Ann Rehabil Med.
2024 Jun;48(3):220-227. 10.5535/arm.230011.
Predictors for Failed Removal of Nasogastric Tube in Patients With Brain Insult
- Affiliations
-
- 1Department of Physical Medicine and Rehabilitation, Lotung Poh-Ai Hospital, Lo-Hsu Foundation, Yilan County, Taiwan (R.O.C.)
- 2Department of Physical Medicine and Rehabilitation, National Taiwan University Hospital, School of Medicine, National Taiwan University, Taipei City, Taiwan (R.O.C.)
- 3Big Data Center, Lotung Poh-Ai Hospital, Lo-Hsu Foundation, Yilan County, Taiwan (R.O.C.)
- KMID: 2557069
- DOI: http://doi.org/10.5535/arm.230011
Abstract
Objective
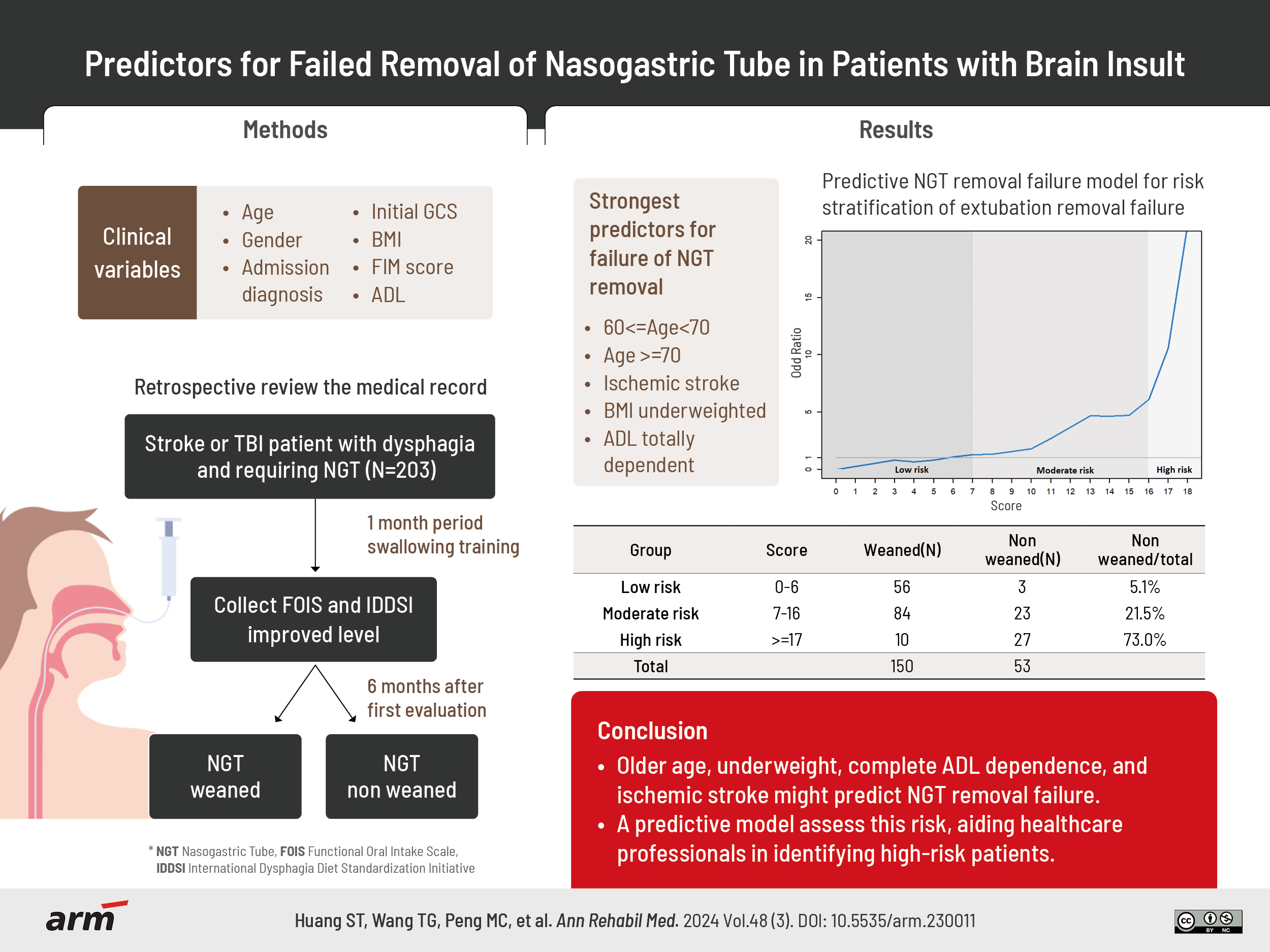
To construct a prognostic model for unsuccessful removal of nasogastric tube (NGT) was the aim of our study.
