J Korean Foot Ankle Soc.
2024 Jun;28(2):60-67. 10.14193/jkfas.2024.28.2.60.
Various Pathologic Conditions of Sinus Tarsi Syndrome Assessed by Imaging and Arthroscopic Findings
- Affiliations
-
- 1Korea Armed Forces Athletic Corps, Mungyeong, Korea
- 2Department of Orthopedic Surgery, Yeungnam University Medical Center, Daegu, Korea
- 3Department of Orthopedic Surgery, College of Medicine, Yeungnam University, Daegu, Korea
- KMID: 2556555
- DOI: http://doi.org/10.14193/jkfas.2024.28.2.60
Abstract
- Purpose
Sinus tarsi syndrome (STS) is caused by various pathologies. However, the exact etiology of STS remains controversial. This study evaluated the imaging and arthroscopic findings of patients who underwent surgical treatment after conservative treatment for STS failed.
Materials and Methods
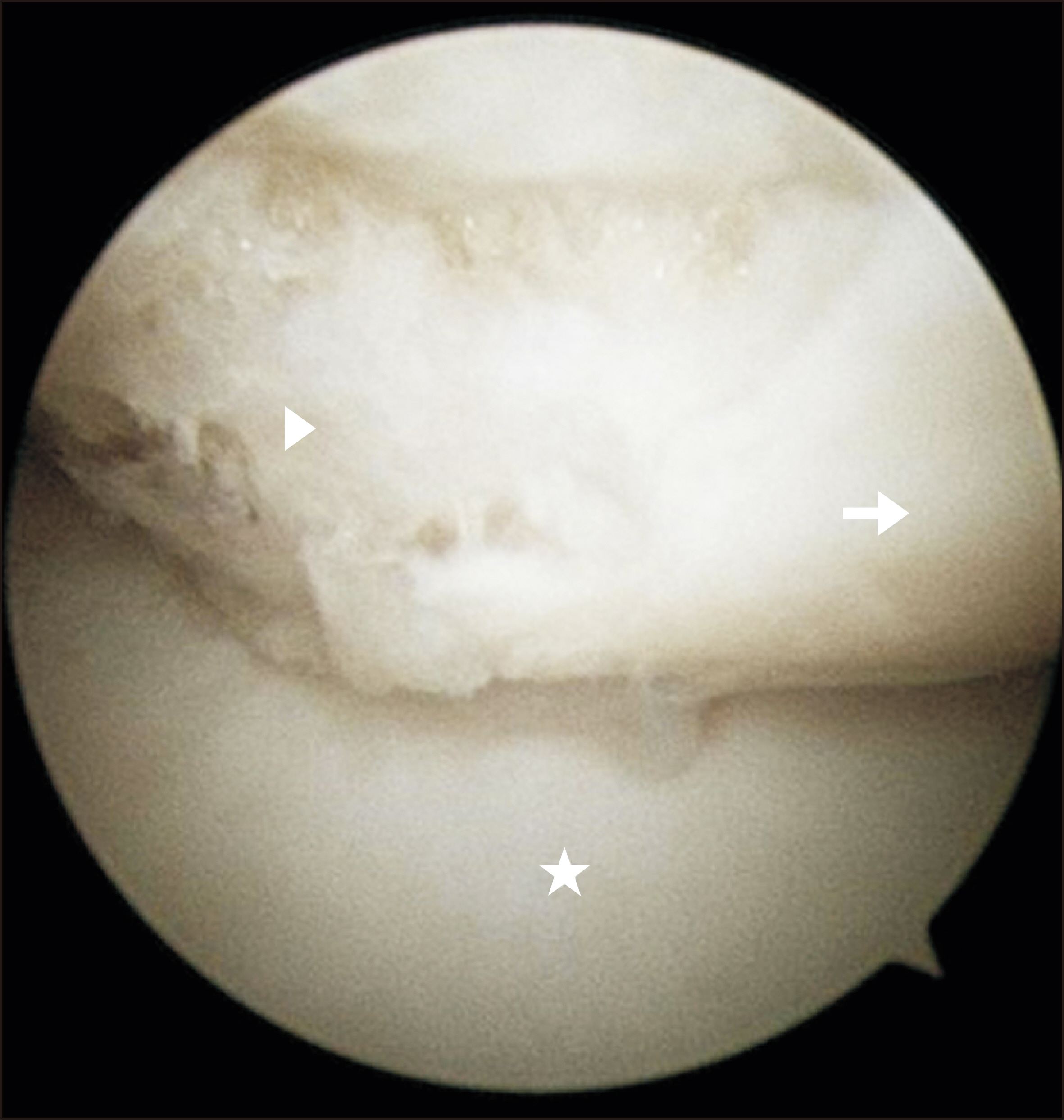
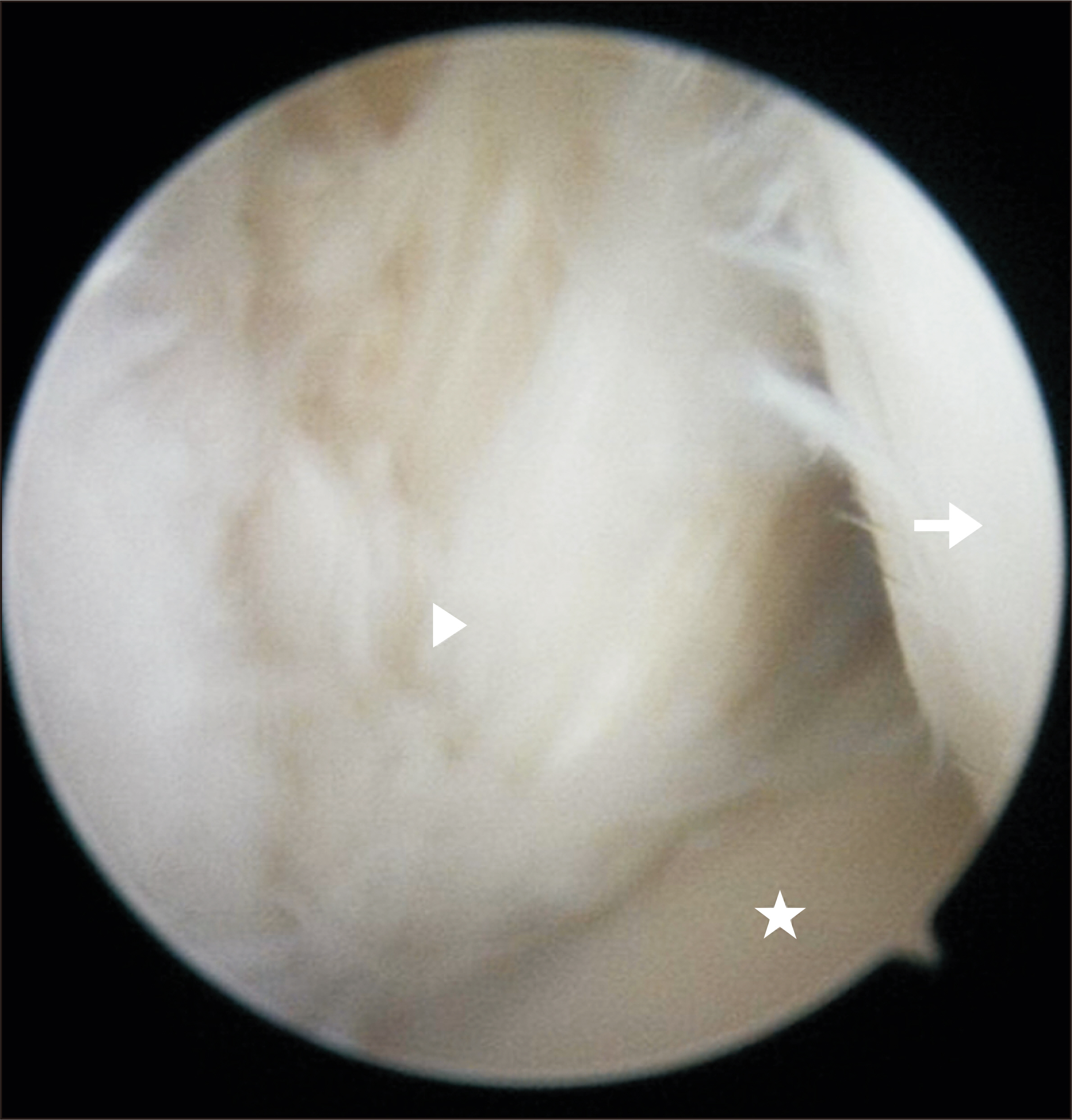
Between December 2014 and August 2018, 20 patients (21 cases) who underwent surgical treatment for STS were included in the study. The clinical results were analyzed using the visual analog scale (VAS) and the American Orthopedic Foot and Ankle Society (AOFAS) ankle-hindfoot functional scale. The radiographic results were analyzed using Meary’s angle, calcaneal pitch angle, and hindfoot alignment angle. The pathologic conditions of sinus tarsi were confirmed by magnetic resonance imaging (MRI) and subtalar arthroscopy. Synovitis, bone edema, and accessory anterolateral talar facet (AALTF) were evaluated on MRI. Synovial thickening, cartilage damage, interosseous talocalcaneal ligament (ITCL) and cervical ligament rupture, soft tissue impingement, AALTF, and accessory talar facet impingement (ATFI) were evaluated by subtalar arthroscopy.
