Korean J healthc assoc Infect Control Prev.
2024 Jun;29(1):40-47. 10.14192/kjicp.2024.29.1.40.
Korean National Healthcare-associated Infections Surveillance System for Hand Hygiene Report: Data Summary from July 2019 to December 2022
- Affiliations
-
- 1Infection Control Office, Korea University Guro Hospital, Seoul, Korea
- 2Department of Nursing Science, Sun Moon University, Asan, Korea
- 3Department of Infection Control, Severance Hospital, Seoul, Korea
- 4Department of Infection Control, Gangnam Severance Hospital, Seoul, Korea
- 5Department of Nursing Science, Gangseo University, Seoul, Korea
- 6Office of Infection Control, Ewha Womans University College of Medicine Seoul Hospital, Seoul, Korea
- 7Office for Infection Control, Asan Medical Center, Seoul, Korea
- 8Infection Control Team, Seoul National University Bundang Hospital, Seongnam, Korea
- 9Infection Control Department, Wonkwang University Hospital, Iksan, Korea
- 10Infection Control Office, Korea University Anam Hospital, Seoul, Korea
- 11Infection Control Team, Hanyang University Hospital, Seoul, Korea
- 12Center for Infection Prevention and Control, Samsung Medical Center, Seoul, Korea
- 13Infection Control Team, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 14College of Nursing, Keimyung University, Daegu, Korea
- 15Infection Control Team, Chung-Ang University Hospital, Seoul, Korea
- 16Infection Control Team, Dankook University Hospital, Cheonan, Korea
- 17Infection Prevention & Control Team, Soon Chun Hyang University Hospital Bucheon, Bucheon, Korea
- KMID: 2556879
- DOI: http://doi.org/10.14192/kjicp.2024.29.1.40
Abstract
- Background
Hand hygiene is considered the simplest and most cost-effective method of infection prevention. Regular observation and feedback on hand hygiene compliance are key strategies for its enhancement. This study evaluated the effectiveness of hand hygiene surveillance, including direct observation and feedback, by comprehensively analyzing the reported hand hygiene compliance within the Korean National Healthcare-Associated Infections Surveillance System from 2019 to 2022.
Methods
Participating medical institutions included general hospitals and hospitals with infection control departments that consented to participate. Hand hygiene surveillance was conducted using direct observation. Collected data, including