Neurointervention.
2024 Jul;19(2):123-128. 10.5469/neuroint.2024.00150.
A Case of Severe Delayed Vasospasm after Clipping Surgery for an Unruptured Intracranial Aneurysm
- Affiliations
-
- 1Jeju National University School of Medicine, Jeju, Korea
- 2Department of Neurology, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- 3Department of Neurosurgery, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea
- 4Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2556665
- DOI: http://doi.org/10.5469/neuroint.2024.00150
Abstract
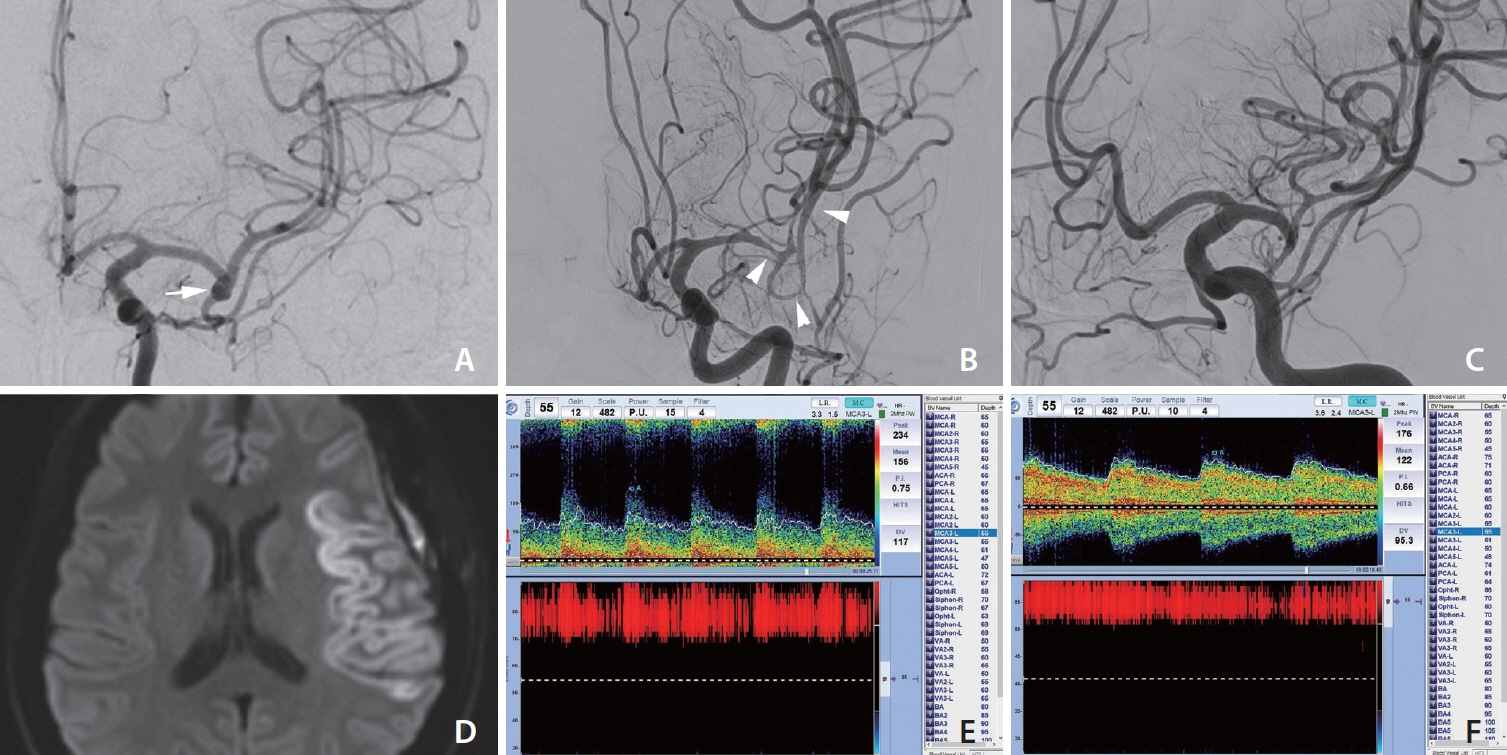
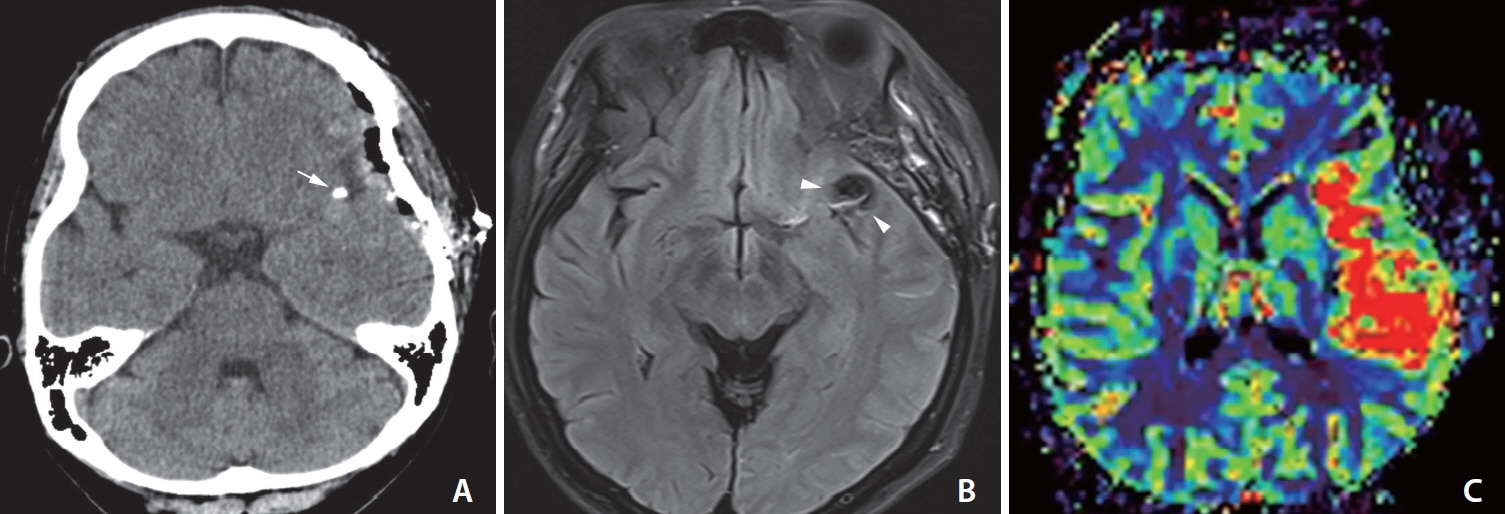
- Delayed ischemic stroke associated with intractable vasospasm after clipping of unruptured intracranial aneurysms (UIAs) has been rarely reported. We report a patient with delayed ischemic stroke associated with intractable vasospasm following UIA clipping. A middle-aged female underwent surgery for unruptured middle cerebral artery bifurcation aneurysms. The patient tolerated the neurosurgical procedure well. Seven days postoperatively, the headache was unbearable; a postcraniotomy headache persisted and abruptly presented with global aphasia and right-sided hemiplegia after a nap. Emergency digital subtraction angiography showed severe luminal narrowing with segmental vasoconstriction, consistent with severe vasospasm. The patient’s neurological deficit improved after chemical angioplasty. Neurosurgeons should pay close attention to this treatable/preventive entity after neurological deterioration following UIA clipping, even in patients without subarachnoid hemorrhage.
Keyword
Figure
Reference
-
