J Cerebrovasc Endovasc Neurosurg.
2024 Jun;26(2):204-209. 10.7461/jcen.2023.E2023.10.002.
Delayed fatal rupture of vertebral artery after treated with flow-diverter in fibromuscular dysplasia patient: A case report and review of the literature
- Affiliations
-
- 1Department of Neurosurgery, Institute of Wonkwang Medical Science, Wonkwang University School of Medicine, Iksan, Korea
- KMID: 2556983
- DOI: http://doi.org/10.7461/jcen.2023.E2023.10.002
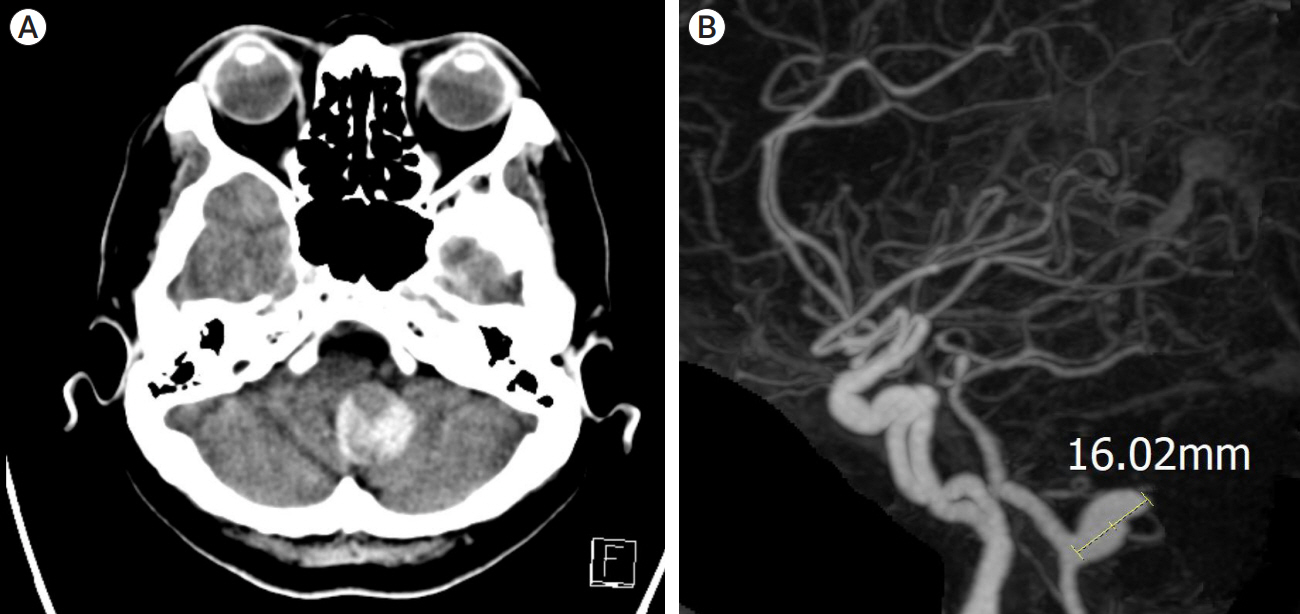
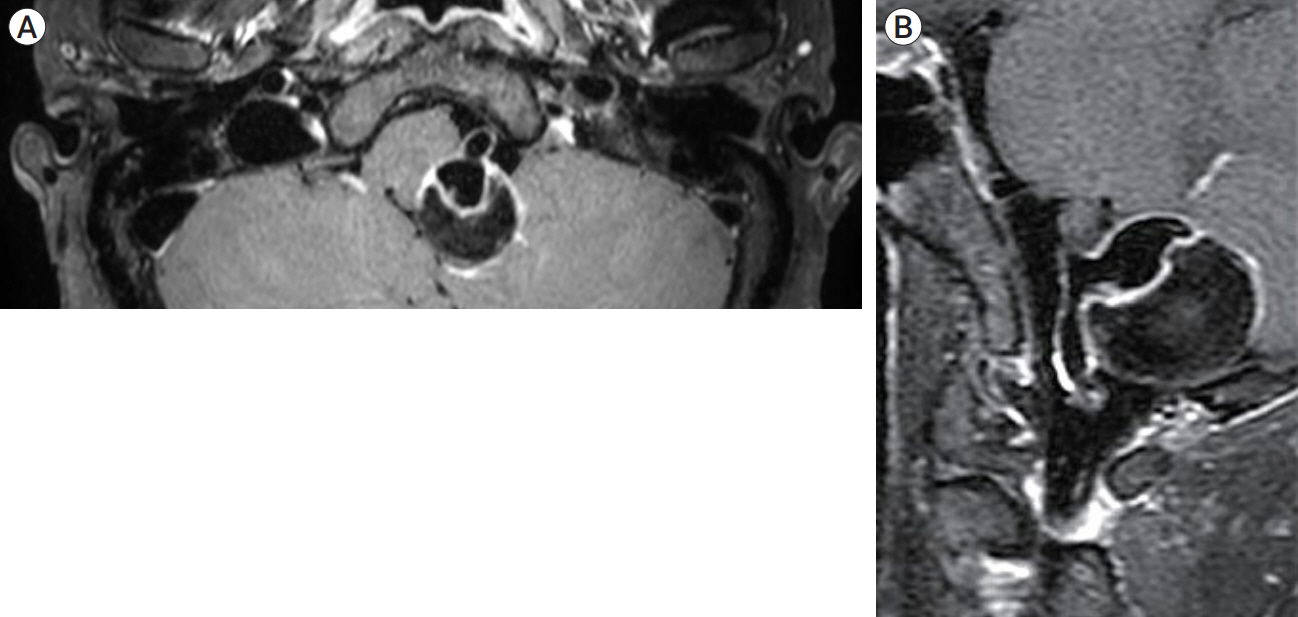
