Kosin Med J.
2024 Mar;39(1):44-50. 10.7180/kmj.23.126.
Human resources and medical supplies consumption during the COVID-19 pandemic: a single-center study
- Affiliations
-
- 1Department of Internal Medicine, Hallym University Kangnam Sacred Heart Hospital, Seoul, Korea
- KMID: 2556797
- DOI: http://doi.org/10.7180/kmj.23.126
Abstract
- Background
In the face of the unexpected coronavirus disease 2019 (COVID-19) pandemic, every country has struggled with insufficient human resources and medical supplies. This study aims to provide the statistical information necessary for discussing how to model stockpiles of medical resources.
Methods
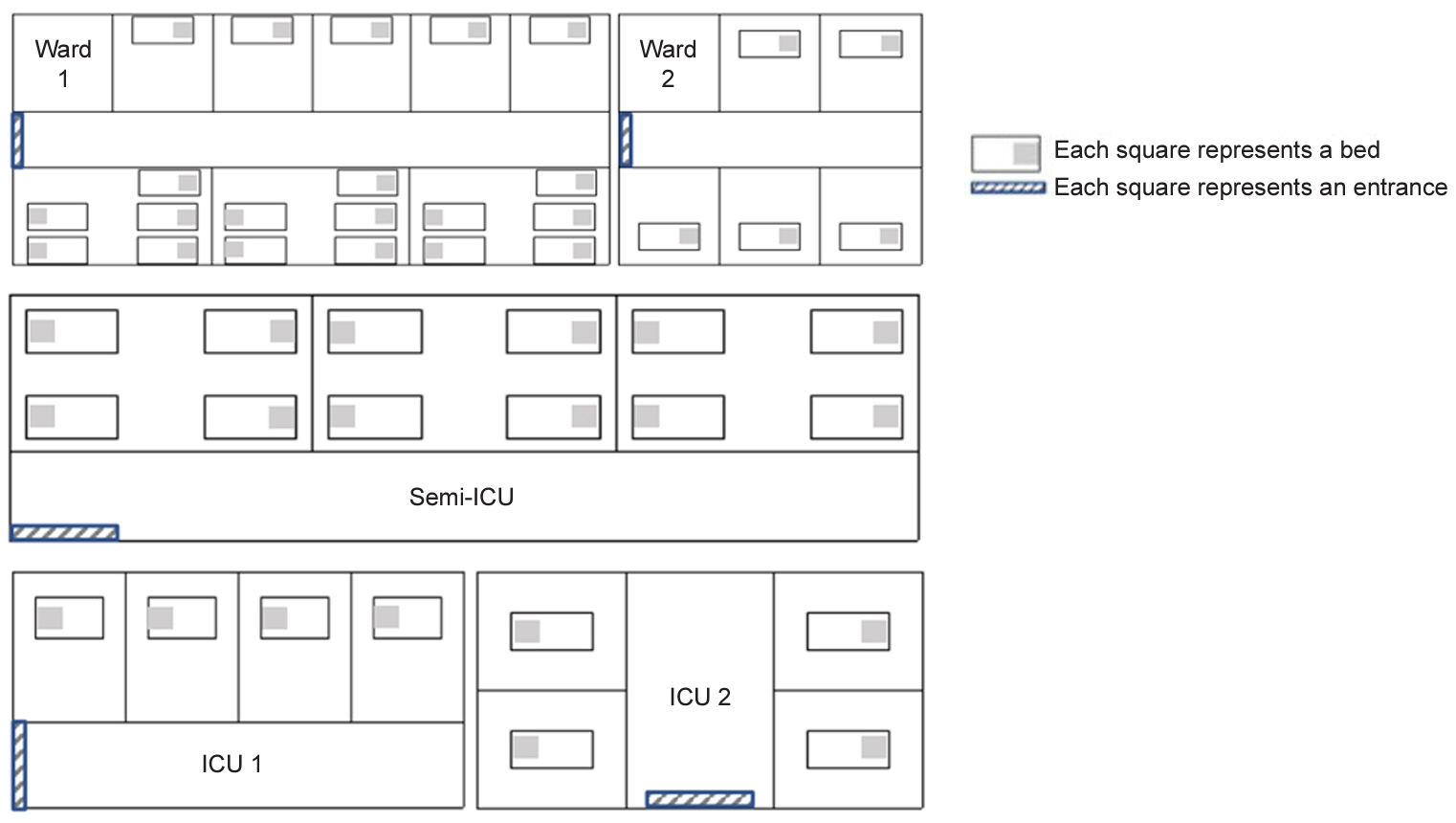
This study was conducted at the Hallym University Kangnam Sacred Heart Hospital, in South Korea. The study duration was 2 weeks, centered on March 16, 2022, when the number of daily confirmed patients with COVID-19 in Korea peaked. The number of human resources was obtained by counting the number of healthcare workers using CCTV. Drug prescriptions and medical device usage were obtained from electronic medical records.
