J Korean Med Sci.
2024 Jun;39(24):e209. 10.3346/jkms.2024.39.e209.
Glycemic Control and Oral Health Outcomes in Patients With Diabetes: Insights From a Nationwide Korean Survey
- Affiliations
-
- 1Department of Prosthodontics, Dental Clinic Center, Chungbuk National University Hospital, Cheongju, Korea
- 2Division of Pulmonary Medicine and Allergy, Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- 3Department of Mathematics, College of Natural Sciences, Hanyang University, Seoul, Korea
- 4Division of Pulmonary Medicine, Department of Internal Medicine, Chungbuk National University College of Medicine and Chungbuk National University Hospital, Cheongju, Korea
- 5Division of Endocrinology and Metabolism, Department of Internal Medicine, Chungbuk National University College of Medicine and Chungbuk National University Hospital, Cheongju, Korea
- KMID: 2556689
- DOI: http://doi.org/10.3346/jkms.2024.39.e209
Abstract
- Background
Diabetes is recognized as a risk factor for various inflammatory conditions, including periodontitis. There exists a bidirectional relationship between glycemic control and oral health in individuals with diabetes. This study aimed to analyze the link between glycemic control and oral health status among Korean patients with diabetes.
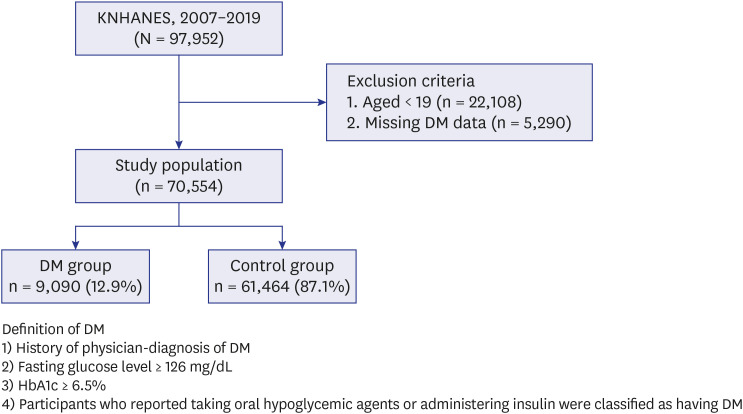
Methods
Using data from a population-based nationwide survey conducted between 2007 and 2019, we identified 70,554 adults with diabetes-related information. The study population included 9,090 individuals diagnosed with diabetes and 61,164 healthy controls. The association between glycemic control, defined by mean glycated hemoglobin (HbA1c) values, and various oral health measures, such as tooth brushing frequency, periodontitis, denture wearing, Decayed, Missing, and Filled Teeth (DMFT) index, number of remaining teeth, and past-year dental clinic visits, was evaluated using multivariate logistic regression analyses.
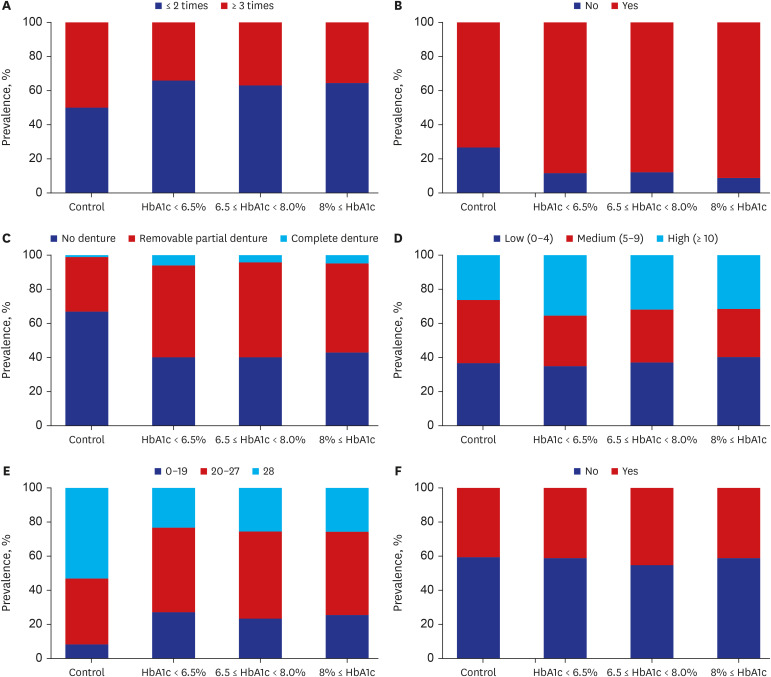
Results
Compared to the control group, patients with diabetes exhibited a higher prevalence of periodontitis (88.6% vs. 73.3%), complete dentures (5.0% vs. 1.5%), and elevated DMFT index (33.2% vs. 26.7%) (all P < 0.001). Multivariate analyses revealed significant associations between diabetes and several oral health factors: denture status (No denture: adjusted odds ratio [aOR], 0.784; 95% confidence interval [CI], 0.627–0.979), and having fewer permanent teeth (0–19) (aOR, 1.474; 95% CI, 1.085–2.003). Additionally, a positive correlation was found between higher HbA1c levels and the risk of having fewer remaining teeth (0–19) (HbA1c < 6.5%: aOR, 1.129; 95% CI, 0.766–1.663; 6.5% ≤ HbA1c < 8.0%: aOR, 1.590; 95% CI, 1.117– 2.262; HbA1c ≥ 8%: aOR, 1.910; 95% CI, 1.145–3.186) (P for trends = 0.041).