Methods
This study examined patients with swallowing disorders receiving NGT feeding due to stroke or traumatic brain injury in a regional hospital. Clinical data was collected, such as age, sex, body mass index (BMI), level of activities of daily living (ADLs) dependence. Additionally, gather information regarding the enhancement in Functional Oral Intake Scale (FOIS) levels and the increase in food types according to the International Dysphagia Diet Standardization Initiative (IDDSI) after one month of swallowing training. A stepwise logistic regression analysis model was employed to predict NGT removal failure using these parameters.
Results
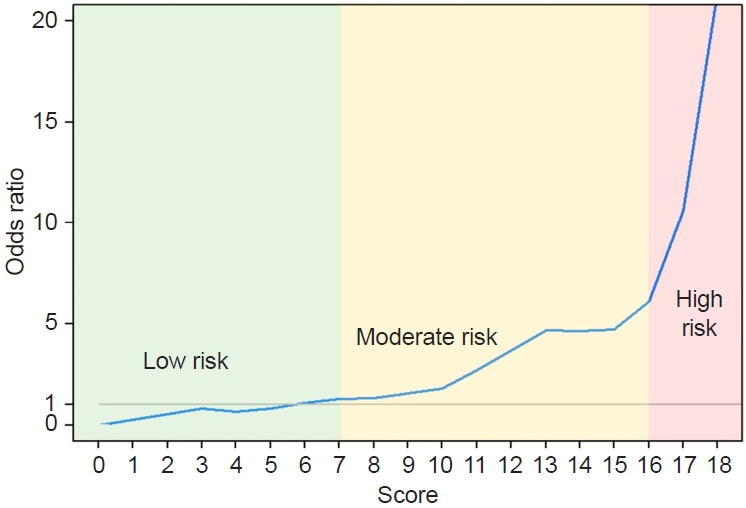
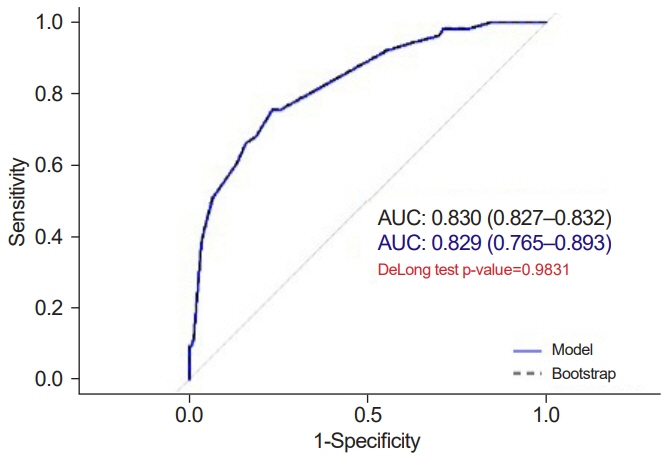
Out of 203 patients, 53 patients (26.1%) had experienced a failed removal of NGT after six months of follow-up. The strongest predictors for failed removal were age over 60 years, underweight BMI, total dependence in ADLs, and ischemic stroke. The admission prediction model categorized patients into high, moderate, and low-risk groups for removal failure. The failure rate of NGT removal was high not only in the high-risk group but also in the moderate-risk groups when there was no improvement in FOIS levels and IDDSI food types.
Conclusion
Our predictive model categorizes patients with brain insults into risk groups for swallowing disorders, enabling advanced interventions such as percutaneous endoscopic gastrostomy for high-risk patients struggling with NGT removal, while follow-up assessments using FOIS and IDDSI aid in guiding rehabilitation decisions for those at moderate risk.
Figure
Reference
-
1. Lee WK, Yeom J, Lee WH, Seo HG, Oh BM, Han TR. Characteristics of dysphagia in severe traumatic brain injury patients: a comparison with stroke patients. Ann Rehabil Med. 2016; 40:432–9.