1. Laukka D, Kivelev J, Rahi M, Vahlberg T, Paturi J, Rinne J, et al. Detection rates and trends of asymptomatic unruptured intracranial aneurysms from 2005 to 2019. Neurosurgery. 2024; 94:297–306.
Article2. Vlak MH, Algra A, Brandenburg R, Rinkel GJ. Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: a systematic review and meta-analysis. Lancet Neurol. 2011; 10:626–636.
Article3. Fu AY, Kumarapuram S, Sreenivasan S, Roychowdhury S, Gupta G. Trends in global research for treating intracranial aneurysms: a bibliometric analysis. World Neurosurg. 2023; 177:143–151.e4.
Article4. Scullen T, Mathkour M, Nerva JD, Dumont AS, Amenta PS. Editorial. Clipping versus coiling for the treatment of middle cerebral artery aneurysms: which modality should be considered first? J Neurosurg. 2019; 133:1120–1123.
Article5. Pflaeging M, Kabbasch C, Schlamann M, Pennig L, Juenger ST, Grunz JP, et al. Microsurgical clipping versus advanced endovascular treatment of unruptured middle cerebral artery bifurcation aneurysms after a “coil-first” policy. World Neurosurg. 2021; 149:e336–e344.
Article6. Lee SH, Lee SU, Kwon OK, Bang JS, Ban SP, Kim T, et al. Clinical outcomes of clipping and coiling in elderly patients with unruptured cerebral aneurysms: a national cohort study in Korea. J Korean Med Sci. 2021; 36:e178.
Article7. Campe C, Neumann J, Sandalcioglu IE, Rashidi A, Luchtmann M. Vasospasm and delayed cerebral ischemia after uneventful clipping of an unruptured intracranial aneurysm - a case report. BMC Neurol. 2019; 19:226.
Article8. Paolini S, Kanaan Y, Wagenbach A, Fraser K, Lanzino G. Cerebral vasospasm in patients with unruptured intracranial aneurysms. Acta Neurochir (Wien). 2005; 147:1181–1188. discussion 1188.