Conclusion
We found a positive association between diabetes and poor oral health, as well as a noteworthy relationship between reduced permanent teeth (≤ 19) and glycemic control. These insights emphasize the critical role of oral health management in diabetic care and underscore the importance of maintaining effective glycemic control strategies for overall health and well-being in patients with diabetes.
Keyword
Figure
Reference
-
1. Bloomgarden ZT. Diabetes complications. Diabetes Care. 2004; 27(6):1506–1514. PMID: 15161810.
Article2. Knapp S. Diabetes and infection: is there a link?--A mini-review. Gerontology. 2013; 59(2):99–104. PMID: 23182884.3. Casanova L, Hughes FJ, Preshaw PM. Diabetes and periodontal disease: a two-way relationship. Br Dent J. 2014; 217(8):433–437. PMID: 25342350.
Article4. Holt RI, de Groot M, Golden SH. Diabetes and depression. Curr Diab Rep. 2014; 14(6):491. PMID: 24743941.
Article5. Stöhr J, Barbaresko J, Neuenschwander M, Schlesinger S. Bidirectional association between periodontal disease and diabetes mellitus: a systematic review and meta-analysis of cohort studies. Sci Rep. 2021; 11(1):13686. PMID: 34211029.
Article6. Graves DT, Ding Z, Yang Y. The impact of diabetes on periodontal diseases. Periodontol 2000. 2020; 82(1):214–224. PMID: 31850631.
Article7. Genco RJ, Graziani F, Hasturk H. Effects of periodontal disease on glycemic control, complications, and incidence of diabetes mellitus. Periodontol 2000. 2020; 83(1):59–65. PMID: 32385875.
Article8. Khader YS, Dauod AS, El-Qaderi SS, Alkafajei A, Batayha WQ. Periodontal status of diabetics compared with nondiabetics: a meta-analysis. J Diabetes Complications. 2006; 20(1):59–68. PMID: 16389170.
Article9. ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Cusi K, et al. American Diabetes Association Professional Practice C. 4. comprehensive medical evaluation and assessment of comorbidities: standards of care in diabetes-2024. Diabetes Care. 2024; 47(Suppl 1):S52–S76. PMID: 38078591.10. Han K, Park JB. Clinical implications of age and sex in the prevalence of periodontitis in Korean adults with diabetes. Exp Ther Med. 2018; 15(4):3865–3873. PMID: 29556264.
Article11. ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care. 2023; 46(Suppl 1):S19–S40. PMID: 36507649.12. Lee DH, Jung KY, Park KS, Kim KM, Moon JH, Lim S, et al. Characterization of patients with type 2 diabetes according to body mass index: Korea National Health and Nutrition Examination Survey from 2007 to 2011. Endocrinol Metab (Seoul). 2015; 30(4):514–521. PMID: 26354494.
Article13. Choi JH, Lee KA, Moon JH, Chon S, Kim DJ, Kim HJ, et al. 2023 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J. 2023; 47(5):575–594. PMID: 37793979.
Article14. World Health Organization. Oral Health Surveys: Basic Methods. Geneva, Switzerland: World Health Organization;2013.15. Hancocks S. Federation Dentaire Internationale. The FDI’s first ten years, 1900–1910. Fédération Dentaire Internationale. Int Dent J. 2000; 50(4):175–183. PMID: 11042817.16. Cappelli DP. Prevention in Clinical Oral Health Care. Philadelphia, PA, USA: Elsevier Health Sciences;2007.17. Klein HP, Knutson JW. Dental status and dental needs of elementary school children. Public Health Rep. 1938; 53:751–765.18. A guide to the UK Adult Dental Health Survey 1998. Br Dent J. 2001; (Spec No):1–56.19. Sheiham A, Steele JG, Marcenes W, Finch S, Walls AW. The impact of oral health on stated ability to eat certain foods; findings from the National Diet and Nutrition Survey of Older People in Great Britain. Gerodontology. 1999; 16(1):11–20. PMID: 10687504.
