Kosin Med J.
2024 Jun;39(2):132-137. 10.7180/kmj.23.153.
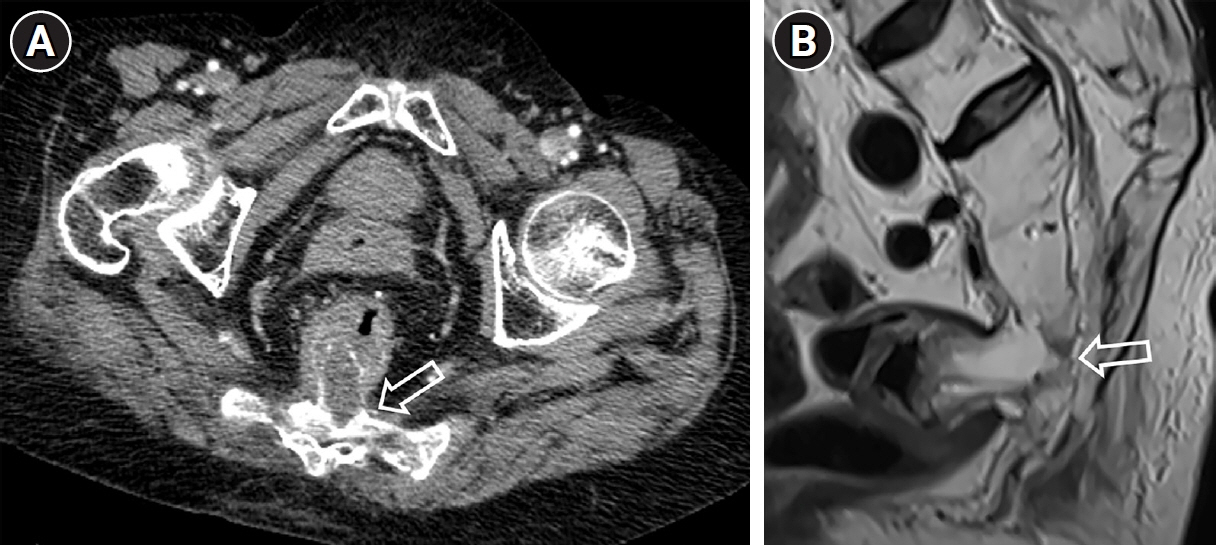
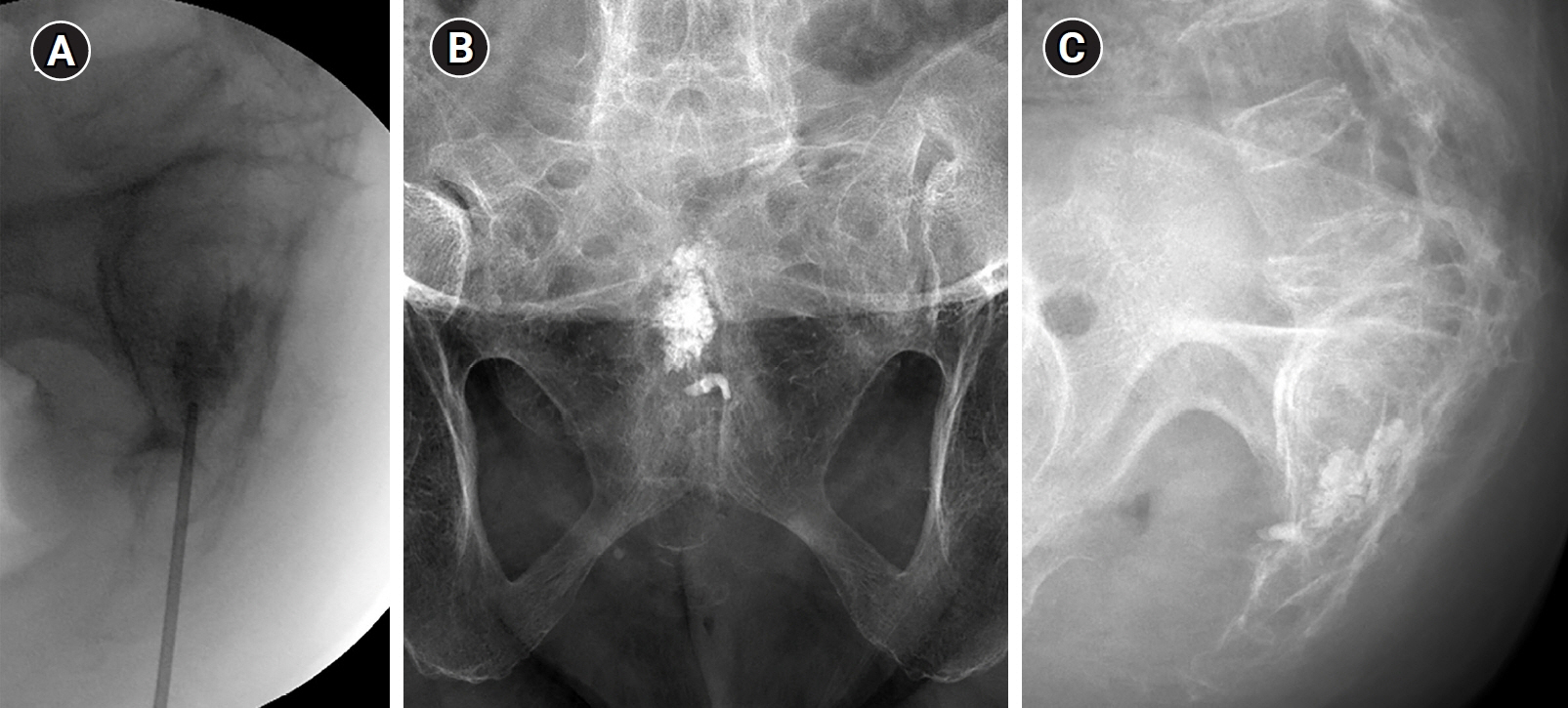
Interpedicular approach in percutaneous sacroplasty for treating pain due to direct invasion of rectal cancer into the S3 body: a case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kyungpook National University Chilgok Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- 2Department of Anesthesiology and Pain Medicine, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2556811
- DOI: http://doi.org/10.7180/kmj.23.153
Abstract
- Percutaneous sacroplasty is mainly used as an intervention for pain associated with sacral insufficiency fractures or sacral metastatic tumors. However, sacroplasty for managing the pain associated with direct sacral invasion of rectal cancer has been rarely reported. We present a case of a 74-year-old patient who underwent sacroplasty via the interpedicular approach under fluoroscopic guidance to relieve pain resulting from direct tumor invasion into the S3 body. After the procedure, the patient experienced immediate pain relief and did not feel worse pain with ambulation. Aside from peritumoral vascular leakage, no other significant complications occurred immediately post-procedure. Our results suggest that fluoroscopically guided interpedicular sacroplasty is a safe and effective option for relieving the pain associated with direct sacral invasion by rectal cancer.
Figure
Reference
-
References
1. Raque GH Jr, Vitaz TW, Shields CB. Treatment of neoplastic diseases of the sacrum. J Surg Oncol. 2001; 76:301–7.2. Sinaei M, Swallow C, Milot L, Moghaddam PA, Smith A, Atri M. Patterns and signal intensity characteristics of pelvic recurrence of rectal cancer at MR imaging. Radiographics. 2013; 33:E171–87.3. Tarawneh AM, Sabou S, AlKalbani S, Pasku D, Quraishi NA. Clinical outcomes of sacroplasty for metastatic sacral tumours: a systematic review and meta-analysis. Eur Spine J. 2020; 29:3116–22.4. Fırat AK, Gumus B, Kaya E, Kuku I, Harma A. Interpedicular approach in percutaneous sacroplasty for treatment of sacral vertebral body pathologic fractures. Cardiovasc Intervent Radiol. 