Acute Crit Care.
2024 May;39(2):294-303. 10.4266/acc.2023.01130.
Comparison of factors influencing the decision to withdraw life-sustaining treatment in intensive care unit patients after implementation of the Life-Sustaining Treatment Act in Korea
- Affiliations
-
- 1Department of Medical Humanities, Dong-A University College of Medicine, Busan, Korea
- 2Department of Surgery and Critical Care Medicine, Ewha Womans University Seoul Hospital, Seoul, Korea
- 3Department of Surgery, Ewha Womans University College of Medicine, Seoul, Korea
- 4Department of Anesthesia and Pain Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 5Department of Anesthesiology and Pain Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 6Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2557246
- DOI: http://doi.org/10.4266/acc.2023.01130
Abstract
- Background
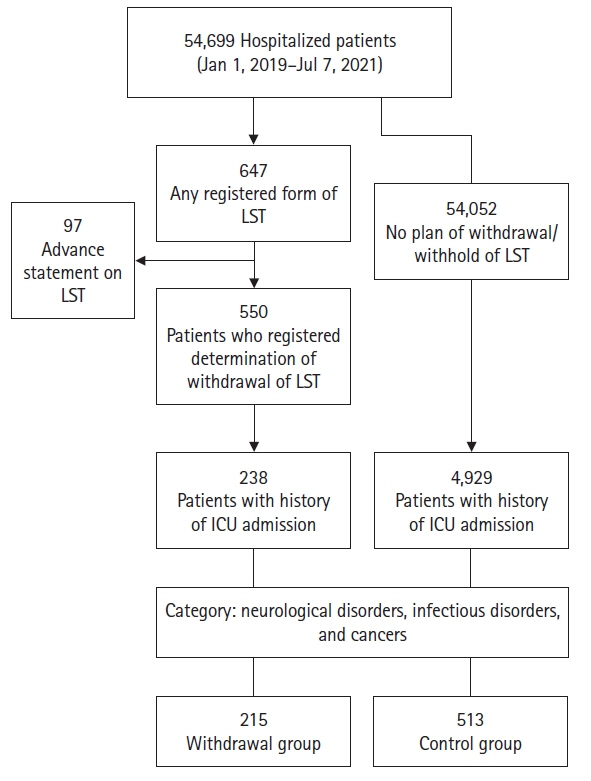
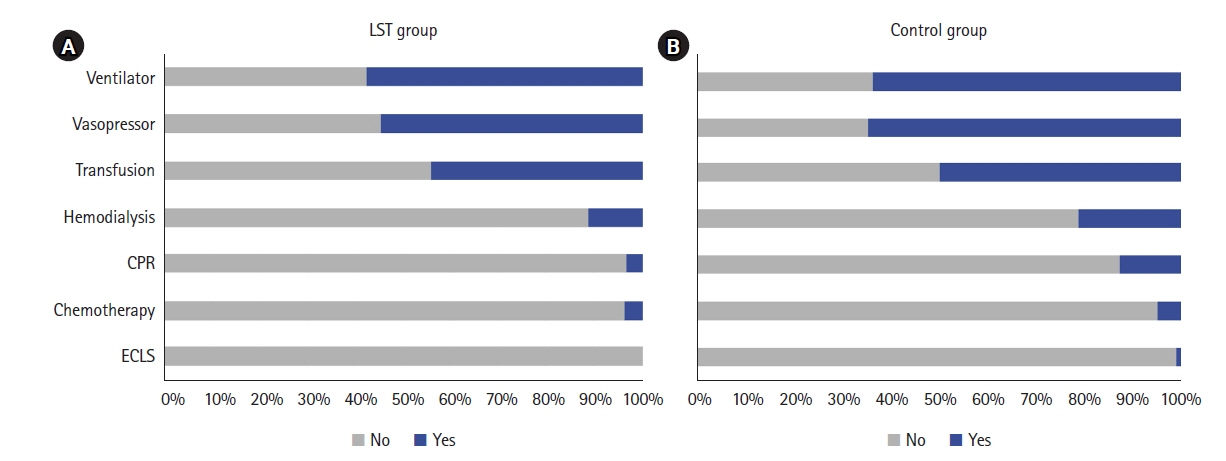
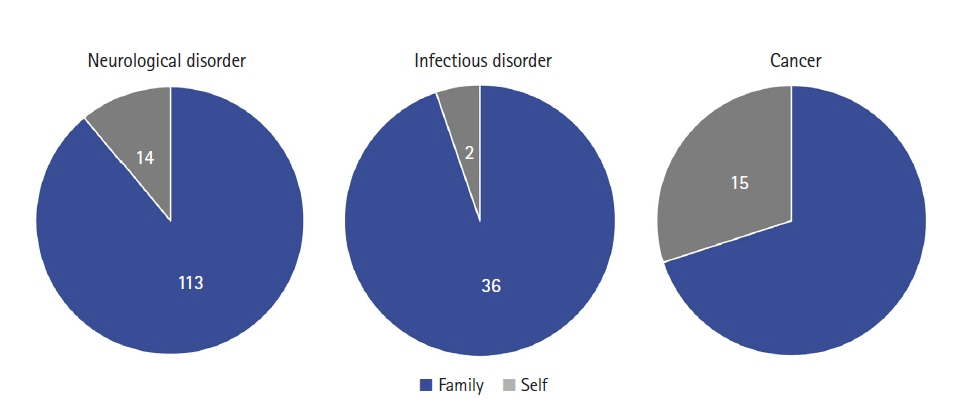
The decision to discontinue intensive care unit (ICU) treatment during the end-oflife stage has recently become a significant concern in Korea, with an observed increase in life-sustaining treatment (LST) withdrawal. There is a growing demand for evidence-based support for patients, families, and clinicians in making LST decisions. This study aimed to identify factors influencing LST decisions in ICU inpatients and to analyze their impact on healthcare utilization. Methods: We retrospectively reviewed medical records of ICU patients with neurological disorders, infectious disorders, or cancer who were treated at a single university hospital between January 1, 2019 and July 7, 2021. Factors influencing the decision to withdraw LST were compared between those who withdrew LST and those who did