Endocrinol Metab.
2024 Jun;39(3):479-488. 10.3803/EnM.2023.1857.
Impact of Antidiabetic Drugs on Clinical Outcomes of COVID-19: A Nationwide Population-Based Study
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 3Department of Internal Medicine, Sungkyunkwan University School of Medicine, Suwon, Korea
- 4Department of Biostatistics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Statistics and Actuarial Science, Soongsil University, Seoul, Korea
- KMID: 2556640
- DOI: http://doi.org/10.3803/EnM.2023.1857
Abstract
- Background
Inconsistent results have been reported regarding the association between the use of antidiabetic drugs and the clinical outcomes of coronavirus disease 2019 (COVID-19). This study aimed to investigate the effect of antidiabetic drugs on COVID-19 outcomes in patients with diabetes using data from the National Health Insurance Service (NHIS) in South Korea.
Methods
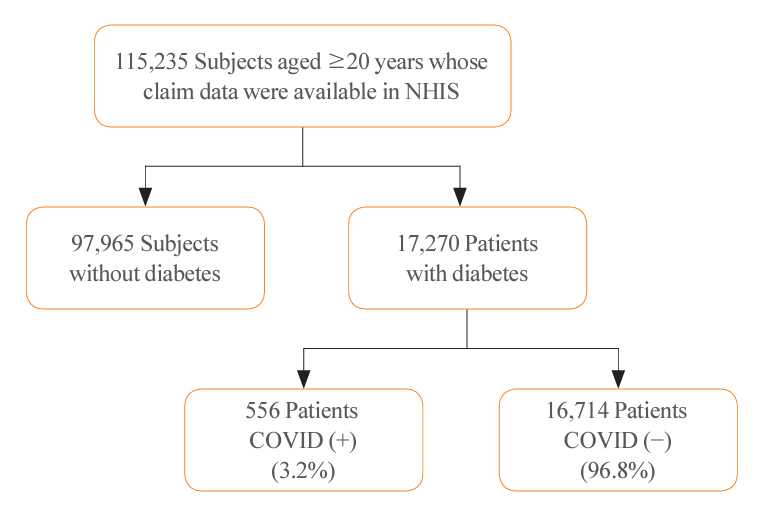
We analyzed the NHIS data of patients aged ≥20 years who tested positive for COVID-19 and were taking antidiabetic drugs between December 2019 and June 2020. Multiple logistic regression analysis was performed to analyze the clinical outcomes of COVID-19 based on the use of antidiabetic drugs.
Results
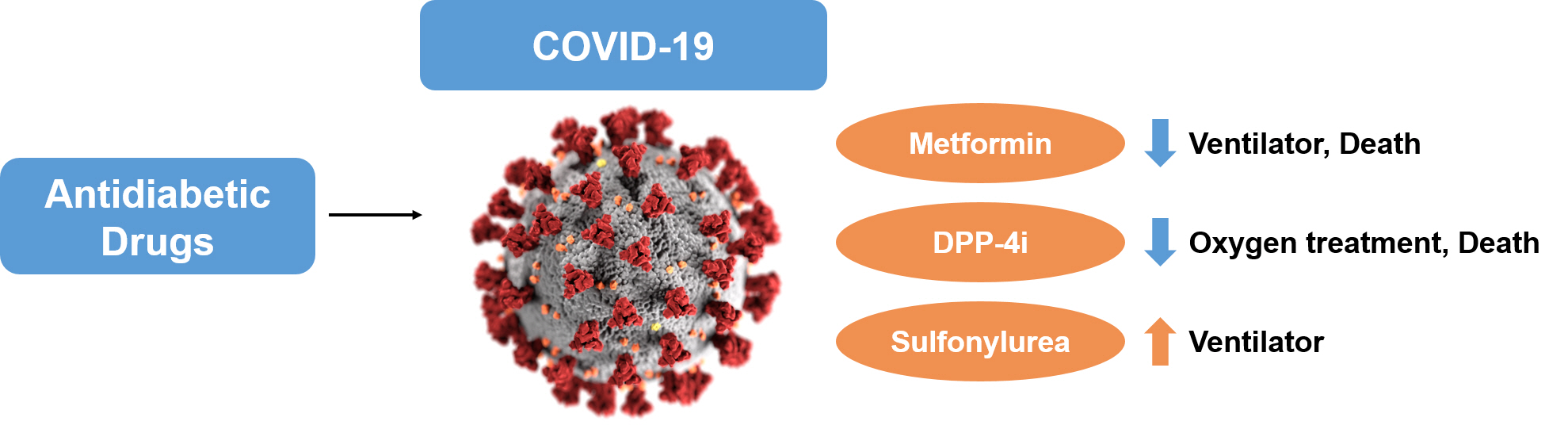
A total of 556 patients taking antidiabetic drugs tested positive for COVID-19, including 271 male (48.7%), most of whom were in their sixties. Of all patients, 433 (77.9%) were hospitalized, 119 (21.4%) received oxygen treatment, 87 (15.6%) were admitted to the intensive care unit, 31 (5.6%) required mechanical ventilation, and 61 (11.0%) died. Metformin was significantly associated with the lower risks of mechanical ventilation (odds ratio [OR], 0.281; 95% confidence interval [CI], 0.109 to 0.720; P=0.008), and death (OR, 0.395; 95% CI, 0.182 to 0.854; P=0.018). Dipeptidylpeptidase-4 inhibitor (DPP-4i) were significantly associated with the lower risks of oxygen treatment (OR, 0.565; 95% CI, 0.356 to 0.895; P=0.015) and death (OR, 0.454; 95% CI, 0.217 to 0.949; P=0.036). Sulfonylurea was significantly associated with the higher risk of mechanical ventilation (OR, 2.579; 95% CI, 1.004 to 6.626; P=0.049).