Results
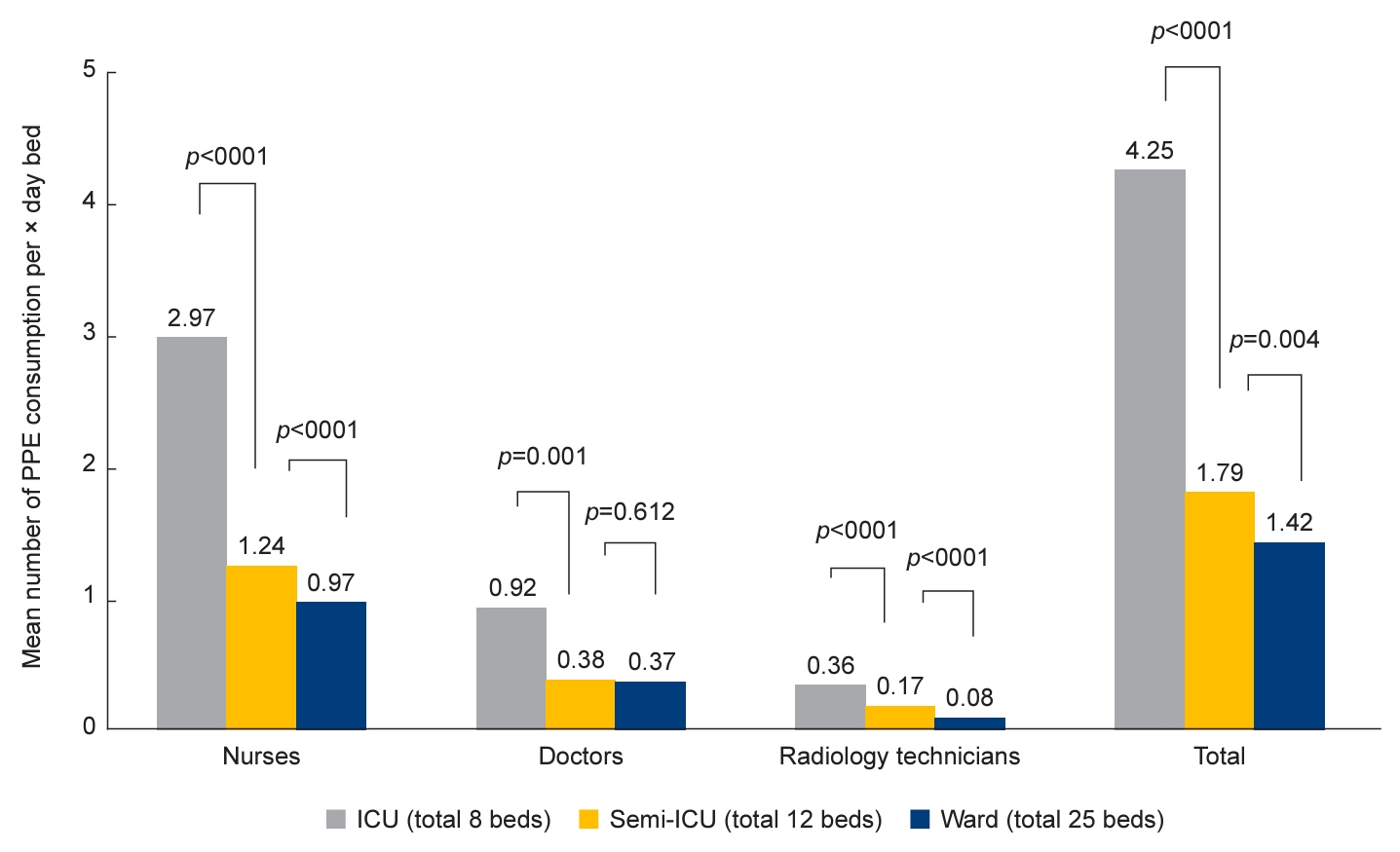
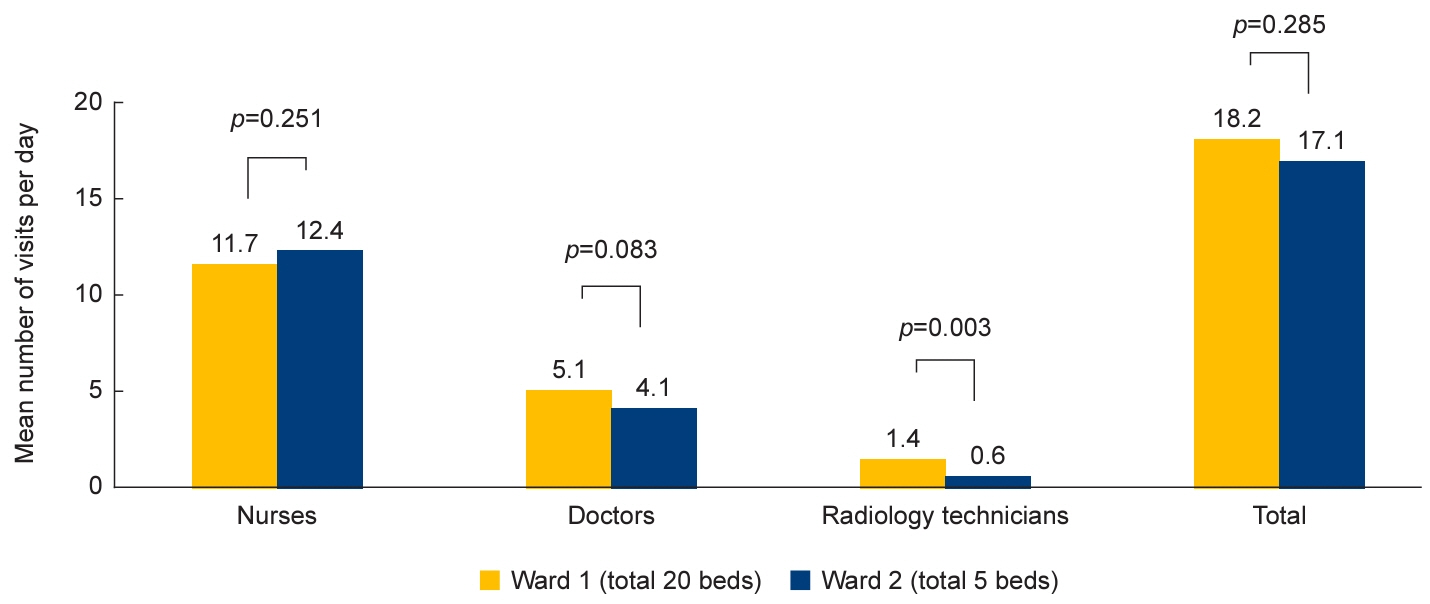
In total, 117 inpatients and 26,485 outpatients were managed at this hospital during the 2-week study period. Daily visits were highest among nurses in all units, followed by doctors and radiology technicians. The mean daily consumption of personal protective equipment (PPE) per bed was 4.3 sets in the intensive care unit (ICU), 1.8 in the semi-ICU, and 1.4 in the ward. Despite the four-fold difference in the number of patients, there was no statistically significant difference between the two wards in the number of daily visits. Drug prescription rates were higher among inpatients than at-home patients.
