Acute Crit Care.
2024 May;39(2):243-250. 10.4266/acc.2023.01186.
Effects of ketamine on the severity of depression and anxiety following postoperative mechanical ventilation: a single-blind randomized clinical trial in Iran
- Affiliations
-
- 1Department of Anesthesiology and Intensive Care, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
- 2Department of Psychiatry, Faculty of Medicine, Golestan University of Medical Sciences, Gorgan, Iran
- 3Department of Neurological Surgery, Faculty of Medicine, Golestan University of Medical Sciences, Neuroscience Research Center, Gorgan, Iran
- 4Department of Biostatistics and Epidemiology, School of Public Health, Golestan University of Medical Sciences, Gorgan, Iran
- KMID: 2557240
- DOI: http://doi.org/10.4266/acc.2023.01186
Abstract
- Background
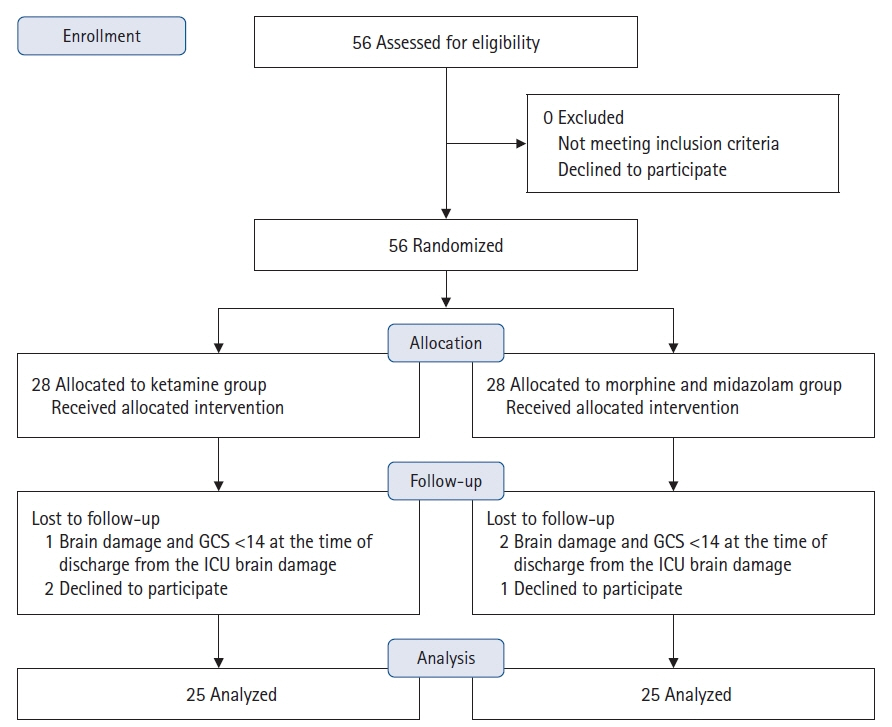
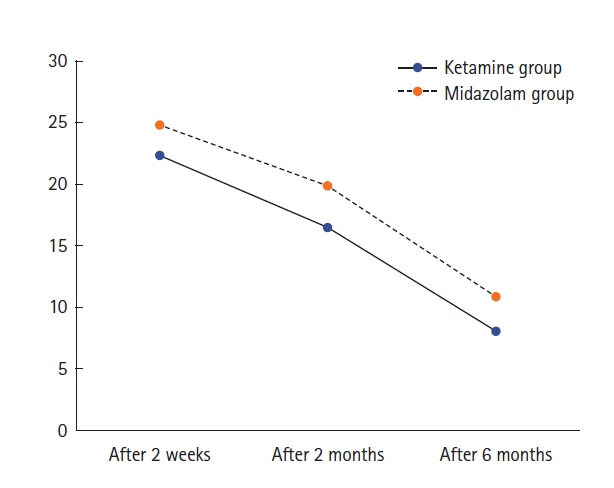
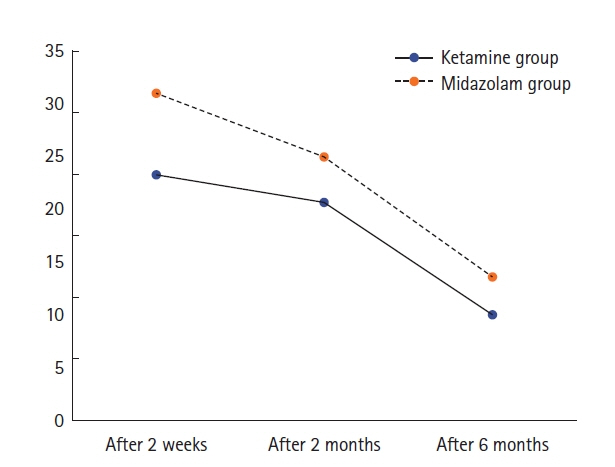
In this study, we compare the effects of ketamine and the combination of midazolam and morphine on the severity of depression and anxiety in mechanically ventilated patients after discharge from the intensive care unit (ICU). Methods: This randomized single-blind clinical trial included 50 patients who were candidates for craniotomy and postoperative mechanical ventilation in the ICU of 5 Azar Teaching Hospital in Gorgan City, North Iran, from 2021 to 2022. Patients were allocated to two groups by quadruple block randomization. In group A, 0.5 mg/kg of ketamine was infused over 15 minutes after craniotomy and then continued at a dose of 5 µ/kg/min during mechanical ventilation. In group B, midazolam was infused at a dose of 2–3 mg/hr and morphine at a dose of 3–5 mg/hr. After patients were discharged from the ICU, if their Glasgow Coma Scale scores were ≥14, Beck’s anxiety and depression inventories were completed by a psychologist within 2 weeks, 2 months, and 6 months after discharge. Results: The mean scores of depression at 2 months (P=0.01) and 6 months (P=0.03) after discharge were significantly lower in the ketamine group than in the midazolam and morphine group. The mean anxiety scores were significantly lower in the ketamine group 2 weeks (P=0.006) and 6 months (P=0.002) after discharge. Conclusions: Ketamine is an effective drug for preventing and treating anxiety and depression over the long term in patients discharged from the ICU. However, further larger volume studies are required to validate these results.
Keyword
Figure
Reference
-