Article20. Kim SW, Han K, Kim SY, Park CK, Rhee CK, Yoon HK. The relationship between the number of natural teeth and airflow obstruction: a cross-sectional study using data from the Korean National Health and Nutrition Examination Survey. Int J Chron Obstruct Pulmon Dis. 2015; 11:13–21. PMID: 26730184.
Article21. Kim MK, Lee WY, Kang JH, Kang JH, Kim BT, Kim SM, et al. 2014 clinical practice guidelines for overweight and obesity in Korea. Endocrinol Metab (Seoul). 2014; 29(4):405–409. PMID: 25559568.
Article22. Shin SH, Park J, Cho J, Sin DD, Lee H, Park HY. Severity of airflow obstruction and work loss in a nationwide population of working age. Sci Rep. 2018; 8(1):9674. PMID: 29946117.
Article23. Azarpazhooh A, Leake JL. Systematic review of the association between respiratory diseases and oral health. J Periodontol. 2006; 77(9):1465–1482. PMID: 16945022.
Article24. Sacks DB, Arnold M, Bakris GL, Bruns DE, Horvath AR, Lernmark Å, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care. 2023; 46(10):e151–e199. PMID: 37471273.
Article25. Kim HL, Lee EM, Ahn SY, Kim KI, Kim HC, Kim JH, et al. The 2022 focused update of the 2018 Korean Hypertension Society Guidelines for the management of hypertension. Clin Hypertens. 2023; 29(1):11. PMID: 36788612.
Article26. Jellinger PS, Handelsman Y, Rosenblit PD, Bloomgarden ZT, Fonseca VA, Garber AJ, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Guidelines for Management of Dyslipidemia and Prevention of Cardiovascular Disease. Endocr Pract. 2017; 23(Suppl 2):1–87.
Article27. Cekici A, Kantarci A, Hasturk H, Van Dyke TE. Inflammatory and immune pathways in the pathogenesis of periodontal disease. Periodontol 2000. 2014; 64(1):57–80. PMID: 24320956.
Article28. Latti BR, Kalburge JV, Birajdar SB, Latti RG. Evaluation of relationship between dental caries, diabetes mellitus and oral microbiota in diabetics. J Oral Maxillofac Pathol. 2018; 22(2):282.
Article29. Lontchi-Yimagou E, Sobngwi E, Matsha TE, Kengne AP. Diabetes mellitus and inflammation. Curr Diab Rep. 2013; 13(3):435–444. PMID: 23494755.
Article30. Kudiyirickal MG, Pappachan JM. Diabetes mellitus and oral health. Endocrine. 2015; 49(1):27–34. PMID: 25487035.
Article31. Taboza ZA, Costa KL, Silveira VR, Furlaneto FA, Montenegro R Jr, Russell S, et al. Periodontitis, edentulism and glycemic control in patients with type 2 diabetes: a cross-sectional study. BMJ Open Diabetes Res Care. 2018; 6(1):e000453.
Article32. Zhang Y, Leveille SG, Camhi SM, Shi L. Association of oral care with periodontitis and glycemic control among US adults with diabetes. BMC Oral Health. 2023; 23(1):903. PMID: 37990177.
Article33. de Lima AK, Amorim Dos Santos J, Stefani CM, Almeida de Lima A, Damé-Teixeira N. Diabetes mellitus and poor glycemic control increase the occurrence of coronal and root caries: a systematic review and meta-analysis. Clin Oral Investig. 2020; 24(11):3801–3812.
Article34. Chang Y, Lee JS, Lee KJ, Woo HG, Song TJ. Improved oral hygiene is associated with decreased risk of new-onset diabetes: a nationwide population-based cohort study. Diabetologia. 2020; 63(5):924–933. PMID: 32128623.
Article36. Newman MG, Takei H, Klokkevold PR, Carranza FA. Carranza’s Clinical Periodontology. Philadelphia, PA, USA: Elsevier Health Sciences;2011.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors Associated with Poor Glycemic Control among Patients with Type 2 Diabetes Mellitus: The Fifth Korea National Health and Nutrition Examination Survey (2010-2012)
- Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
- Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
- Diabetes-related Characteristics in Men with Diabetes for the Glucose Control Group and Noncontrol Group
- Subjective Assessment of Diabetes Self-Care Correlates with Perceived Glycemic Control but not with Actual Glycemic Control