2011; 34 Suppl 2:S282–7.5. Dehdashti AR, Martin JB, Jean B, Rufenacht DA. PMMA cementoplasty in symptomatic metastatic lesions of the S1 vertebral body. Cardiovasc Intervent Radiol. 2000; 23:235–7.6. Gupta AC, Chandra RV, Yoo AJ, Leslie-Mazwi TM, Bell DL, Mehta BP, et al. Safety and effectiveness of sacroplasty: a large single-center experience. AJNR Am J Neuroradiol. 2014; 35:2202–6.7. Tian QH, Liu HF, Wang T, Cheng YS, Wu CG. Percutaneous sacroplasty for painful sacral metastases involving multiple sacral vertebral bodies: initial experience with an interpedicular approach. Korean J Radiol. 2019; 20:939–46.8. Zhang J, Wu CG, Gu YF, Li MH. Percutaneous sacroplasty for sacral metastatic tumors under fluoroscopic guidance only. Korean J Radiol. 2008; 9:572–6.9. Kortman K, Ortiz O, Miller T, Brook A, Tutton S, Mathis J, et al. Multicenter study to assess the efficacy and safety of sacroplasty in patients with osteoporotic sacral insufficiency fractures or pathologic sacral lesions. J Neurointerv Surg. 2013; 5:461–6.10. Jayaraman MV, Chang H, Ahn SH. An easily identifiable anatomic landmark for fluoroscopically guided sacroplasty: anatomic description and validation with treatment in 13 patients. AJNR Am J Neuroradiol. 2009; 30:1070–3.11. Cotten A, Dewatre F, Cortet B, Assaker R, Leblond D, Duquesnoy B, et al. Percutaneous vertebroplasty for osteolytic metastases and myeloma: effects of the percentage of lesion filling and the leakage of methyl methacrylate at clinical follow-up. Radiology. 1996; 200:525–30.12. Frey ME, Warner C, Thomas SM, Johar K, Singh H, Mohammad MS, et al. Sacroplasty: a ten-year analysis of prospective patients treated with percutaneous sacroplasty: literature review and technical considerations. Pain Physician. 