1. Peris A, Bonizzoli M, Iozzelli D, Migliaccio ML, Zagli G, Bacchereti A, et al. Early intra-intensive care unit psychological intervention promotes recovery from post traumatic stress disorders, anxiety and depression symptoms in critically ill patients. Crit Care. 2011; 15:R41.
Article2. Mikkelsen ME, Still M, Anderson BJ, Bienvenu OJ, Brodsky MB, Brummel N, et al. Society of Critical Care Medicine's international consensus conference on prediction and identification of long-term impairments after critical illness. Crit Care Med. 2020; 48:1670–9.
Article3. Egerod I, Risom SS, Thomsen T, Storli SL, Eskerud RS, Holme AN, et al. ICU-recovery in Scandinavia: a comparative study of intensive care follow-up in Denmark, Norway and Sweden. Intensive Crit Care Nurs. 2013; 29:103–11.
Article4. Wu KK, Cho VW, Chow FL, Tsang AP, Tse DM. Posttraumatic stress after treatment in an intensive care unit. East Asian Arch Psychiatry. 2018; 28:39–44.
Article5. Hatch R, Young D, Barber V, Griffiths J, Harrison DA, Watkinson P. Anxiety, depression and post traumatic stress disorder after critical illness: a UK-wide prospective cohort study. Crit Care. 2018; 22:310.
Article6. Davydow DS, Gifford JM, Desai SV, Bienvenu OJ, Needham DM. Depression in general intensive care unit survivors: a systematic review. Intensive Care Med. 2009; 35:796–809.
Article7. Cuthbertson BH, Rattray J, Campbell MK, Gager M, Roughton S, Smith A, et al. The PRaCTICaL study of nurse led, intensive care follow-up programmes for improving long term outcomes from critical illness: a pragmatic randomised controlled trial. BMJ. 2009; 339:b3723.
Article8. Peskett M, Gibb P. Developing and setting up a patient and relatives intensive care support group. Nurs Crit Care. 2009; 14:4–10.
Article9. Vollenweider FX, Leenders KL, Oye I, Hell D, Angst J. Differential psychopathology and patterns of cerebral glucose utilisation produced by (S)- and (R)-ketamine in healthy volunteers using positron emission tomography (PET). Eur Neuropsychopharmacol. 1997; 7:25–38.
Article10. Zhang Z, Zhang WH, Lu YX, Lu BX, Wang YB, Cui LY, et al. Intraoperative low-dose S-ketamine reduces depressive symptoms in patients with Crohn’s disease undergoing bowel resection: a randomized controlled trial. J Clin Med. 2023; 12:1152.
Article11. Gan SL, Long YQ, Wang QY, Feng CD, Lai CX, Liu CT, et al. Effect of esketamine on postoperative depressive symptoms in patients undergoing thoracoscopic lung cancer surgery: a randomized controlled trial. Front Psychiatry. 2023; 14:1128406.