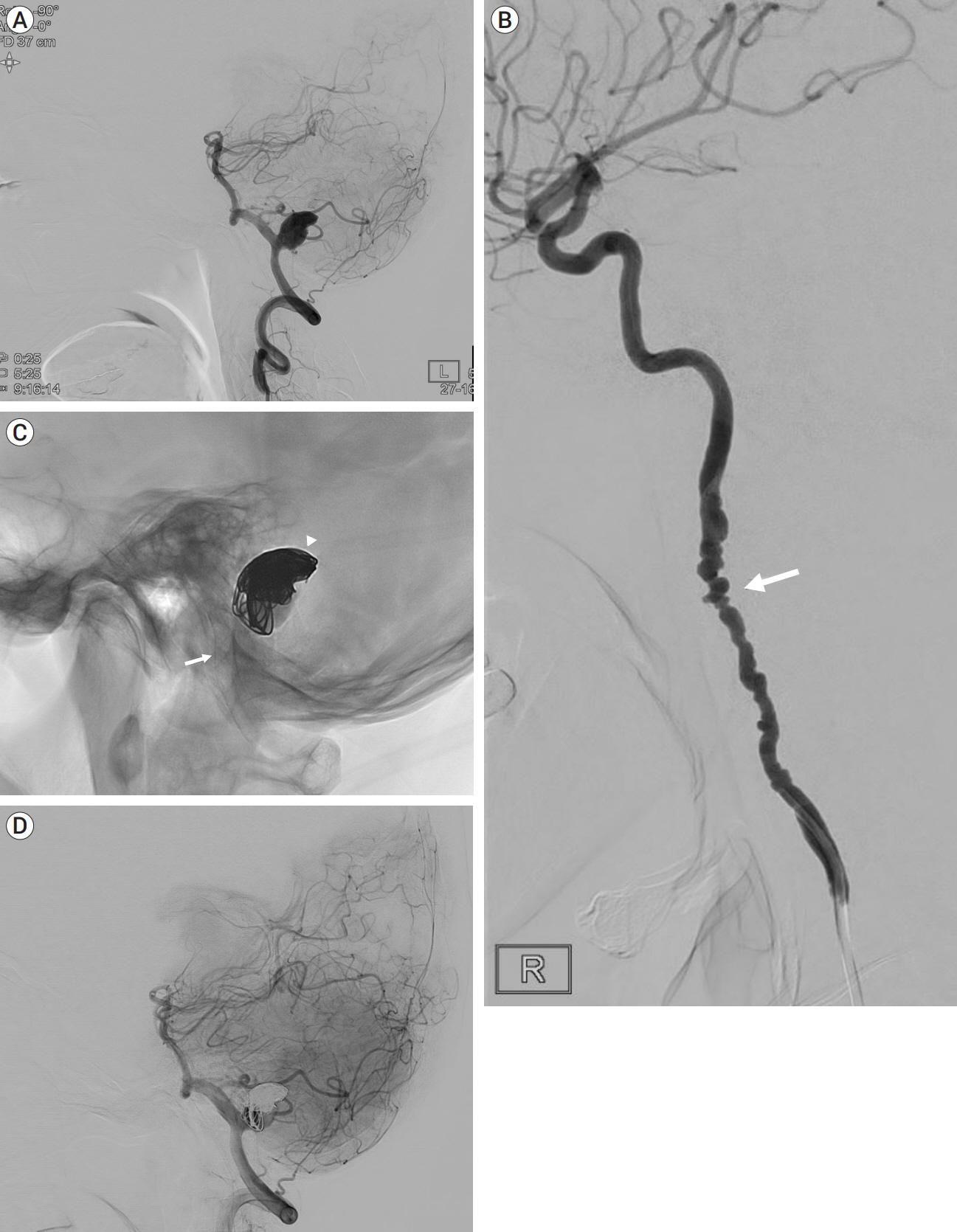
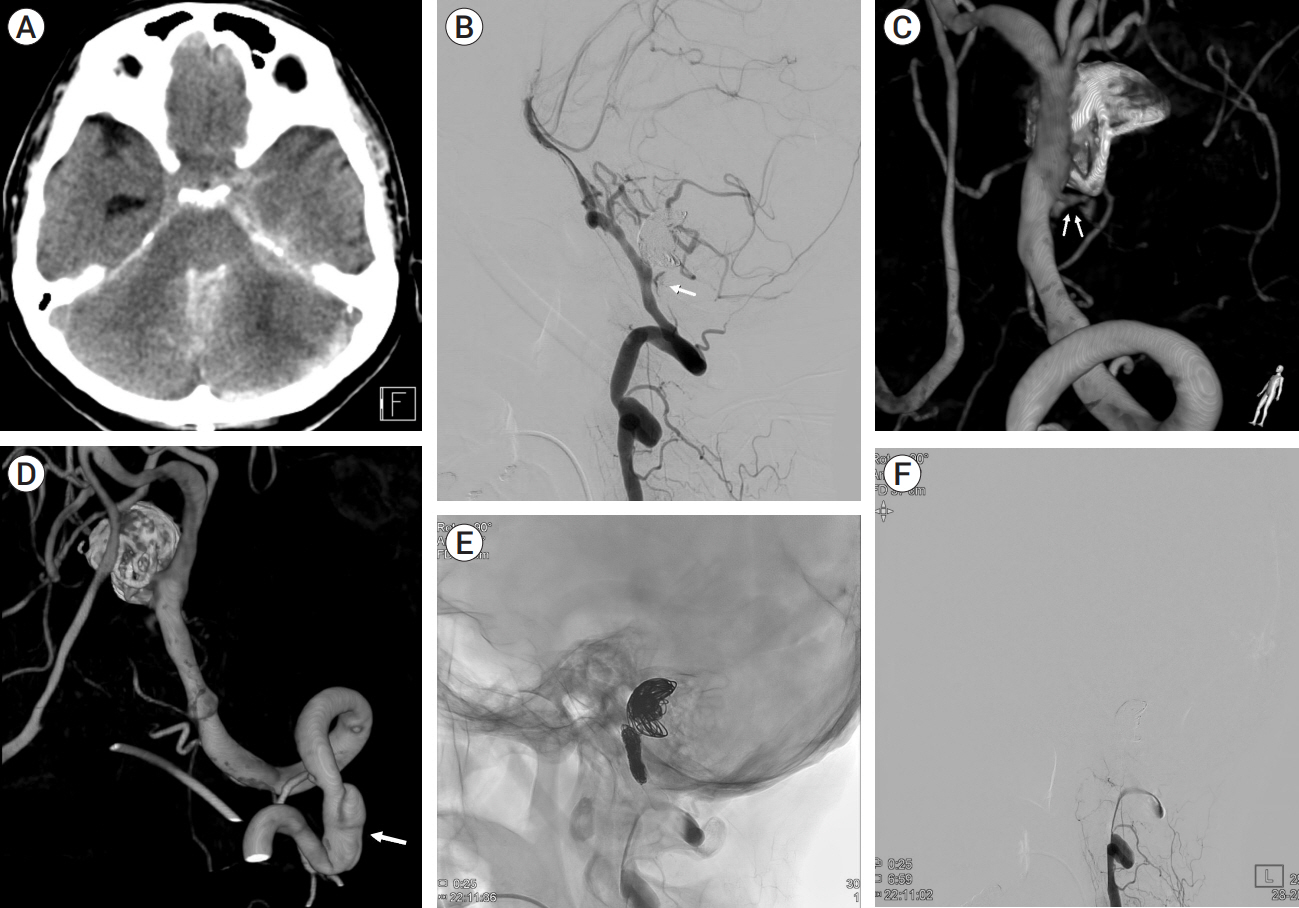
Abstract
- Fibromuscular dysplasia (FMD) is a noninflammatory arterial diseases that affects predominantly women. Multiple studies have demonstrated an increased prevalence of FMD in patients who experience carotid or vertebral artery dissection (VAD). This case report presents a 57-year-old female who presented with a headache and was diagnosed with partially thrombosed giant aneurysm of vertebral artery. This aneurysm was successfully treated with flow-diverter and coil, but new onset rupture of vertebral artery was detected two weeks later, leading to internal trapping. This case report underscores the need for awareness and understanding of treatment of dissection and aneurysm in patient who is suspected FMD
Keyword
Figure
Reference
-
1. De Bray JM, Marc G, Pautot V, Vielle B, Pasco A, Lhoste P, et al. Fibromuscular dysplasia may herald symptomatic recurrence of cervical artery dissection. Cerebrovasc Dis. 2007; 23(5-6):448–52.
