Pediatr Emerg Med J.
2024 Jul;11(3):115-121. 10.22470/pemj.2024.00969.
Changes in the characteristics of pediatric emergency practice following the introduction of pediatric specialist care
- Affiliations
-
- 1Department of Emergency Medicine, Chungbuk National University Hospital, Cheongju, Republic of Korea
- KMID: 2557049
- DOI: http://doi.org/10.22470/pemj.2024.00969
Abstract
- Purpose
We aimed to evaluate whether pediatric emergency practice has improved since the introduction of pediatric specialist care (PSC).
Methods
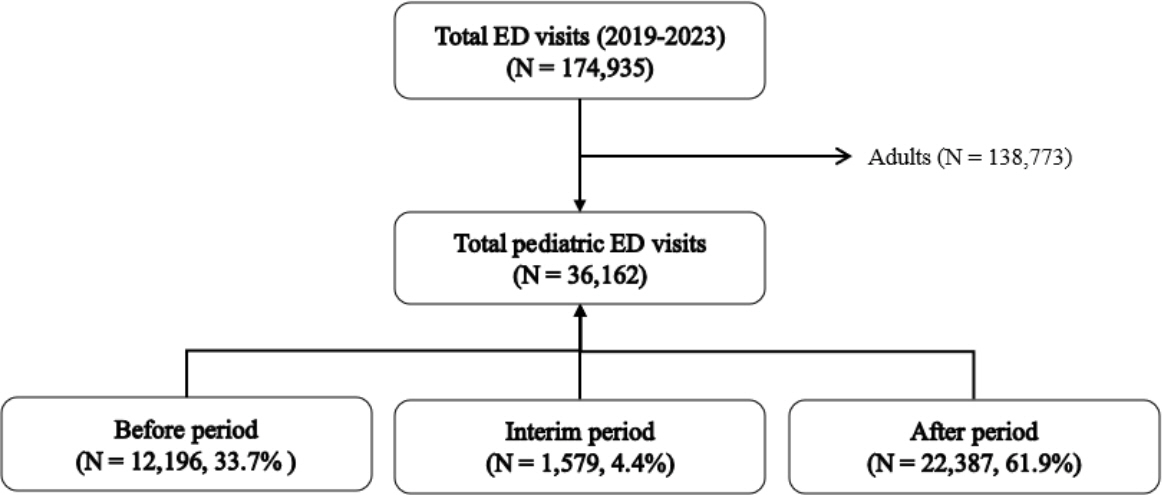
Retrospective observational study was conducted using the data retrieved from the emergency department (ED) of a tertiary university hospital in Cheongju, Korea. Patients younger than 19 years who visited the ED from January 2019 through December 2023 were enrolled in this study. Hospitalization (overall and intensive care unit [ICU]), in-hospital mortality, and return visit within 24 hours were compared between the periods before (January 2019-January 2021) and after (June 2021-December 2023) the introduction of PSC. Adjusted odds ratios with 95% confidence intervals were calculated for the outcomes using multivariable logistic regression.
Results
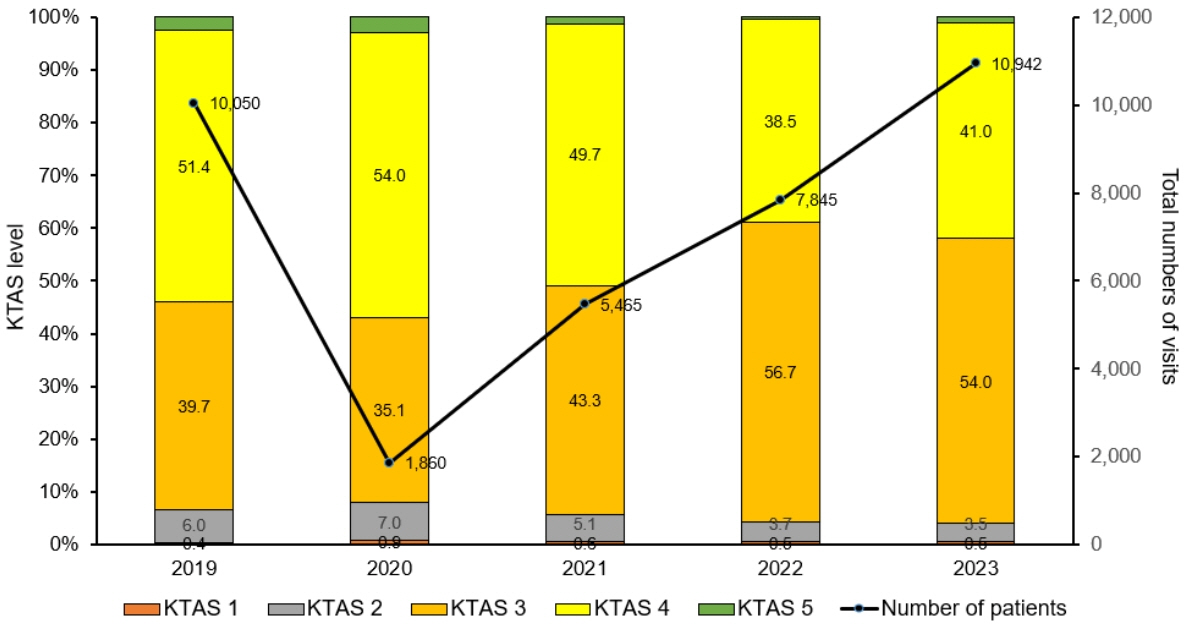
During the study period, a total of 36,162 patients visited the ED. The visits increased from 12,196 before to 22,387 after the introduction of PSC (increase by 83.6%). Annual numbers of the visits have increased since 2020 and reached 10,942 in 2023. After the introduction of PSC, decreases were noted in the hospitalization (adjusted odds ratio, 0.67; 95% confidence interval, 0.62-0.72) and return visit within 24 hours (0.73; 0.61-0.88). Hospitalization to the ICU increased (2.90; 2.29-3.69), while there was no significant difference in the in-hospital mortality (1.31; 0.77-2.25).