not. Results: Among 54,699 hospital admissions, LST was withdrawn in 550 cases (1%). Cancer was the most common diagnosis, followed by pneumonia and cerebral infarction. Among ICU inpatients, LST was withdrawn from 215 (withdrawal group). The withdrawal group was older (78 vs. 75 years, P=0.002), had longer total hospital stays (16 vs. 11 days, P<0.001), and higher ICU readmission rates than the control group. There were no significant differences in the healthcare costs of ICU stay between the two groups. Most LST decisions (86%) were made by family. Conclusions: The decisions to withdraw LST of ICU inpatients were influenced by age, readmission, and disease category. ICU costs were similar between the withdrawal and control groups. Further research is needed to tailor LST decisions in the ICU.
Figure
Cited by 1 articles
-
End-of-life care in the intensive care unit: the optimal process of decision to withdrawing life-sustaining treatment based on the Korean medical environment and culture
Ho Jin Yong, Dohhyung Kim
Acute Crit Care. 2024;39(2):321-322. doi: 10.4266/acc.2024.00675.
Reference
-
1. Welfare Ministry of Health and Welfare. Act on decisions on life-sustaining treatment for patients in hospice and palliative care or at the end of life. No. 17218. Welfare Ministry of Health and Welfare;2020.2. Kim HA, Cho M, Son DS. Temporal change in the use of laboratory and imaging tests in one week before death, 2006-2015. J Korean Med Sci. 2023; 38:e98.
Article3. Council on Ethical and Judician Affairs, American Medical Association. Medical futility in end-of-life care: report of the council on ethical and judicial affairs. JAMA. 1999; 281:937–41.4. Curtis JR, Vincent JL. Ethics and end-of-life care for adults in the intensive care unit. Lancet. 2010; 376:1347–53.
