J Cerebrovasc Endovasc Neurosurg.
2024 Jun;26(2):196-203. 10.7461/jcen.2023.E2023.07.003.
Various treatment modalities for isolated intracranial middle cerebral arterial dissection with progressive ischemic symptoms: 2 case reports of endovascular stent and bypass surgery
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Neurological Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea
- KMID: 2556982
- DOI: http://doi.org/10.7461/jcen.2023.E2023.07.003
Abstract
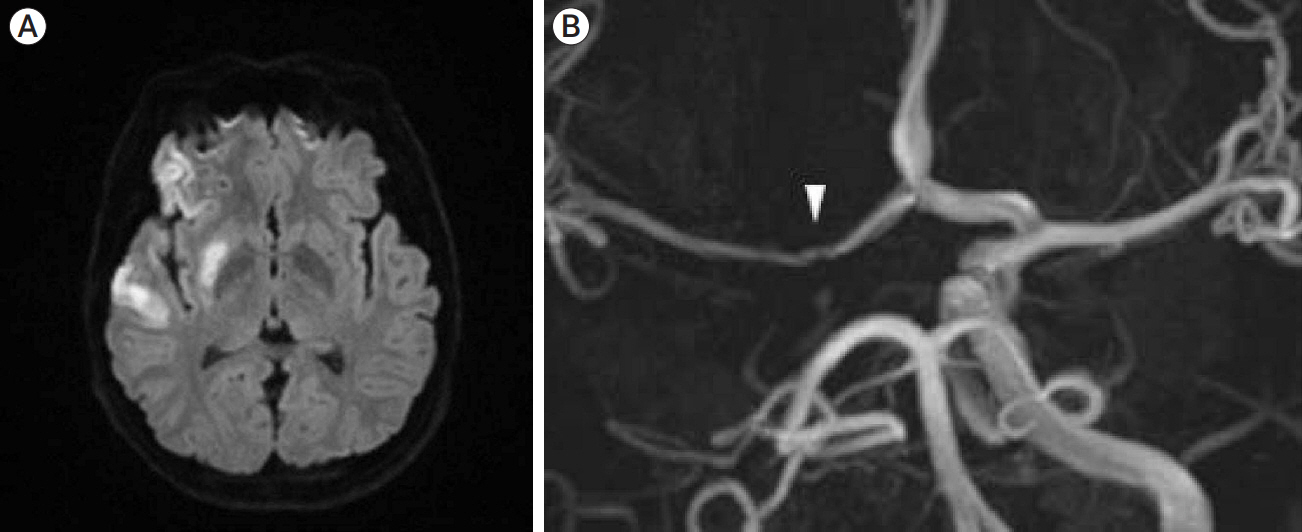
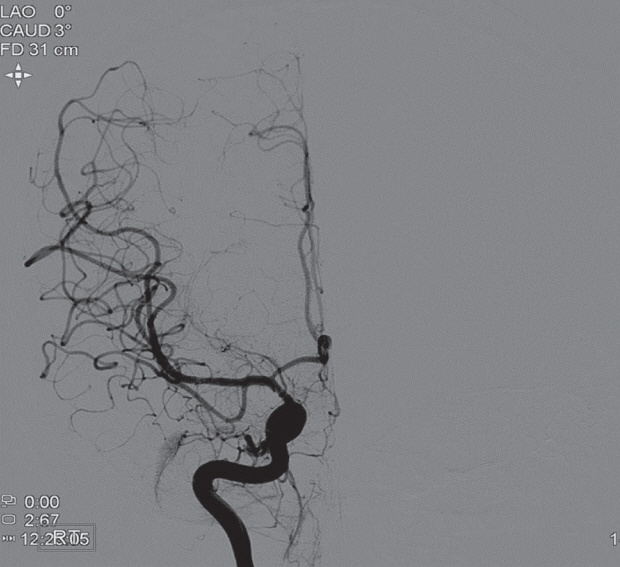
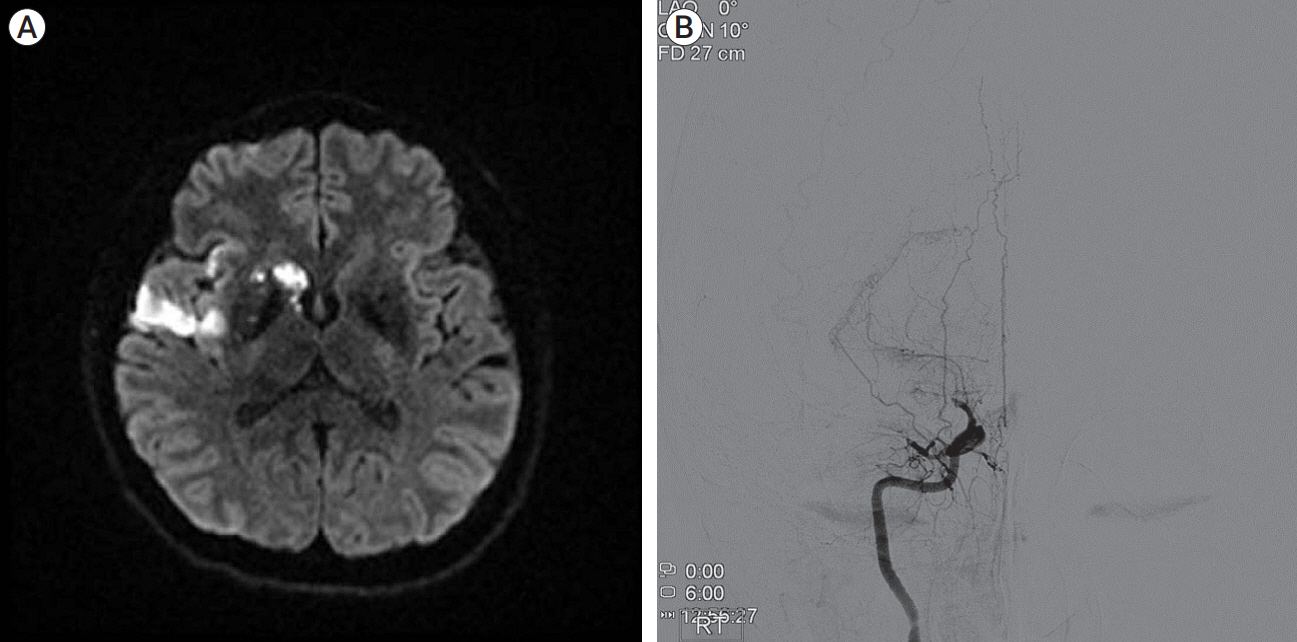
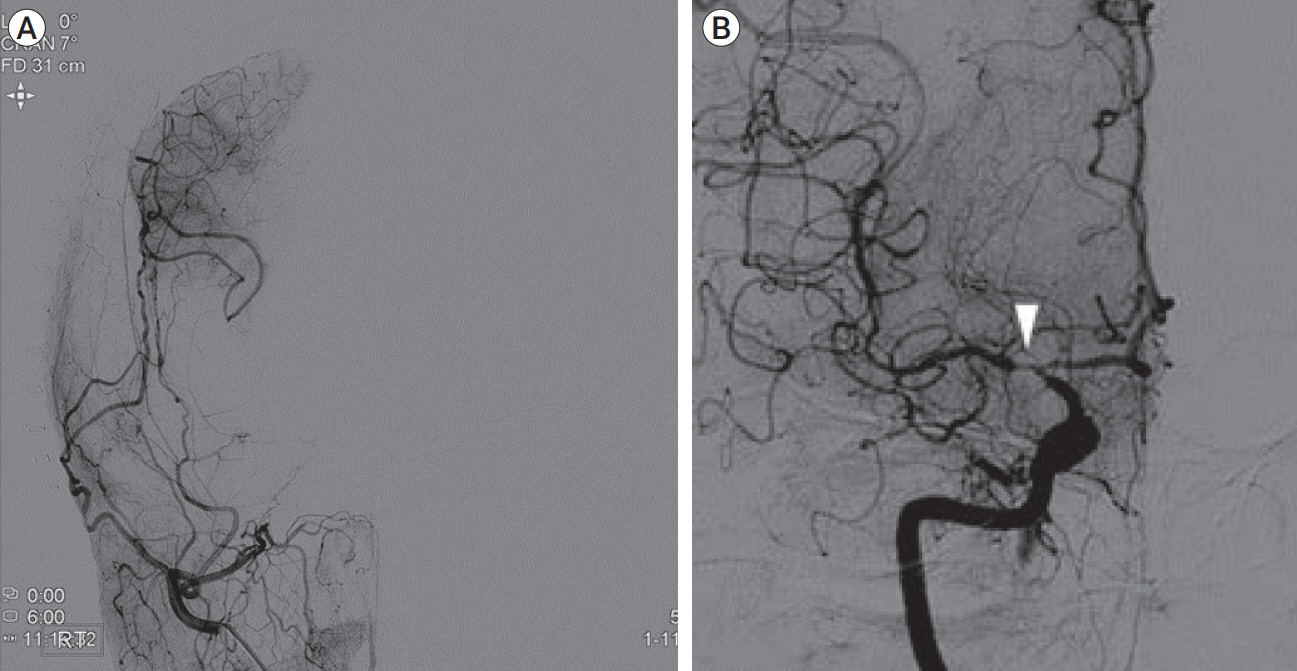
- Isolated middle cerebral artery dissection (MCAD) is rare but increasingly recognized as a significant clinical entity, particularly in younger adults. Ischemic stroke is the most common manifestation in symptomatic cases but symptoms can vary in severity from headaches to severe neurologic deficits. Due to its rarity and unpredictable clinical course, there is no established treatment strategy