Conclusion
After the introduction of PSC, overall hospitalization and return visit decreased, while hospitalization to the ICU increased without a difference in the in-hospital mortality. Multidisciplinary efforts are needed to continue providing the pediatric specialist-centered emergency practice.
Figure
Reference
-
References
1. Statistics Korea. Child population statistics [Internet]. Statistics Korea; c2024 [cited 2024 Mar 8]. Available from: https://www.index.go.kr/unity/potal/main/EachDtlPageDetail.do?idx_cd=3053. Korean.2. National Emergency Medical Center. 2022 The 21st National Emergency Medical Care annual report [Internet]. National Emergency Medical Statistics; c2024 [cited 2024 Mar 8]. Available from: https://www.e-gen.or.kr/nemc/statistics_annual_report.do. Korean.3. Bennett CL, Espinola JA, Sullivan AF, Boggs KM, Clay CE, Lee MO, et al. Evaluation of the 2020 pediatric emergency physician workforce in the US. JAMA Netw Open. 2021; 4:e2110084.
Article4. Kim DK, Kwak YH, Lee SJ, Jung JY, Song BK, Lee JH, et al. A national survey of current practice patterns and preparedness of pediatric emergency care in Korea. J Korean Soc Emerg Med. 2012; 23:126–31. Korean.5. Kim J. An experience of operating the pediatric emergency room. Soonchunhyang Med Sci. 2012; 18:43–7. Korean.
Article6. Huang IA, Tuan PL, Jaing TH, Wu CT, Chao M, Wang HH, et al. Comparisons between full-time and part-time pediatric emergency physicians in pediatric emergency department. Pediatr Neonatol. 2016; 57:371–7.7. Spaite DW, Bartholomeaux F, Guisto J, Lindberg E, Hull B, Eyherabide A, et al. Rapid process redesign in a university-based emergency department: decreasing waiting time intervals and improving patient satisfaction. Ann Emerg Med. 2002; 39:168–77.
Article8. Ryu JH, Min MK, Lee DS, Yeom SR, Lee SH, Wang IJ, et al. Changes in relative importance of the 5-level triage system, Korean Triage and Acuity Scale, for the disposition of emergency patients induced by forced reduction in its level number: a multi-center registry-based retrospective cohort study. J Korean Med Sci. 2019; 34:e114.
Article9. Statistics Kora. The 8th Korean standard classification of disease and cause of death (KCD-8) [Internet]. Statistics Korea; c2021 [cited 2024 Mar 8]. Available from: https://www.koicd.kr/kcd/kcd.do?degree=08. Korean.10. Noh H, Kim DK, Lee SH, Kwak YH, Jung JH, Jang HY, et al. Comparisons of pediatric patients who visited to the pediatric emergency department and the general emergency department. Pediatr Emerg Med J. 2015; 2:29–34. Korean.
Article11. Weiner SG, Ruffing RP, Barnewolt BA. A comparison of resource utilization between emergency physicians and pediatric emergency physicians. Pediatr Emerg Care. 2012; 28:869–72.
Article12. Kwak YH, Park JD. Background and necessity of implementing the subspecialty of pediatric emergency medicine in Korea. Pediatr Emerg Med J. 2020; 7:57–60. Korean.
Article13. Shin S, Choi H, Choi B. Utilization characteristics of an advanced pediatric emergency center: a single center study over 2 years. Pediatr Emerg Med J. 2020; 7:16–22. Korean.
Article14. Je S, Hong JS, Lee JS. A plan for strengthening pediatric emergency care: establishment of pediatric certified emergency center. Pediatr Emerg Med J. 2017; 4:46–50. Korean.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Regionalization of pediatric emergency care in Korea
- The degree of Satisfaction with Nursing Care of Pediatric patients visiting Emergency Center
- A plan for strengthening pediatric emergency care: establishment of pediatric certified emergency center
- An Experience of Operating the Pediatric Emergency Room
- An Analysis of Pediatric Emergency Nursing Practice and Nursing Competence among Emergency Department Nurses