Results
The mean duration of symptoms was 28.7 months (4~120). All patients showed significant improvement in the VAS and AOFAS ankle-hindfoot scale. Significant improvements in hindfoot alignment angle and Meary’s angle postoperatively were noted in patients who underwent medial displacement calcaneal osteotomy. MRI confirmed synovitis in all patients, AALTF in 19 cases (90.5%), and ATFI with bone edema in seven cases (33.3%). In subtalar arthroscopy, pathologic conditions were observed in the following order: synovitis in 21 cases (100%), AALTF in 20 cases (95.2%), ITCL partial rupture in nine cases (42.9%), and soft tissue impingement in seven cases (33.3%). All cases had two or more pathological conditions, and 15 (71.4%) had three or more.
Conclusion
In cases of STS that do not respond to conservative treatment, a comprehensive examination of the lesions of the tarsal sinus and lesions around the subtalar joint is essential.
Figure
Reference
-
1. Lee KB, Bai LB, Song EK, Jung ST, Kong IK. 2008; Subtalar arthroscopy for sinus Tarsi syndrome: arthroscopic findings and clinical outcomes of 33 consecutive cases. Arthroscopy. 24:1130–4. doi: 10.1016/j.arthro.2008.05.007. DOI: 10.1016/j.arthro.2008.05.007. PMID: 19028165.
Article2. Taillard W, Meyer JM, Garcia J, Blanc Y. 1981; The sinus tarsi syndrome. Int Orthop. 5:117–30. doi: 10.1007/BF00267842. DOI: 10.1007/BF00267842. PMID: 7275413.
Article3. Frey C, Feder KS, DiGiovanni C. 1999; Arthroscopic evaluation of the subtalar joint: does sinus tarsi syndrome exist? Foot Ankle Int. 20:185–91. doi: 10.1177/107110079902000309. DOI: 10.1177/107110079902000309. PMID: 10195298.
Article4. Oloff LM, Schulhofer SD, Bocko AP. 2001; Subtalar joint arthroscopy for sinus tarsi syndrome: a review of 29 cases. J Foot Ankle Surg. 40:152–7. doi: 10.1016/s1067-2516(01)80081-8. DOI: 10.1016/S1067-2516(01)80081-8. PMID: 11417597.
Article5. Beltran J. 1994; Sinus tarsi syndrome. Magn Reson Imaging Clin N Am. 2:59–65. doi: 10.1016/S1064-9689(21)00325-1. DOI: 10.1016/S1064-9689(21)00325-1. PMID: 7584239.
Article6. Klein MA, Spreitzer AM. 1993; MR imaging of the tarsal sinus and canal: normal anatomy, pathologic findings, and features of the sinus tarsi syndrome. Radiology. 186:233–40. doi: 10.1148/radiology.186.1.8416571. DOI: 10.1148/radiology.186.1.8416571. PMID: 8416571.
Article7. Lektrakul N, Chung CB, Lai Ym, Theodorou DJ, Yu J, Haghighi P, et al. 2001; Tarsal sinus: arthrographic, MR imaging, MR arthrographic, and pathologic findings in cadavers and retrospective study data in patients with sinus tarsi syndrome. Radiology. 219:802–10. doi: 10.1148/radiology.219.3.r01jn31802. DOI: 10.1148/radiology.219.3.r01jn31802. PMID: 11376274.
Article8. Frey C, Gasser S, Feder K. 1994; Arthroscopy of the subtalar joint. Foot Ankle Int. 15:424–8. doi: 10.1177/107110079401500804. DOI: 10.1177/107110079401500804. PMID: 7981813.
Article9. Mabit C, Boncoeur-Martel MP, Chaudruc JM, Valleix D, Descottes B, Caix M. 1997; Anatomic and MRI study of the subtalar ligamentous support. Surg Radiol Anat. 19:111–7. doi: 10.1007/BF01628135. DOI: 10.1007/BF01628135. PMID: 9210245.
