Pediatr Emerg Med J.
2024 Jul;11(3):122-128. 10.22470/pemj.2023.00892.
Clinical features and use of renal replacement therapy in children who visit the emergency department with benign acute childhood myositis or rhabdomyolysis who visit the emergency department
- Affiliations
-
- 1Department of Emergency Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2557050
- DOI: http://doi.org/10.22470/pemj.2023.00892
Abstract
- Purpose
This study was performed to analyze clinical features and use of renal replacement therapy (RRT) for children who visit the pediatric emergency department with benign acute childhood myositis (BACM) or rhabdomyolysis.
Methods
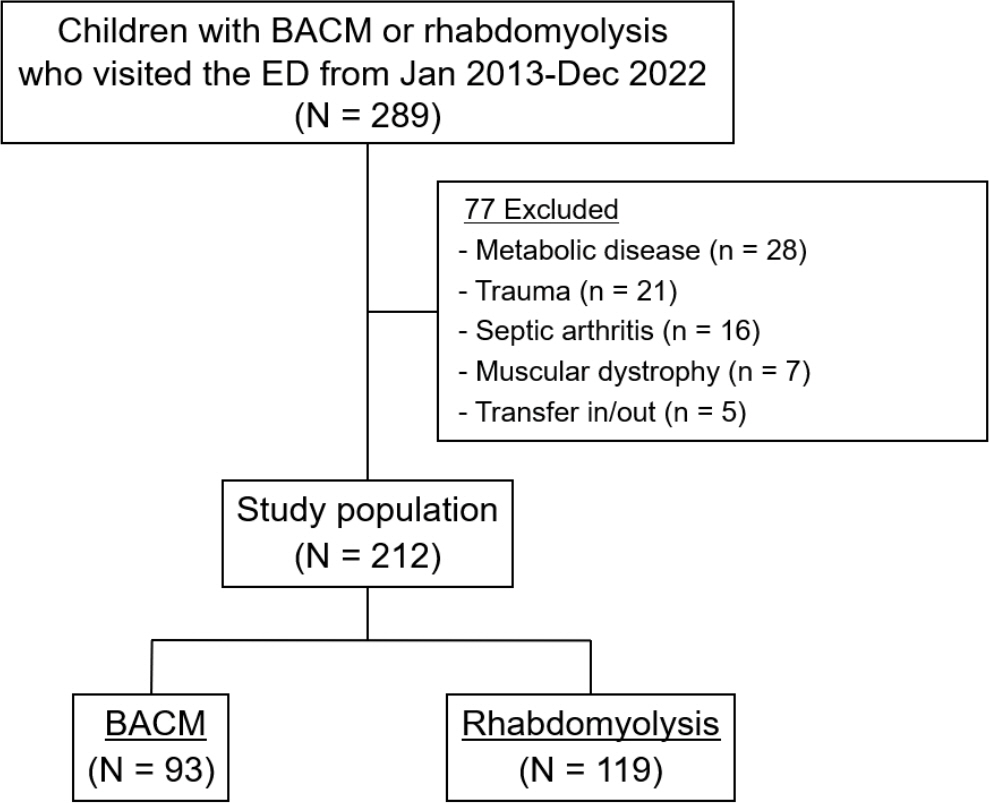
We retrospectively reviewed medical records of 289 children who visited the emergency department with BACM or rhabdomyolysis from January 2013 through December 2022. Clinical features, laboratory and microbiological findings, and outcomes were compared between children with the two diagnoses. Subsequently, multivariable logistic regressions were performed to identify factors associated with applying RRT.