Article5. Lee SI, Hong KS, Park J, Lee YJ. Decision-making regarding withdrawal of life-sustaining treatment and the role of intensivists in the intensive care unit: a single-center study. Acute Crit Care. 2020; 35:179–88.
Article6. Park SY, Lee B, Seon JY, Oh IH. A national study of life-sustaining treatments in South Korea: what factors affect decision-making? Cancer Res Treat. 2021; 53:593–600.
Article7. Kim JS, Yoo SH, Choi W, Kim Y, Hong J, Kim MS, et al. Implication of the life-sustaining treatment decisions act on end-of-life care for Korean terminal patients. Cancer Res Treat. 2020; 52:917–24.
Article8. Phua J, Joynt GM, Nishimura M, Deng Y, Myatra SN, Chan YH, et al. Withholding and withdrawal of life-sustaining treatments in intensive care units in Asia. JAMA Intern Med. 2015; 175:363–71.
Article9. Yun YH, Lee CG, Kim SY, Lee SW, Heo DS, Kim JS, Lee KS, Hong YS, et al. The attitudes of cancer patients and their families toward the disclosure of terminal illness. J Clin Oncol. 2004; 22:307–14.
Article10. Manalo MF. End-of-life decisions about withholding or withdrawing therapy: medical, ethical, and religio-cultural considerations. Palliat Care. 2013; 7:1–5.
Article11. Kim H, Im HS, Lee KO, Min YJ, Jo JC, Choi Y, et al. Changes in decision-making process for life-sustaining treatment in patients with advanced cancer after the life-sustaining treatment decisions-making act. BMC Palliat Care. 2021; 20:63.
Article12. Luce JM. End-of-life decision making in the intensive care unit. Am J Respir Crit Care Med. 2010; 182:6–11.
Article13. Yildirim S, Durmaz Y, Şan Y, Taşkıran İ, Cinleti BA, Kirakli C. Cost of chronic critically ill patients to the healthcare system: a single-center experience from a developing country. Indian J Crit Care Med. 2021; 25:519–23.
Article14. Khandelwal N, Benkeser D, Coe NB, Engelberg RA, Teno JM, Curtis JR. Patterns of cost for patients dying in the intensive care unit and implications for cost savings of palliative care interventions. J Palliat Med. 2016; 19:1171–8.
Article15. Slatyer MA, James OF, Moore PG, Leeder SR. Costs, severity of illness and outcome in intensive care. Anaesth Intensive Care. 1986; 14:381–9.
Article16. Kim D, Yoo SH, Seo S, Lee HJ, Kim MS, Shin SJ, et al. Analysis of cancer patient decision-making and health service utilization after enforcement of the life-sustaining treatment decision-making act in Korea. Cancer Res Treat. 2022; 54:20–9.
Article17. Arabi YM, Myatra SN, Lobo SM. Surging ICU during COVID-19 pandemic: an overview. Curr Opin Crit Care. 2022; 28:638–44.
Article18. Lautrette A, Darmon M, Megarbane B, Joly LM, Chevret S, Adrie C, et al. A communication strategy and brochure for relatives of patients dying in the ICU. N Engl J Med. 2007; 356:469–78.
Article19. Ursin LØ. Withholding and withdrawing life-sustaining treatment: ethically equivalent? Am J Bioeth. 2019; 19:10–20.
Article20. Jeong W, Kim S, Kim H, Park EC, Jang SI. Effects of life-sustaining treatment plans on healthcare expenditure and healthcare utilization. BMC Health Serv Res. 2023; 23:1236.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Experience of Life-sustaining Treatment in Patient Care among Intensive Care Unit Nurses: Phenomenological Approach
- Awareness of good death, perception of life-sustaining treatment decision, and changes in nursing activities after decision to discontinue life-sustaining treatment among nurses in intensive care units at tertiary general hospitals
- Decision-making regarding withdrawal of lifesustaining treatment and the role of intensivists in the intensive care unit: a single-center study
- Implementation of Antimicrobial Stewardship Programs in End-of-Life Care
- Association of Physician Orders for Life Sustaining Treatment Completion and Healthcare Utilization before Death