Article9. Peterson CM, Podila SS, Girotra T. Unruptured aneurysmal clipping complicated by delayed and refractory vasospasm: case report. BMC Neurol. 2020; 20:344.
Article10. Vachata P, Lodin J, Hejčl A, Cihlář F, Sameš M. Delayed ischemic neurological deficit after uneventful elective clipping of unruptured intracranial aneurysms. Brain Sci. 2020; 10:495.
Article11. Gutiérrez O, Caldas JG, Rabello JP. Unruptured aneurysm: vasospasm after surgery and endovascular treatment. A case report. Interv Neuroradiol. 2001; 7:37–39.
Article12. Kitazawa K, Hongo K, Tanaka Y, Oikawa S, Kyoshima K, Kobayashi S. Postoperative vasospasm of unruptured paraclinoid carotid aneurysms: analysis of 30 cases. J Clin Neurosci. 2005; 12:150–155.
Article13. Tsyben A, Paldor I, Laidlaw J. Cerebral vasospasm and delayed ischaemic deficit following elective aneurysm clipping. J Clin Neurosci. 2016; 34:33–38.
Article14. Kim M, Son W, Kang DH, Park J. Cerebral vasospasm with delayed ischemic neurologic deficit after unruptured aneurysm surgery: report of two cases and review of the literature. J Korean Neurosurg Soc. 2021; 64:665–670.
Article15. Hashimoto H, Kameda M, Yasuhara T, Date I. A case of unexpected symptomatic vasospasm after clipping surgery for an unruptured intracranial aneurysm. J Stroke Cerebrovasc Dis. 2016; 25:e25–e27.
Article16. Bloomfield SM, Sonntag VK. Delayed cerebral vasospasm after uncomplicated operation on an unruptured aneurysm: case report. Neurosurgery. 1985; 17:792–796.
Article17. Ceraudo M, Truffelli M, Anania P, Prior A, D’Andrea A, Zona G, et al. A case report of cerebral vasospasm following elective clipping of unruptured aneurysm: pathogenetic theories and clinical features of a dangerous underestimated event. Surg Case Rep. 2020; 3:1–6.18. Yang K, Ahn JS, Park JC, Kwon DH, Kwun BD. Clinical and angiographical delayed cerebral vasospasms after uncomplicated surgical clipping of unruptured intracranial aneurysms: illustrated review and two case reports. Turk Neurosurg. 2015; 25:662–665.19. Cuoco JA, Guilliams EL, Rogers CM, Patel BM, Marvin EA. Recurrent cerebral vasospasm and delayed cerebral ischemia weeks subsequent to elective clipping of an unruptured middle cerebral artery aneurysm. World Neurosurg. 2020; 141:52–58.
Article20. Knight JA 2nd, Bigder MG, Mandel M, Li Y, Steinberg GK. Contralateral vasospasm in an uncomplicated elective anterior communicating artery aneurysm clipping. World Neurosurg. 2020; 138:214–217.
Article21. Hansen-Schwartz J. Cerebral vasospasm: a consideration of the various cellular mechanisms involved in the pathophysiology. Neurocrit Care. 2004; 1:235–246.
Article22. Cook DA. Mechanisms of cerebral vasospasm in subarachnoid haemorrhage. Pharmacol Ther. 1995; 66:259–284.
Article23. Witten AJ, Ordaz JD, Alentado VJ, Bohnstedt B. Intracranial vasospasm after evacuation of acute spontaneous subdural hematoma. Cureus. 2021; 13:e15284.
Article24. Rocha-Filho PA, Gherpelli JL, de Siqueira JT, Rabello GD. Post-craniotomy headache: characteristics, behaviour and effect on quality of life in patients operated for treatment of supratentorial intracranial aneurysms. Cephalalgia. 2008; 28:41–48.
Article25. Chowdhury T, Garg R, Sheshadri V, Venkatraghavan L, Bergese SD, Cappellani RB, et al. Perioperative factors contributing the post-craniotomy pain: a synthesis of concepts. Front Med (Lausanne). 2017; 4:23.
Article26. Lai PMR, Gormley WB, Patel N, Frerichs KU, Aziz-Sultan MA, Du R. Age-dependent radiographic vasospasm and delayed cerebral ischemia in women after aneurysmal subarachnoid hemorrhage. World Neurosurg. 2019; 130:e230–e235.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postoperative Vasospasm in Unruptured Intracranial Aneurysm
- Cerebral Vasospasm with Delayed Ischemic Neurologic Deficit after Unruptured Aneurysm Surgery : Report of Two Cases and Review of the Literature
- Letters to the Editor: Cerebral Vasospasm after Surgical Clipping Versus GDC Embolization in Ruptured Intracranial Aneurysm
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms
- Surgical Treatment of Unruptured Cerebral Aneurysms