Conclusion
In patients with diabetes and COVID-19, metformin exhibited reduced risks of mechanical ventilation and death, DPP- 4i was linked with lower risks of oxygen treatment and death, while sulfonylurea was related to the increased risk of mechanical ventilation.
Keyword
Figure
Reference
-
1. Gao YD, Ding M, Dong X, Zhang JJ, Kursat Azkur A, Azkur D, et al. Risk factors for severe and critically ill COVID-19 patients: a review. Allergy. 2021; 76:428–55.
Article2. Zhang JJ, Dong X, Liu GH, Gao YD. Risk and protective factors for COVID-19 morbidity, severity, and mortality. Clin Rev Allergy Immunol. 2023; 64:90–107.
Article3. Guo L, Shi Z, Zhang Y, Wang C, Do Vale Moreira NC, Zuo H, et al. Comorbid diabetes and the risk of disease severity or death among 8807 COVID-19 patients in China: a meta-analysis. Diabetes Res Clin Pract. 2020; 166:108346.
Article4. Shi Q, Zhang X, Jiang F, Zhang X, Hu N, Bimu C, et al. Clinical characteristics and risk factors for mortality of COVID-19 patients with diabetes in Wuhan, China: a two-center, retrospective study. Diabetes Care. 2020; 43:1382–91.
Article5. Zhang Y, Li H, Zhang J, Cao Y, Zhao X, Yu N, et al. The clinical characteristics and outcomes of patients with diabetes and secondary hyperglycaemia with coronavirus disease 2019: a single-centre, retrospective, observational study in Wuhan. Diabetes Obes Metab. 2020; 22:1443–54.
Article6. Moon SJ, Rhee EJ, Jung JH, Han KD, Kim SR, Lee WY, et al. Independent impact of diabetes on the severity of coronavirus disease 2019 in 5,307 patients in South Korea: a nationwide cohort study. Diabetes Metab J. 2020; 44:737–46.
Article7. Kim MK, Jeon JH, Kim SW, Moon JS, Cho NH, Han E, et al. The clinical characteristics and outcomes of patients with moderate-to-severe coronavirus disease 2019 infection and diabetes in Daegu, South Korea. Diabetes Metab J. 2020; 44:602–13.
Article8. Chung SM, Lee YY, Ha E, Yoon JS, Won KC, Lee HW, et al. The risk of diabetes on clinical outcomes in patients with coronavirus disease 2019: a retrospective cohort study. Diabetes Metab J. 2020; 44:405–13.
Article9. Ou M, Zhu J, Ji P, Li H, Zhong Z, Li B, et al. Risk factors of severe cases with COVID-19: a meta-analysis. Epidemiol Infect. 2020; 148:e175.
Article10. Cariou B, Hadjadj S, Wargny M, Pichelin M, Al-Salameh A, Allix I, et al. Phenotypic characteristics and prognosis of inpatients with COVID-19 and diabetes: the CORONADO study. Diabetologia. 2020; 63:1500–15.
Article11. Pedrosa AR, Martins DC, Rizzo M, Silva-Nunes J. Metformin in SARS-CoV-2 infection: a hidden path. From altered inflammation to reduced mortality. A review from the literature. J Diabetes Complications. 2023; 37:108391.12. Bonora BM, Avogaro A, Fadini GP. Disentangling conflicting evidence on DPP-4 inhibitors and outcomes of COVID-19: narrative review and meta-analysis. J Endocrinol Invest. 2021; 44:1379–86.