healthcare workers, clinical areas, hand hygiene moments, and hand hygiene compliance, were recorded to calculate hand hygiene compliance rates. Additionally, the volume of alcohol-based hand sanitizers used per patient per day was investigated as an indirect indicator of hand hygiene compliance. The study was conducted from July 2019 to December 2022.
Results
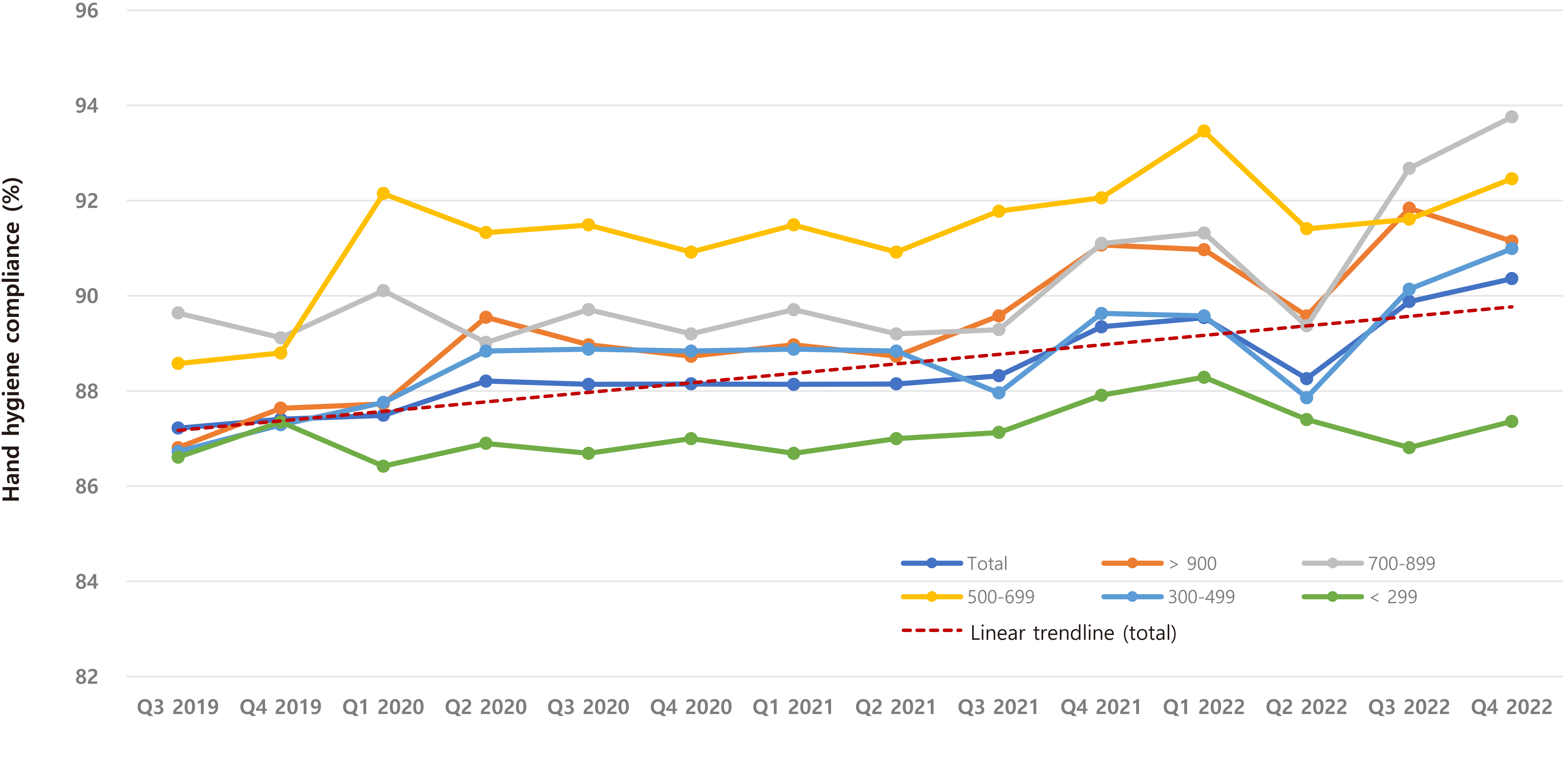
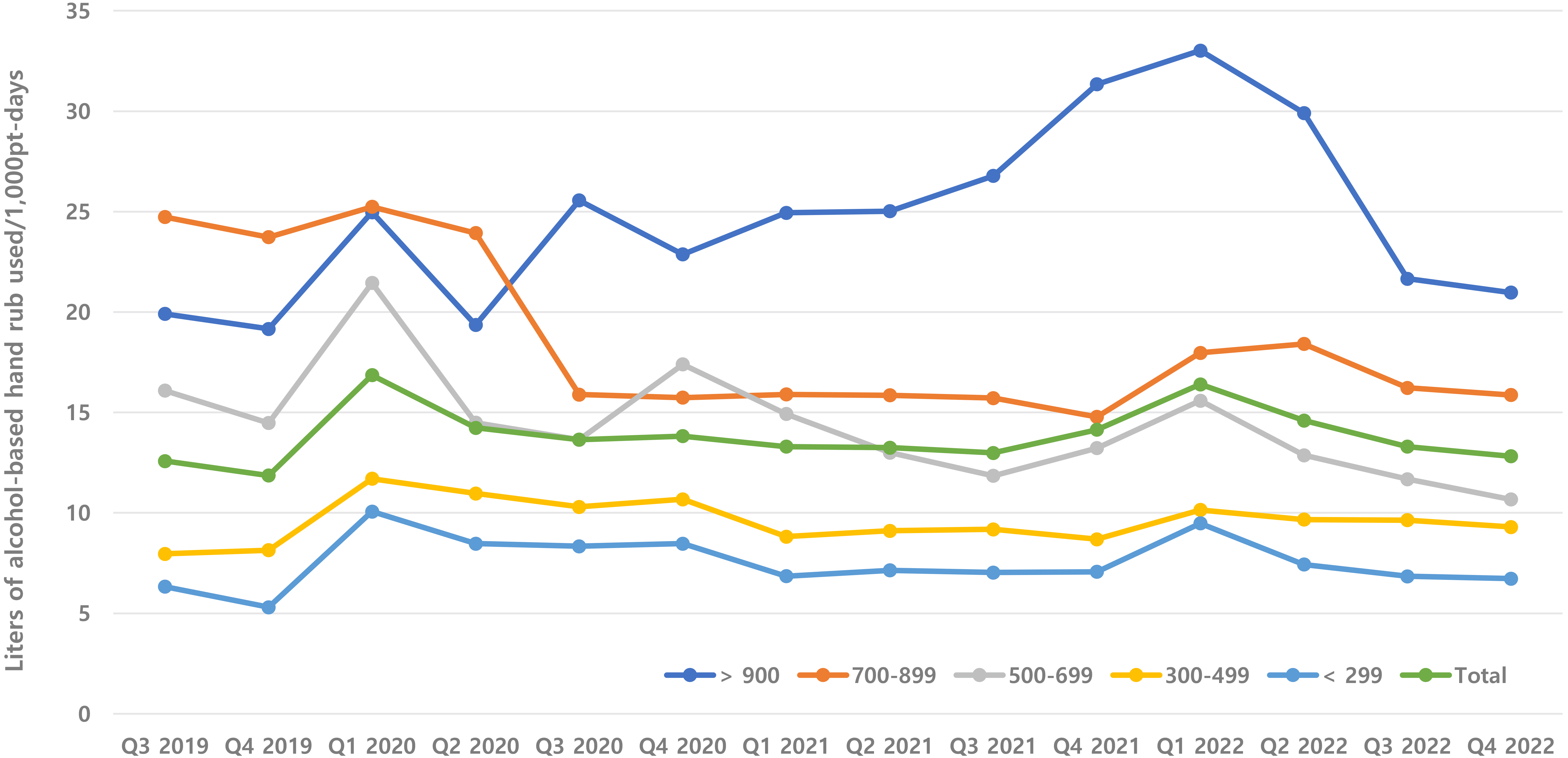
Hand hygiene compliance increased from 87.2% in Q3 2019 to 89.9% in 2022. Nurses and medical technologists showed the highest compliance rates, whereas doctors showed the lowest compliance rates. Intensive care units excelled in compliance, whereas emergency de partments lagged. Compliance was highest after patient contact and lowest when the patient’s surroundings were touched. Larger hospitals consumed more alcohol-based hand sanitizers than smaller hospitals did.
Conclusion
This study confirmed an improvement in hand hygiene compliance through sustained surveillance, indicating its contribution not only to preventing infection transfer within healthcare facilities but also to fostering a culture of hand hygiene in the country.