Results
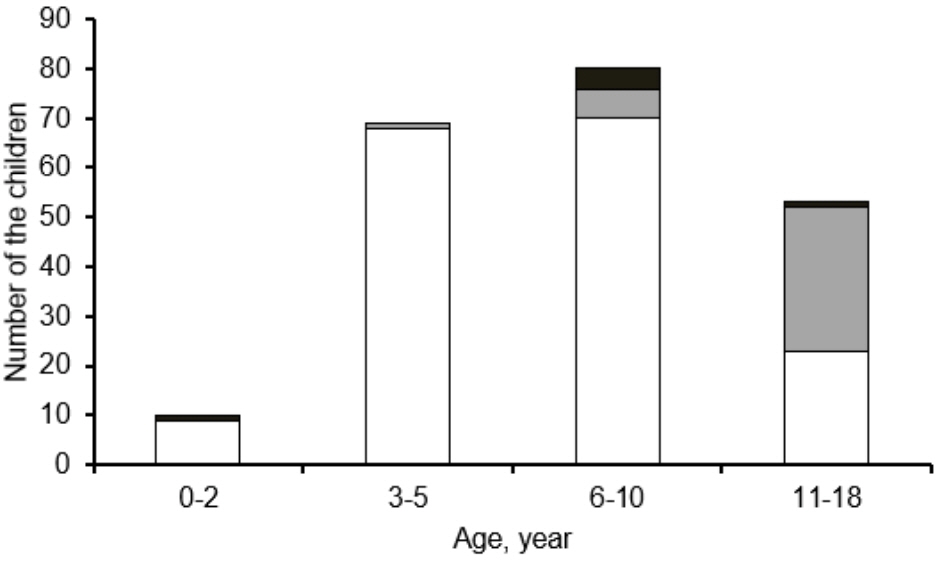
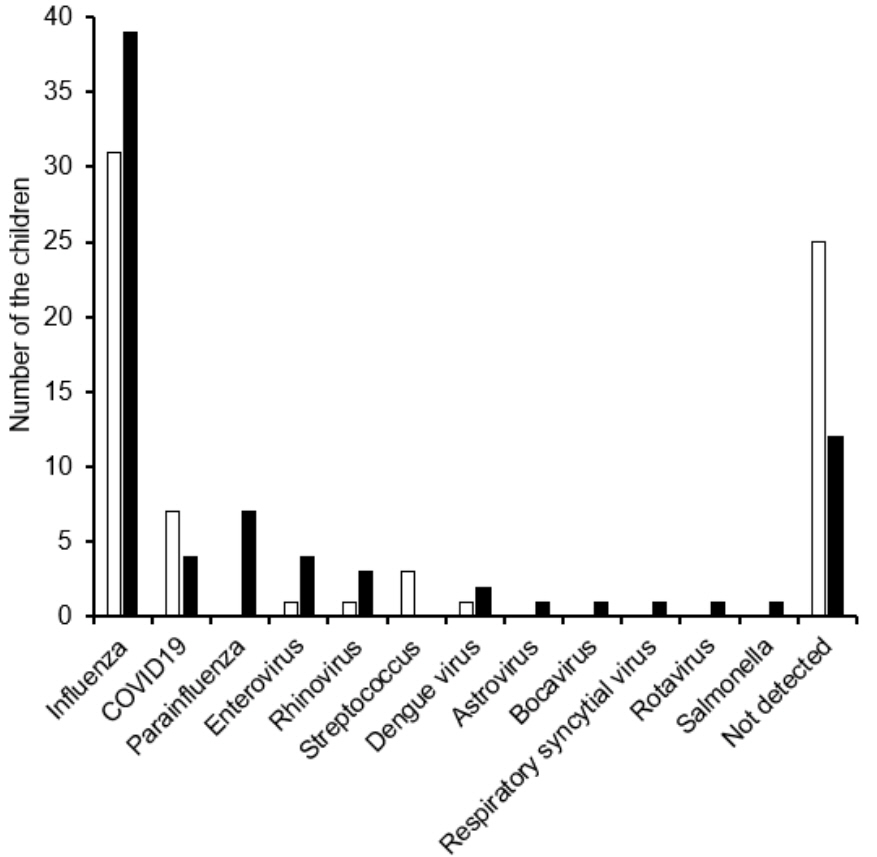
Of the 289 children, a total of 212 were analyzed, including 93 with BACM and 119 with rhabdomyolysis. Influenza (70 of the 145 children [48.3%]) was the most common cause, followed by exercise (36 of 212 [17.0%]). Compared with the children with BACM, those with rhabdomyolysis showed significantly higher frequencies of being boys and hematuria, and higher concentrations of hemoglobin, creatinine, creatine kinase, and myoglobin. Continuous venovenous hemofiltration, a modality of RRT, was applied to 8 children (6.7%) with rhabdomyolysis, of whom 1 died. Creatine kinase was independently associated with the application of RRT (adjusted odds ratio, 1.06; 95% confidence interval, 1.00-1.12; P = 0.036).