for isolated MCAD. Through two case reports, we reviewed the post-operative clinical course of MCAD under different treatment modalities. Case 1 was a 21-year-old woman who presented to the emergency department with headaches and left-side hemiparesis. Isolated MCAD was diagnosed and she was successfully treated with the placement of a self-expandable stent and subsequent chemical angioplasty for post-stent vasospasm. Case 2 was a 35-year-old woman who presented to the emergency department with left-side hemiparesis and dysarthria. Isolated MCAD was diagnosed and she was successfully treated with superficial temporal artery (STA) to middle cerebral artery (MCA) anastomosis.
Figure
Reference
-
1. Amlie-Lefond C, Bernard TJ, Sebire G, Friedman NR, Heyer GL, Lerner NB, et al. Predictors of cerebral arteriopathy in children with arterial ischemic stroke: Results of the International Pediatric Stroke Study. Circulation. 2009; Mar. 119(10):1417–23.
Article2. Bernava G, Meling TR, Rosi A, Hofmeister J, Yilmaz H, Brina O, et al. Acute stenting and concomitant tirofiban administration for the endovascular treatment of acute ischemic stroke related to intracranial artery dissections: A single center experience and systematic review of the literature. J Stroke Cerebrovasc Dis. 2021; Aug. 30(8):105891.
Article3. Caplan LR. Dissections of brain-supplying arteries. Nat Clin Pract Neurol. 2008; Jan. 4(1):34–42.
Article4. Debette S, Compter A, Labeyrie MA, Uyttenboogaart M, Metso TM, Majersik JJ, et al. Epidemiology, pathophysiology, diagnosis, and management of intracranial artery dissection. Lancet Neurol. 2015; Jun. 14(6):640–54.
Article5. Debette S, Grond-Ginsbach C, Bodenant M, Kloss M, Engelter S, Metso T, et al. Differential features of carotid and vertebral artery dissections: The CADISP study. Neurology. 2011; Sep. 77(12):1174–81.
Article6. Debette S, Mazighi M, Bijlenga P, Pezzini A, Koga M, Bersano A, et al. ESO guideline for the management of extracranial and intracranial artery dissection. Eur Stroke J. 2021; Sep. 6(3):XXXIX–LXXXVIII.