Article2. Takizawa C, Gemmell E, Kenworthy J, Speyer R. A systematic review of the prevalence of oropharyngeal dysphagia in stroke, Parkinson’s disease, Alzheimer’s disease, head injury, and pneumonia. Dysphagia. 2016; 31:434–41.
Article3. Martino R, Foley N, Bhogal S, Diamant N, Speechley M, Teasell R. Dysphagia after stroke: incidence, diagnosis, and pulmonary complications. Stroke. 2005; 36:2756–63.4. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003; 124:328–36.
Article5. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 2014; 20:7739–51.
Article6. Metheny NA, Meert KL, Clouse RE. Complications related to feeding tube placement. Curr Opin Gastroenterol. 2007; 23:178–82.
Article7. Hsu CY, Lai JN, Kung WM, Hung CH, Yip HT, Chang YC, et al. Nationwide prevalence and outcomes of long-term nasogastric tube placement in adults. Nutrients. 2022; 14:1748.
Article8. Gomes CA Jr, Andriolo RB, Bennett C, Lustosa SA, Matos D, Waisberg DR, et al. Percutaneous endoscopic gastrostomy versus nasogastric tube feeding for adults with swallowing disturbances. Cochrane Database Syst Rev. 2015; 2015:CD008096.9. Ickenstein GW, Höhlig C, Prosiegel M, Koch H, Dziewas R, Bodechtel U, et al. Prediction of outcome in neurogenic oropharyngeal dysphagia within 72 hours of acute stroke. J Stroke Cerebrovasc Dis. 2012; 21:569–76.
Article10. Kumar S, Doughty C, Doros G, Selim M, Lahoti S, Gokhale S, et al. Recovery of swallowing after dysphagic stroke: an analysis of prognostic factors. J Stroke Cerebrovasc Dis. 2014; 23:56–62.
Article11. Mandaville A, Ray A, Robertson H, Foster C, Jesser C. A retrospective review of swallow dysfunction in patients with severe traumatic brain injury. Dysphagia. 2014; 29:310–8.
Article12. Dietrich CG, Schoppmeyer K. Percutaneous endoscopic gastrostomy- too often? Too late? Who are the right patients for gastrostomy? World J Gastroenterol. 2020; 26:2464–71.13. Lin YN, Chen SY, Wang TG, Chang YC, Chie WC, Lien IN. Findings of videofluoroscopic swallowing studies are associated with tube feeding dependency at discharge in stroke patients with dysphagia. Dysphagia. 2005; 20:23–31. Erratum in: Dysphagia 2005;20:388.
Article14. Lee JH, Kim SB, Lee KW, Lee SJ, Park JG, Ri JW. Associating factors regarding nasogastric tube removal in patients with Dysphagia after stroke. Ann Rehabil Med. 2014; 38:6–12.
Article15. Oto T, Kandori Y, Ohta T, Domen K, Koyama T. Predicting the chance of weaning dysphagic stroke patients from enteral nutrition: a multivariate logistic modelling study. Eur J Phys Rehabil Med. 2009; 45:355–62.16. Ikenaga Y, Nakayama S, Taniguchi H, Ohori I, Komatsu N, Nishimura H, et al. Factors predicting recovery of oral intake in stroke survivors with dysphagia in a convalescent rehabilitation ward. J Stroke Cerebrovasc Dis. 2017; 26:1013–9.
Article17. Lee KC, Liu CT, Tzeng IS, Chie WC. Predictors of nasogastric tube removal in patients with stroke and dysphagia. Int J Rehabil Res. 2021; 44:205–8.
Article18. Nakadate A, Otaka Y, Kondo K, Yamamoto R, Matsuura D, Honaga K, et al. Age, body mass index, and white blood cell count predict the resumption of oral intake in subacute stroke patients. J Stroke Cerebrovasc Dis. 2016; 25:2801–8.
Article19. Inooka Y, Yamana H, Shinoda Y, Inokuchi H, Matsui H, Fushimi K, et al. Predictive factors for oral intake recovery after acute stroke: analysis of a Japanese nationwide inpatient database. Dysphagia. 2022; 37:1623–32.