2017; 20:E1063–72.13. Moussazadeh N, Laufer I, Werner T, Krol G, Boland P, Bilsky MH, et al. Sacroplasty for cancer-associated insufficiency fractures. Neurosurgery. 2015; 76:446–50.14. Richards AM, Mears SC, Knight TA, Dinah AF, Belkoff SM. Biomechanical analysis of sacroplasty: does volume or location of cement matter? AJNR Am J Neuroradiol. 2009; 30:315–7.15. Belkoff SM, Molloy S. Temperature measurement during polymerization of polymethylmethacrylate cement used for vertebroplasty. Spine (Phila Pa 1976). 2003; 28:1555–9.16. O'Brien JP, Sims JT, Evans AJ. Vertebroplasty in patients with severe vertebral compression fractures: a technical report. AJNR Am J Neuroradiol. 2000; 21:1555–8.17. Andresen R, Radmer S, Ludtke CW, Kamusella P, Wissgott C, Schober HC. Balloon sacroplasty as a palliative pain treatment in patients with metastasis-induced bone destruction and pathological fractures. Rofo. 2014; 186:881–6.18. Chow E, Wong R, Hruby G, Connolly R, Franssen E, Fung KW, et al. Prospective patient-based assessment of effectiveness of palliative radiotherapy for bone metastases. Radiother Oncol. 2001; 61:77–82.19. Sasikumar A, Bhan C, Jenkins JT, Antoniou A, Murphy J. Systematic review of pelvic exenteration with en bloc sacrectomy for recurrent rectal adenocarcinoma: R0 resection predicts disease-free survival. Dis Colon Rectum. 2017; 60:346–52.20. Quraishi NA, Giannoulis KE, Edwards KL, Boszczyk BM. Management of metastatic sacral tumours. Eur Spine J. 2012; 21:1984–93.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Transiliac sacroplasty for Denis 3 fracture: Two cases report
- Percutaneous Sacroplasty for Painful Sacral Metastases Involving Multiple Sacral Vertebral Bodies: Initial Experience with an Interpedicular Approach
- Percutaneous Sacroplasty for the Sacral Insufficiency Fracture Caused by Metastasis
- Percutaneous Sacroplasty for Sacral Metastatic Tumors Under Fluoroscopic Guidance Only
- Therapeutic Considerations of Percutaneous Sacroplasty for the Sacral Insufficiency Fracture