1336–44.
Article5. Gerry S, Birks J, Bonnici T, Watkinson PJ, Kirtley S, Collins GS. Early warning scores for detecting deterioration in adult hospital patients: a systematic review protocol. BMJ Open. 2017; 7:e019268.
Article6. Laupland KB, Zahar JR, Adrie C, Schwebel C, Goldgran-Toledano D, Azoulay E, et al. Determinants of temperature abnormalities and influence on outcome of critical illness. Crit Care Med. 2012; 40:145–51.
Article7. Laupland KB, Shahpori R, Kirkpatrick AW, Ross T, Gregson DB, Stelfox HT. Occurrence and outcome of fever in critically ill adults. Crit Care Med. 2008; 36:1531–5.
Article8. Erkens R, Wernly B, Masyuk M, Muessig JM, Franz M, Schulze PC, et al. Admission body temperature in critically ill patients as an independent risk predictor for overall outcome. Med Princ Pract. 2020; 29:389–95.
Article9. Kellett J, Sebat F. Make vital signs great again: a call for action. Eur J Intern Med. 2017; 45:13–9.10. Treacy M, Caroline Stayt L. To identify the factors that influence the recognizing and responding to adult patient deterioration in acute hospitals. J Adv Nurs. 2019; 75:3272–85.
Article11. Stevenson JE, Israelsson J, Petersson G, Bath PA. Factors influencing the quality of vital sign data in electronic health records: a qualitative study. J Clin Nurs. 2018; 27:1276–86.
Article12. Elliott M. The global elements of vital signs' assessment: a guide for clinical practice. Br J Nurs. 2021; 30:956–62.
Article13. Pollard TJ, Johnson AE, Raffa JD, Celi LA, Mark RG, Badawi O. The eICU Collaborative Research Database, a freely available multi-center database for critical care research. Sci Data. 2018; 5:180178.
Article14. McShea M, Holl R, Badawi O, Riker RR, Silfen E. The eICU research institute: a collaboration between industry, health-care providers, and academia. IEEE Eng Med Biol Mag. 2010; 29:18–25.
Article15. MIT Critical Data Group. Secondary analysis of electronic health records. Springer Nature Press;2016.16. Pollard T, Johnson A, Raffa J, Celi LA, Badawi O, Mark R. eICU collaborative research database (version 2.0) [Internet]. PhysioNet;2019. [cited 2024 Feb 20]. Available from: https://physionet.org/content/eicu-crd/2.0/.17. Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, et al. PhysioBank, PhysioToolkit, and PhysioNet: components of a new research resource for complex physiologic signals. Circulation. 2000; 101:E215–20.18. Wood S. Generalized additive models: an introduction with R. Chapman and Hall/CRC;2006.19. Sauerbrei W, Perperoglou A, Schmid M, Abrahamowicz M, Becher H, Binder H, et al. State of the art in selection of variables and functional forms in multivariable analysis-outstanding issues. Diagn Progn Res. 2020; 4:3.
Article20. Wood S. Mixed GAM Computation vehicle with GCV/AIC/REML/NCV smoothness estimation and GAMMs by REML/PQL [Internet]. R Foundation for Statistical Computing; 2017 [cited 2024 Feb 20]. Available from: https://cran.r-project.org/web/packages/mgcv/mgcv.pdf.21. Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010; 21:128–38.22. Quinten VM, van Meurs M, Olgers TJ, Vonk JM, Ligtenberg JJ, Ter Maaten JC. Repeated vital sign measurements in the emergency department predict patient deterioration within 72 hours: a prospective observational study. Scand J Trauma Resusc Emerg Med. 2018; 26:57.
Article23. Candel BG, Duijzer R, Gaakeer MI, Ter Avest E, Sir Ö, Lameijer H, et al. The association between vital signs and clinical outcomes in emergency department patients of different age categories. Emerg Med J. 2022; 39:903–11.
Article24. Hands C, Reid E, Meredith P, Smith GB, Prytherch DR, Schmidt PE, et al. Patterns in the recording of vital signs and early warning scores: compliance with a clinical escalation protocol. BMJ Qual Saf. 2013; 22:719–26.
Article25. Drummond GB, Fischer D, Arvind DK. Current clinical methods of measurement of respiratory rate give imprecise values. ERJ Open Res. 2020; 6:00023–2020.
Article26. Loughlin PC, Sebat F, Kellett JG. Respiratory rate: the forgotten vital sign. Make it count! Jt Comm J Qual Patient Saf. 2018; 44:494–9.27. Elliott M, Williamson R. Is respiratory rate measurement important? An audit of fundamental nursing textbooks. Mediterr Nurs Midwifery. 2022; 1:120–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A deep learning model for estimating sedation levels using heart rate variability and vital signs: a retrospective cross-sectional study at a center in South Korea
- A Machine Learning Approach for Predicting In-Hospital Cardiac Arrest Using Single-Day Vital Signs, Laboratory Test Results, and International Classification of Disease-10 Block for Diagnosis
- Association between persistent tachycardia and tachypnea and in-hospital mortality among non-hypotensive emergency department patients admitted to the hospital
- The Effect of Induction Mode on Various Parameters and Vital Signs during Anesthesia Induction with Propofol Using a Target Contolled Infusion
- The Prognostic Values of Acute Physiological Parameters in Hemorrhagic Stroke Patients: Differences Between Patients with High and Low Glasgow Coma Scale Scores on Admission