Article20. Muscari A, Falcone R, Pirazzoli E, Faccioli L, Muscari S, Pastore Trossello M, et al. Predicting failure to recover swallowing in patients with severe post-stroke dysphagia: the DIsPHAGIc score. Dysphagia. 2023; 38:290–304.
Article21. Morgan A, Ward E, Murdoch B, Kennedy B, Murison R. Incidence, characteristics, and predictive factors for Dysphagia after pediatric traumatic brain injury. J Head Trauma Rehabil. 2003; 18:239–51.
Article22. Mackay LE, Morgan AS, Bernstein BA. Swallowing disorders in severe brain injury: risk factors affecting return to oral intake. Arch Phys Med Rehabil. 1999; 80:365–71.
Article23. Rhie SH, Choi JW, Jeon SJ, Kang SD, Joo MC, Kim MS. Characteristics of patients with aneurysmal subarachnoid hemorrhage and risk factors related to dysphagia. Ann Rehabil Med. 2016; 40:1024–32.
Article24. Campillo B, Paillaud E, Uzan I, Merlier I, Abdellaoui M, Perennec J, et al. Value of body mass index in the detection of severe malnutrition: influence of the pathology and changes in anthropometric parameters. Clin Nutr. 2004; 23:551–9.
Article25. Curtis M, Swan L, Fox R, Warters A, O’Sullivan M. Associations between body mass index and probable sarcopenia in community-dwelling older adults. Nutrients. 2023; 15:1505.
Article26. Veldee MS, Peth LD. Can protein-calorie malnutrition cause dysphagia? Dysphagia. 1992; 7:86–101.
Article27. Kuroda Y, Kuroda R. Relationship between thinness and swallowing function in Japanese older adults: implications for sarcopenic dysphagia. J Am Geriatr Soc. 2012; 60:1785–6. Erratum in: J Am Geriatr Soc 2012;60:2385.28. Maeda K, Takaki M, Akagi J. Decreased skeletal muscle mass and risk factors of sarcopenic dysphagia: a prospective observational cohort study. J Gerontol A Biol Sci Med Sci. 2017; 72:1290–4.
Article29. Kim Y, Kim CK, Jung S, Yoon BW, Lee SH. Obesity-stroke paradox and initial neurological severity. J Neurol Neurosurg Psychiatry. 2015; 86:743–7.
Article30. Fernández-Pombo A, Seijo-Raposo IM, López-Osorio N, Cantón-Blanco A, González-Rodríguez M, Arias-Rivas S, et al. Lesion location and other predictive factors of dysphagia and its complications in acute stroke. Clin Nutr ESPEN. 2019; 33:178–82.
Article31. Ke Z, Liu W, Chen FY, Ge WY, Li XP, Fan XN, et al. Intracerebral hemorrhage and absence of pneumonia are independent predictors for nasogastric tube removal of post-stroke dysphagia. Ann Indian Acad Neurol. 2023; 26:90–3.
Article32. Paolucci S, Antonucci G, Grasso MG, Bragoni M, Coiro P, De Angelis D, et al. Functional outcome of ischemic and hemorrhagic stroke patients after inpatient rehabilitation: a matched comparison. Stroke. 2003; 34:2861–5.
Article33. Chuang ST, Yen YH, Hsu H, Lai MW, Hung YF, Tsai SW. Predictive factors for nasogastric tube removal in post-stroke patients. Medicina (Kaunas). 2023; 59:368.
Article34. Ikenaga Y, Fudeya M, Kusunoki T, Yamaguchi H. Factors contributing to complete oral intake in dysphagic stroke patients with enteral feeding tubes in convalescent rehabilitation wards. Prog Rehabil Med. 2023; 8:20230011.
Article35. Hansen TS, Engberg AW, Larsen K. Functional oral intake and time to reach unrestricted dieting for patients with traumatic brain injury. Arch Phys Med Rehabil. 2008; 89:1556–62.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Self-Knotting of Nasogastric Tube in a Stroke Patient with Dysphagia: A Case Report
- The Effect of Nasogastric Tube on Swallowing Function in Stroke Patients with Dysphagia
- A Nasogastric Tube Inserted into the Gastrocutaneous Fistula
- Removal of Knotted Nasogastric Tube: A Literature Review and Lessons From Our Case
- Two Cases of Hyperemesis Gravidarum Managed by Enteral Feeding via Nasogastric Tube