Conclusion
Rhabdomyolysis in children who require RRT may be associated with a higher concentration of creatine kinase.
Keyword
Figure
Reference
-
References
1. Costa Azevedo A, Costa E Silva A, Juliana Silva C, Poço Miranda S, Costa M, Martinho I. Benign acute childhood myositis: a 5-year retrospective study. Arch Pediatr. 2022; 29:490–3.
Article2. Brisca G, Mariani M, Pirlo D, Romanengo M, Pistorio A, Gaiero A, et al. Management and outcome of benign acute childhood myositis in pediatric emergency department. Ital J Pediatr. 2021; 47:57.
Article3. Szugye HS. Pediatric rhabdomyolysis. Pediatr Rev. 2020; 41:265–75.
Article4. Harmer MJ, Nijloveanu V, Thodi E, Ding WY, Longthorpe C, Fenton-Jones M, et al. Paediatric rhabdomyolysis: A UK centre's 10-year retrospective experience. J Paediatr Child Health. 2023; 59:346–51.5. Ozawa H, Noma S, Nonaka I. Myositis and rhabdomyolysis with influenza infection. Nihon Rinsho. 2000; 58:2276–81.6. Mannix R, Tan ML, Wright R, Baskin M. Acute pediatric rhabdomyolysis: causes and rates of renal failure. Pediatrics. 2006; 118:2119–25.
Article7. Agharokh L, Zaniletti I, Yu AG, Lee BC, Hall M, Williams DJ, et al. Trends in pediatric rhabdomyolysis and associated renal failure: a 10-year population-based study. Hosp Pediatr. 2022; 12:718–25.
Article8. Kuok CI, Chan WK. Acute kidney injury in pediatric non-traumatic rhabdomyolysis. Pediatr Nephrol. 2021; 36:3251–7.
Article9. Lim YS, Cho H, Lee ST, Lee Y. Acute kidney injury in pediatric patients with rhabdomyolysis. Korean J Pediatr. 2018; 61:95–100.
Article10. Gardner HM, Askenazi DJ, Hoefert JA, Helton A, Wu CL. Acute kidney injury among children admitted with viral rhabdomyolysis. Hosp Pediatr. 2021; 11:878–85.
Article11. Chavez LO, Leon M, Einav S, Varon J. Beyond muscle destruction: a systematic review of rhabdomyolysis for clinical practice. Crit Care. 2016; 20:135.
Article12. Kerr J, Macartney K, Britton PN. Influenza-associated myositis: a single-centre, 5-year retrospective study. Eur J Pediatr. 2021; 180:577–84.
Article13. Garg RK, Malhotra HS, Jain A, Malhotra KP. Dengue-associated neuromuscular complications. Neurol India. 2015; 63:497–516.
Article14. Park IH, Kim YA, Shin SY, Park YS, Yoon HJ, Kim CO, et al. A case of dengue fever complicated by rhabdomyolysis. Infect Chemother. 2005; 37:234–6. Korean.15. Gelbart B, DeMarco R, David Hussey A, Namachivayam SP, McRae R, Quinlan C, et al. Rhabdomyolysis in a tertiary PICU: a 10-year study. Pediatr Crit Care Med. 2018; 19:e51–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rhabdomyolysis after Lamotrigine Poisoning: A Case report
- Survival after Cardiac Arrest due to Acute Methamphetamine Poisoning: A Case Report
- Hyperkalemia in a patient with rhabdomyolysis and compartment syndrome: A case report
- Utilization characteristics of an advanced pediatric emergency center: a single center study over 2 years
- Risk factors for acute bronchiolitis-related return visits to the emergency department