Article2. Iihara K, Sakai N, Murao K, Sakai H, Higashi T, Kogure S, et al. Dissecting aneurysms of the vertebral artery: A management strategy. J Neurosurg. 2002; Aug. 97(2):259–67.
Article3. Jin SC, Kwon DH, Choi CG, Ahn JS, Kwun BD. Endovascular strategies for vertebrobasilar dissecting aneurysms. AJNR Am J Neuroradiol. 2009; Sep. 30(8):1518–23.
Article4. Kesav P, Manesh Raj D, John S. Cerebrovascular fibromuscular dysplasia – A practical review. Vasc Health Risk Manag. 2023; Aug. 19:543–56.
Article5. Lather HD, Gornik HL, Olin JW, Gu X, Heidt ST, et al. Prevalence of intracranial aneurysm in women with fibromuscular dysplasia: A report from the US registry for fibromuscular dysplasia. JAMA Neurol. 2017; Sep. 74(9):1081–7.
Article6. Li H, Li XF, Zhang X, He XY, Duan CZ, Liu YC. Treatment of unruptured vertebral dissecting aneurysms: internal trapping or stent-assisted coiling. Int J Neurosci. 2016; 126(3):243–8.
Article7. Mehta B, Burke T, Kole M, Bydon A, Seyfried D, Malik G. Stent-within-a-stent technique for the treatment of dissecting vertebral artery aneurysms. AJNR Am J Neuroradiol. 2003; Oct. 24(9):1814–8.8. Narata AP, Yilmaz H, Schaller K, Lovblad KO, Pereira VM. Flow-diverting stent for ruptured intracranial dissecting aneurysm of vertebral artery. Neurosurgery. 2012; Apr. 70(4):982–8.
Article9. Olin JW, Gornik HL, Bacharach JM, Biller J, Fine LJ, Gray BH, et al. Fibromuscular dysplasia: State of the science and critical unanswered questions: A scientific statement from the american heart association. Circulation. 2014; Mar. 129(9):1048–78.
Article10. Talarowska P, Dobrowolski P, Klisiewicz A, Kostera-Pruszczyk A, Członkowska A, Kurkowska-Jastrzębska I, et al. High incidence and clinical characteristics of fibromuscular dysplasia in patients with spontaneous cervical artery dissection: The ARCADIA-POL study. Vasc Med. 2019; Apr. 24(2):112–9.
Article11. Touzé E, Oppenheim C, Trystram D, Nokam G, Pasquini M, Alamowitch S, et al. Fibromuscular dysplasia of cervical and intracranial arteries. Int J stroke. 2010; Aug. 5(4):296–305.
Article12. Zhao KJ, Zhao R, Huang QH, Xu Y, Hong B, Fang YB, et al. The interaction between stent(s) implantation, PICA involvement, and immediate occlusion degree affect symptomatic intracranial spontaneous vertebral artery dissection aneurysm (sis-VADA) recurrence after reconstructive treatment with Stent(s)-Assisted Coiling. Eur Radiol. 2014; Sep. 24(9):2088–96.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypoplasia of Left Vertebral Artery with Intimal Fibromuscular Dysplasia in a Korean Woman
- Delayed Proximal Flow Diverting Stent Migration in a Ruptured Intracranial Aneurysm: A Case Report
- Kinking of Flow Diverter in a Giant Wide-Necked Supraclinoid Internal Carotid Artery Aneurysm
- Symptomatic Post Endarterectomy Common Carotid Artery Pseudoaneurysm Treated with Combination of Flow Diverter Implantation and Carotid Stenting
- A Case of Pseudoaneurysm of the Common Carotid Artery Associated with Central Venous Catheterization in a Patient on Hemodialysis