Article12. Hojat M, Shapurian R, Mehryar AH. Psychometric properties of a Persian version of the short form of the Beck Depression Inventory for Iranian college students. Psychol Rep. 1986; 59:331–8.
Article13. Ghassemzadeh H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a Persian-language version of the Beck Depression Inventory: second edition. BDI-II-PERSIAN. Depress Anxiety. 2005; 21:185–92.14. Salari-Moghaddam S, Ranjbar AR, Fathi-Ashtiani A. Validity and reliability measurement of the Persian version of anxiety control questionnaire. J Clin Psych. 2018; 9:33–43.15. Ionescu DF, Bentley KH, Eikermann M, Taylor N, Akeju O, Swee MB, et al. Repeat-dose ketamine augmentation for treatment-resistant depression with chronic suicidal ideation: a randomized, double blind, placebo controlled trial. J Affect Disord. 2019; 243:516–24.
Article16. Zanos P, Gould TD. Mechanisms of ketamine action as an antidepressant. Mol Psychiatry. 2018; 23:801–11.
Article17. Zanos P, Thompson SM, Duman RS, Zarate CA, Gould TD. Convergent mechanisms underlying rapid antidepressant action. CNS Drugs. 2018; 32:197–227.
Article18. Duman RS, Aghajanian GK, Sanacora G, Krystal JH. Synaptic plasticity and depression: new insights from stress and rapid-acting antidepressants. Nat Med. 2016; 22:238–49.
Article19. Deyama S, Duman RS. Neurotrophic mechanisms underlying the rapid and sustained antidepressant actions of ketamine. Pharmacol Biochem Behav. 2020; 188:172837.
Article20. Zarate CA, Brutsche NE, Ibrahim L, Franco-Chaves J, Diazgranados N, Cravchik A, et al. Replication of ketamine's antidepressant efficacy in bipolar depression: a randomized controlled add-on trial. Biol Psychiatry. 2012; 71:939–46.
Article21. Niciu MJ, Luckenbaugh DA, Ionescu DF, Mathews DC, Richards EM, Zarate CA. Subanesthetic dose ketamine does not induce an affective switch in three independent samples of treatment-resistant major depression. Biol Psychiatry. 2013; 74:e23–4.
Article22. Pang L, Cui M, Dai W, Kong J, Chen H, Wu S. Can intraoperative low-dose R, S-ketamine prevent depressive symptoms after surgery? The first meta-analysis of clinical trials. Front Pharmacol. 2020; 11:586104.23. Wang J, Sun Y, Ai P, Cui V, Shi H, An D, et al. The effect of intravenous ketamine on depressive symptoms after surgery: a systematic review. J Clin Anesth. 2022; 77:110631.
Article24. Tully JL, Dahlén AD, Haggarty CJ, Schiöth HB, Brooks S. Ketamine treatment for refractory anxiety: a systematic review. Br J Clin Pharmacol. 2022; 88:4412–26.
Article25. Glue P, Neehoff S, Sabadel A, Broughton L, Le Nedelec M, Shadli S, et al. Effects of ketamine in patients with treatment-refractory generalized anxiety and social anxiety disorders: exploratory double-blind psychoactive-controlled replication study. J Psychopharmacol. 2020; 34:267–72.
Article26. Gommers D, Bakker J. Medications for analgesia and sedation in the intensive care unit: an overview. Crit Care. 2008; 12 Suppl 3(Suppl 3):S4.
Article27. Hsu YH, Lin FS, Yang CC, Lin CP, Hua MS, Sun WZ. Evident cognitive impairments in seemingly recovered patients after midazolam-based light sedation during diagnostic endoscopy. J Formos Med Assoc. 2015; 114:489–97.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Low-dose intravenous ketamine versus intravenous ketorolac in pain control in patients with acute renal colic in an emergency setting: a double-blind randomized clinical trial
- Effect of calcium on premenstrual syndrome: A double-blind randomized clinical trial
- Comparison of low-dose ketamine to methadone for postoperative pain in opioid addicts: a randomized clinical trial
- Subanesthetic intravenous ketamine vs. caudal bupivacaine for postoperative analgesia in children undergoing infra-umbilical surgeries: a non-inferiority randomized, single-blind controlled trial
- Effects of Auricular Acupressure Therapy on Psychological Factors, Sleep Quality, and Salivary Cortisol Levels in South Korean Older Adults in the Community: A Single-blind, Randomized Controlled Trial