Article13. Han T, Ma S, Sun C, Zhang H, Qu G, Chen Y, et al. Association between anti-diabetic agents and clinical outcomes of COVID-19 in patients with diabetes: a systematic review and meta-analysis. Arch Med Res. 2022; 53:186–95.
Article14. Singh AK, Singh R, Saboo B, Misra A. Non-insulin anti-diabetic agents in patients with type 2 diabetes and COVID-19: a critical appraisal of literature. Diabetes Metab Syndr. 2021; 15:159–67.
Article15. Bramante CT, Huling JD, Tignanelli CJ, Buse JB, Liebovitz DM, Nicklas JM, et al. Randomized trial of metformin, ivermectin, and fluvoxamine for COVID-19. N Engl J Med. 2022; 387:599–610.
Article16. Reis G, Dos Santos Moreira Silva EA, Medeiros Silva DC, Thabane L, Cruz Milagres A, Ferreira TS, et al. Effect of early treatment with metformin on risk of emergency care and hospitalization among patients with COVID-19: the TOGETHER randomized platform clinical trial. Lancet Reg Health Am. 2022; 6:100142.
Article17. Ventura-Lopez C, Cervantes-Luevano K, Aguirre-Sanchez JS, Flores-Caballero JC, Alvarez-Delgado C, Bernaldez-Sarabia J, et al. Treatment with metformin glycinate reduces SARS-CoV-2 viral load: an in vitro model and randomized, double-blind, phase IIb clinical trial. Biomed Pharmacother. 2022; 152:113223.18. Guardado-Mendoza R, Garcia-Magana MA, Martinez-Navarro LJ, Macias-Cervantes HE, Aguilar-Guerrero R, Suarez-Perez EL, et al. Effect of linagliptin plus insulin in comparison to insulin alone on metabolic control and prognosis in hospitalized patients with SARS-CoV-2 infection. Sci Rep. 2022; 12:536.19. Abuhasira R, Ayalon-Dangur I, Zaslavsky N, Koren R, Keller M, Dicker D, et al. A randomized clinical trial of linagliptin vs. standard of care in patients hospitalized with diabetes and COVID-19. Front Endocrinol (Lausanne). 2021; 12:794382.20. Bae JH, Han KD, Ko SH, Yang YS, Choi JH, Choi KM, et al. Diabetes fact sheet in Korea 2021. Diabetes Metab J. 2022; 46:417–26.21. Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson comorbidity index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits. 2019; 12:188–97.22. Viollet B, Guigas B, Sanz Garcia N, Leclerc J, Foretz M, Andreelli F. Cellular and molecular mechanisms of metformin: an overview. Clin Sci (Lond). 2012; 122:253–70.
Article23. Kim MJ, Han JY, Shin JY, Kim SI, Lee JM, Hong S, et al. Metformin-associated lactic acidosis: predisposing factors and outcome. Endocrinol Metab (Seoul). 2015; 30:78–83.
Article24. Postler TS, Peng V, Bhatt DM, Ghosh S. Metformin selectively dampens the acute inflammatory response through an AMPK-dependent mechanism. Sci Rep. 2021; 11:18721.
Article25. Xin G, Wei Z, Ji C, Zheng H, Gu J, Ma L, et al. Metformin uniquely prevents thrombosis by inhibiting platelet activation and mtDNA release. Sci Rep. 2016; 6:36222.
Article26. Schaller MA, Sharma Y, Dupee Z, Nguyen D, Uruena J, Smolchek R, et al. Ex vivo SARS-CoV-2 infection of human lung reveals heterogeneous host defense and therapeutic responses. JCI Insight. 2021; 6:e148003.
Article27. Xian H, Liu Y, Rundberg Nilsson A, Gatchalian R, Crother TR, Tourtellotte WG, et al. Metformin inhibition of mitochondrial ATP and DNA synthesis abrogates NLRP3 inflammasome activation and pulmonary inflammation. Immunity. 2021; 54:1463–77.
Article28. Nafakhi H, Alareedh M, Al-Buthabhak K, Shaghee F, Nafakhi A, Kasim S. Predictors of adverse in-hospital outcome and recovery in patients with diabetes mellitus and COVID-19 pneumonia in Iraq. Diabetes Metab Syndr. 2021; 15:33–8.