Figure
Reference
-
1. Horan TC, Andrus M, Dudeck MA. 2008; CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 36:309–32. DOI: 10.1016/j.ajic.2008.03.002. PMID: 18538699.2. Korean Society for Healthcare-associated Infection Control. 2023: 2-5; Healthcare associated infection control and prevention. Paju; Koonja publishing Inc. 2–5.3. World Health Organization (WHO). 2009. A guide to the implementation of the WHO multimodal hand hygiene improvement strategy. WHO;Geneva: p. 1–46.4. Weber D, Talbot T. 2020. Mayhall's hospital epidemiology and infection prevention. 5th ed. Wolters Kluwer;Philadelphia: p. 53–68.5. Wetzker W, Bunte-Schönberger K, Walter J, Pilarski G, Gastmeier P, Reichardt Ch. 2016; Compliance with hand hygiene: reference data from the national hand hygiene campaign in Germany. J Hosp Infect. 92:328–31. DOI: 10.1016/j.jhin.2016.01.022. PMID: 26984282.6. Grayson ML, Russo PL, Cruickshank M, Bear JL, Gee CA, Hughes CF, et al. 2011; Outcomes from the first 2 years of the Australian National Hand Hygiene Initiative. Med J Aust. 195:615–9. DOI: 10.5694/mja11.10747. PMID: 22107015.7. Grayson ML, Stewardson AJ, Russo PL, Ryan KE, Olsen KL, Havers SM, et al. 2018; ; Hand Hygiene Australia and the National Hand Hygiene Initiative. Effects of the Australian National Hand Hygiene Initiative after 8 years on infection control practices, health-care worker education, and clinical outcomes: a longitudinal study. Lancet Infect Dis. 18:1269–77. DOI: 10.1016/S1473-3099(18)30491-2. PMID: 30274723.8. Ministry of Health. The standards for calculating infection prevention and management fees. Notification no. 2022-285. https://www.mohw.go.kr/board.es?mid=a10409020000&bid=0026&act=view&list_no=374222&tag=&nPage=65.(Updated on 22 December 2022).9. Ministry of Health. The standards for calculating infection prevention and management fees at nursing hospitals. Notification no. 2023-109. https://www.mohw.go.kr/board.es?mid=a10409020000&bid=0026&act=view&list_no=376753&tag=&nPage=43.(Updated on 16 June 2023).10. Martos-Cabrera MB, Mota-Romero E, Martos-García R, Gómez-Urquiza JL, Suleiman-Martos N, Albendín-García L, et al. 2019; Hand hygiene teaching strategies among nursing staff: a systematic review. Int J Environ Res Public Health. 16:3039. DOI: 10.3390/ijerph16173039. PMID: 31443355. PMCID: PMC6747325.11. Reichardt C, Königer D, Bunte-Schönberger K, van der Linden P, Mönch N, Schwab F, et al. 2013; Three years of national hand hygiene campaign in Germany: what are the key conclusions for clinical practice? J Hosp Infect. 83 Suppl 1:S11–6. DOI: 10.1016/S0195-6701(13)60004-3. PMID: 23453170.12. Mouajou V, Adams K, DeLisle G, Quach C. 2022; Hand hygiene compliance in the prevention of hospital-acquired infections: a systematic review. J Hosp Infect. 119:33–48. DOI: 10.1016/j.jhin.2021.09.016. PMID: 34582962.13. Seo HJ, Sohng KY, Chang SO, Chaung SK, Won JS, Choi MJ. 2019; Interventions to improve hand hygiene compliance in emergency departments: a systematic review. J Hosp Infect. 102:394–406. DOI: 10.1016/j.jhin.2019.03.013. PMID: 30935982.14. Burnett E. 2009; Perceptions, attitudes, and behavior towards patient hand hygiene. Am J Infect Control. 37:638–42. DOI: 10.1016/j.ajic.2009.04.281. PMID: 19628304.15. Allegranzi B, Pittet D. 2009; Role of hand hygiene in healthcare-associated infection prevention. J Hosp Infect. 73:305–15. DOI: 10.1016/j.jhin.2009.04.019. PMID: 19720430.16. Jung SJ, Ahn MS, Jang MJ, Choi SY, Choi YJ, Jang JH, et al. 2023; Trends in the severity of COVID-19 in South Korea according to the dominant periods of SARS-CoV-2 variants. Public Health Wkly Rep. 16:1464–87.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Perspective of Nationwide Surveillance System for Surgical Site Infections
- Hand hygiene
- A Validation Study of Surveillance Data: Focus on the Korean National Healthcare-associated Infections Surveillance System (KONIS), Intensive Care Unit Module
- Prospective nationwide healthcare-associated infection surveillance system in South Korea
- Pilot Study of Healthcare-associated Infections Surveillance System in Long-term Care Facilities