Conclusions
The higher the COVID-19 severity, the higher the consumption of PPE per patient. Among healthcare workers, nurses had the highest number of inpatient treatment visits for COVID-19. To efficiently utilize, PPE, structures containing more isolation beds in a single negative pressure isolation system would be preferred.
Keyword
Figure
Reference
-
References
1. World Health Organization (WHO). Timeline: WHO’s COVID-19 response [Internet]. WHO;c2022. [cited 2023 Jun 28]. https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline.2. World Health Organization (WHO). WHO Dashboard of COVID-19 related recommendations [Internet]. WHO;c2023. [cited 2023 Aug 9]. https://app.powerbi.com/view?r=eyJrIjoiODgyYjRmZjQtN2UyNi00NGE4LTg1YzMtYzE2OGFhZjBiYzFjIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9&pageName=ReportSection729b5bf5a0b579e86134.3. Korea Disease Control and Prevention Agency (KDCA). Coronavirus disease-19 (COVID-19) [Internet]. KDCA;2023. [cited 2023 Aug 9]. https://ncv.kdca.go.kr/hcp/page.do.4. Best S, Williams SJ. What have we learnt about the sourcing of personal protective equipment during pandemics? Leadership and management in healthcare supply chain management: a scoping review. Front Public Health. 2021; 9:765501.5. Rich-Edwards JW, Ding M, Rocheleau CM, Boiano JM, Kang JH, Becene I, et al. American frontline healthcare personnel’s access to and use of personal protective equipment early in the COVID-19 pandemic. J Occup Environ Med. 2021; 63:913–20.6. Rebmann T, Vassallo A, Holdsworth JE. Availability of personal protective equipment and infection prevention supplies during the first month of the COVID-19 pandemic: a national study by the APIC COVID-19 task force. Am J Infect Control. 2021; 49:434–7.7. Baloch G, Gzara F, Elhedhli S. Covid-19 PPE distribution planning with demand priorities and supply uncertainties. Comput Oper Res. 2022; 146:105913.8. Alizadeh-Meghrazi M, Tosarkani BM, Amin SH, Popovic MR, Ahi P. Design and optimization of a sustainable and resilient mask supply chain during the COVID-19 pandemic: a multi-objective approach. Environ Dev Sustain 2022 Aug 18 [Epub]. https://doi.org/10.1007/s10668-022-02604-z.9. Ash C, Diallo C, Venkatadri U, VanBerkel P. Distributionally robust optimization of a Canadian healthcare supply chain to enhance resilience during the COVID-19 pandemic. Comput Ind Eng. 2022; 168:108051.10. Krylova O, Kazmi O, Wang H, Lam K, Logar-Henderson C, Gapanenko K. Estimating surge in COVID-19 cases, hospital resources and PPE demand with the interactive and locally-informed COVID-19 Health System Capacity Planning Tool. Int J Popul Data Sci. 2022; 5:1710.11. Furman E, Cressman A, Shin S, Kuznetsov A, Razak F, Verma A, et al. Prediction of personal protective equipment use in hospitals during COVID-19. Health Care Manag Sci. 2021; 24:439–53.12. Park JJ, Seo YB, Lee J, Na SH, Choi YK. Protocol and clinical characteristics of patients under ‘at-home care’ for COVID-19 in South Korea: a retrospective cohort study. BMJ Open. 2022; 12:e061765.13. Kam AW, King N, Sharma A, Phillips N, Nayyar V, Shaban RZ. Short research paper: personal protective equipment for the care of suspected and confirmed COVID-19 patients: modelling requirements and burn rate. Infect Dis Health. 2021; 26:214–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Laryngoscopy During the COVID-19 Pandemic
- State and Improvement Policy of Psychiatric Emergency during COVID-19 Pandemic
- The COVID-19 pandemic's impact on prostate cancer screening and diagnosis in Korea
- The Management of Thyroid Disease in COVID-19 Pandemic
- The Activities and Roles of Trauma Surgeons in the Treatment of COVID-19 Patients