Article29. Cheng X, Liu YM, Li H, Zhang X, Lei F, Qin JJ, et al. Metformin is associated with higher incidence of acidosis, but not mortality, in individuals with COVID-19 and pre-existing type 2 diabetes. Cell Metab. 2020; 32:537–47.
Article30. Gao Y, Liu T, Zhong W, Liu R, Zhou H, Huang W, et al. Risk of metformin in patients with type 2 diabetes with COVID-19: a preliminary retrospective report. Clin Transl Sci. 2020; 13:1055–9.
Article31. Broxmeyer HE, Capitano M, Campbell TB, Hangoc G, Cooper S. Modulation of hematopoietic chemokine effects in vitro and in vivo by DPP-4/CD26. Stem Cells Dev. 2016; 25:575–85.
Article32. Soare A, Gyorfi HA, Matei AE, Dees C, Rauber S, Wohlfahrt T, et al. Dipeptidylpeptidase 4 as a marker of activated fibroblasts and a potential target for the treatment of fibrosis in systemic sclerosis. Arthritis Rheumatol. 2020; 72:137–49.
Article33. Meyerholz DK, Lambertz AM, McCray PB. Dipeptidyl peptidase 4 distribution in the human respiratory tract: implications for the middle east respiratory syndrome. Am J Pathol. 2016; 186:78–86.34. Kawasaki T, Chen W, Htwe YM, Tatsumi K, Dudek SM. DPP4 inhibition by sitagliptin attenuates LPS-induced lung injury in mice. Am J Physiol Lung Cell Mol Physiol. 2018; 315:L834–45.
Article35. Quianzon CC, Cheikh IE. History of current non-insulin medications for diabetes mellitus. J Community Hosp Intern Med Perspect. 2012; 2:19081.
Article36. Hughes WT, Smith-McCain BL. Effects of sulfonylurea compounds on Pneumocystis carinii. J Infect Dis. 1986; 153:944–7.
Article37. Cama VF, Marin-Prida J, Acosta-Rivero N, Acosta EF, Diaz LO, Casadesus AV, et al. The microglial NLRP3 inflammasome is involved in human SARS-CoV-2 cerebral pathogenicity: a report of three post-mortem cases. J Neuroimmunol. 2021; 361:577728.
Article38. Yang X, Wang Z, Jia X. Neuroprotection of glibenclamide against brain injury after cardiac arrest via modulation of NLRP3 inflammasome. Annu Int Conf IEEE Eng Med Biol Soc. 2019; 2019:4209–12.
Article39. Esmaeili MH, Enayati M, Khabbaz Abkenar F, Ebrahimian F, Salari AA. Glibenclamide mitigates cognitive impairment and hippocampal neuroinflammation in rats with type 2 diabetes and sporadic Alzheimer-like disease. Behav Brain Res. 2020; 379:112359.
Article40. Dalan R, Ang LW, Tan WY, Fong SW, Tay WC, Chan YH, et al. The association of hypertension and diabetes pharmacotherapy with COVID-19 severity and immune signatures: an observational study. Eur Heart J Cardiovasc Pharmacother. 2021; 7:e48–51.
Article41. Nguyen NN, Ho DS, Nguyen HS, Ho DK, Li HY, Lin CY, et al. Preadmission use of antidiabetic medications and mortality among patients with COVID-19 having type 2 diabetes: a meta-analysis. Metabolism. 2022; 131:155196.
Article42. Chang MC, Hwang JM, Jeon JH, Kwak SG, Park D, Moon JS. Fasting plasma glucose level independently predicts the mortality of patients with coronavirus disease 2019 infection: a multicenter, retrospective cohort study. Endocrinol Metab (Seoul). 2020; 35:595–601.
Article43. Baek MS, Lee MT, Kim WY, Choi JC, Jung SY. COVID-19-related outcomes in immunocompromised patients: a nationwide study in Korea. PLoS One. 2021; 16:e0257641.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Effect of Hepatitis B Virus on COVID-19 Infected Patients: A Nationwide Population-Based Study Using the Health Insurance Review & Assessment Service Database
- The elderly population are more vulnerable for the management of colorectal cancer during the COVID-19 pandemic: a nationwide, population-based study
- Impact of the COVID-19 Pandemic on Esophagogastroduodenoscopy and Gastric Cancer Claims in South Korea: A Nationwide, Population-Based Study
- The impact of the COVID-19 pandemic on clinical practices related to colorectal cancer and colonoscopy in South Korea: a nationwide population-based study
- Clinical outcomes of COVID-19 amongst HIV patients: a systematic literature review