Article7. Ikota M, Kusaka G, Tanaka Y. Superficial temporal artery-middle cerebral artery anastomosis for ischemic stroke due to dissection of the intracranial internal carotid artery with middle cerebral artery extension. NMC Case Rep J. 2018; Mar. 5(2):39–44.
Article8. Jang IK, Lewis BE, Matthai WH Jr, Kleiman NS. Argatroban anticoagulation in conjunction with glycoprotein IIb/IIIa inhibition in patients undergoing percutaneous coronary intervention: An open-label, nonrandomized pilot study. J Thromb Thrombolysis. 2004; Aug. 18(1):31–7.
Article9. Kim DJ, Kim BM, Suh SH, Kim DI. Self-expanding stent placement for anterior circulation intracranial artery dissection presenting with ischemic symptoms. Neurosurgery. 2015; Feb. 76(2):158–64. discussion 64.
Article10. Kitani R, Itouji T, Noda Y, Kimura M, Uchida S. Dissecting aneurysms of the anterior circle of Willis arteries. Report of two cases. J Neurosurg. 1987; Aug. 67(2):296–300.11. Malek AM, Higashida RT, Phatouros CC, Lempert TE, Meyers PM, Smith WS, et al. Endovascular management of extracranial carotid artery dissection achieved using stent angioplasty. AJNR Am J Neuroradiol. 2000; Aug. 21(7):1280–92.12. Markus HS, Levi C, King A, Madigan J, Norris J. Antiplatelet therapy vs anticoagulation therapy in cervical artery dissection: The Cervical Artery Dissection in Stroke Study (CADISS) randomized clinical trial final results. JAMA Neurol. 2019; Jun. 76(6):657–64.
Article13. Metso TM, Metso AJ, Helenius J, Haapaniemi E, Salonen O, Porras M, et al. Prognosis and safety of anticoagulation in intracranial artery dissections in adults. Stroke. 2007; Jun. 38(6):1837–42.
Article14. Ogiwara H, Maeda K, Hara T, Kimura T, Abe H. Spontaneous intracranial internal carotid artery dissection treated by intra-arterial thrombolysis and superficial temporal artery-middle cerebral artery anastomosis in the acute stage-- Case report. Neurol Med Chir (Tokyo). 2005; Mar. 45(3):148–51.15. Oka F, Shimizu H, Matsumoto Y, Watanabe M, Tominaga T. Ischemic stroke due to dissection of intracranial internal carotid artery: Implications for early surgical treatment. Surg Neurol. 2008; Jun. 69(6):578–84. discussion 584-5.
Article16. Ono H, Inoue T, Suematsu S, Tanishima T, Tamura A, Saito I, et al. Middle cerebral artery dissection causing subarachnoid hemorrhage and cerebral infarction: Trapping with high-flow bypass preserving the lenticulostriate artery. Surg Neurol Int. 2017; Jul. 8:157.
Article17. Park-Matsumoto YC, Tazawa T. Transcranial bypass for spontaneous intracranial carotid artery dissection--A case report. Angiology. 2000; Apr. 51(4):335–40. discussion 340-1.18. Putaala J, Metso AJ, Metso TM, Konkola N, Kraemer Y, Haapaniemi E, et al. Analysis of 1008 consecutive patients aged 15 to 49 with first-ever ischemic stroke: The Helsinki young stroke registry. Stroke. 2009; Apr. 40(4):1195–203.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intracranial Atherosclerotic Disease; Current Options for Surgical or Medical Treatment
- Intracranial Cerebrovascular Revascularization(Extracranial-Intracranial Arterial Bypass, EIAB)
- STA-Distal ACA Bypass Using a Contralateral STA Interposition Graft for Symptomatic ACA Stenosis
- A Case of Complete Resolution of Aortic Dissection in the Descending Thoracic Aorta Treated with Endovascular Stent-Graft Implantation
- Stenting of Symptomatic Middle Cerebral Artery Stenosis: Case Report