Article10. Parisien JS, Vangsness T. 1985; Arthroscopy of the subtalar joint: an experimental approach. Arthroscopy. 1:53–7. doi: 10.1016/s0749-8063(85)80079-7. DOI: 10.1016/S0749-8063(85)80079-7. PMID: 4091910.
Article11. Pisani G, Pisani PC, Parino E. 2005; Sinus tarsi syndrome and subtalar joint instability. Clin Podiatr Med Surg. 22:63–77. viidoi: 10.1016/j.cpm.2004.08.005. DOI: 10.1016/j.cpm.2004.08.005. PMID: 15555844.
Article12. Aydıngöz Ü, Topcuoğlu OM, Görmez A, Cankurtaran T, Topcuoğlu ED, Ergen FB. 2016; Accessory anterolateral talar facet in populations with and without symptoms: prevalence and relevant associated ankle MRI findings. AJR Am J Roentgenol. 207:846–51. doi: 10.2214/AJR.16.16056. DOI: 10.2214/AJR.16.16056. PMID: 27504982.
Article13. Niki H, Hirano T, Akiyama Y, Beppu M. 2014; Accessory talar facet impingement in pathologic conditions of the peritalar region in adults. Foot Ankle Int. 35:1006–14. doi: 10.1177/1071100714540891. DOI: 10.1177/1071100714540891. PMID: 24962524.
Article14. Park JW, Park CH. 2018; Accessory talar facet impingement due to accessory anterolateral talar facet misdiagnosed as sinus tarsi syndrome. J Korean Foot Ankle Soc. 22:16–20. doi: 10.14193/jkfas.2018.22.1.16. DOI: 10.14193/jkfas.2018.22.1.16.
Article15. Park JW, Park J, Park CH. 2021; Accessory talar facet impingement and sinus tarsi pain associated with accessory anterolateral talar facet. Foot Ankle Int. 42:1060–7. doi: 10.1177/10711007211002115. DOI: 10.1177/10711007211002115. PMID: 34024149.
Article16. Zell BK, Shereff MJ, Greenspan A, Liebowitz S. 1986; Combined ankle and subtalar instability. Bull Hosp Jt Dis Orthop Inst. 46:37–46.17. Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, Myerson MS, Sanders M. 1994; Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 15:349–53. doi: 10.1177/107110079401500701. DOI: 10.1177/107110079401500701. PMID: 7951968.
Article18. Park CH, Lee WC. 2017; Donor site morbidity after lateral ankle ligament reconstruction using the anterior half of the peroneus longus tendon autograft. Am J Sports Med. 45:922–8. doi: 10.1177/0363546516675167. DOI: 10.1177/0363546516675167. PMID: 27899356.
Article19. Lee KB, Bai LB, Park JG, Song EK, Lee JJ. 2008; Efficacy of MRI versus arthroscopy for evaluation of sinus tarsi syndrome. Foot Ankle Int. 29:1111–6. doi: 10.3113/FAI.2008.1111. DOI: 10.3113/FAI.2008.1111. PMID: 19026205.
Article20. Arshad Z, Bhatia M. 2021; Current concepts in sinus tarsi syndrome: a scoping review. Foot Ankle Surg. 27:615–21. doi: 10.1016/j.fas.2020.08.013. DOI: 10.1016/j.fas.2020.08.013. PMID: 32978087.
Article21. Khan I, Peters J, Welck M, Saifuddin A. 2023; Sinus tarsi and sinus tarsi syndrome: an imaging review. Eur J Radiol. 161:110725. doi: 10.1016/j.ejrad.2023.110725. DOI: 10.1016/j.ejrad.2023.110725. PMID: 36773427.
Article22. Sarrafian SK. 1993; Biomechanics of the subtalar joint complex. Clin Orthop Relat Res. (290):17–26. doi: 10.1097/00003086-199305000-00003. DOI: 10.1097/00003086-199305000-00003.
Article23. Martus JE, Femino JE, Caird MS, Kuhns LR, Craig CL, Farley FA. 2008; Accessory anterolateral talar facet as an etiology of painful talocalcaneal impingement in the rigid flatfoot: a new diagnosis. Iowa Orthop J. 28:1–8.24. Landis JR, Koch GG. 1977; The measurement of observer agreement for categorical data. Biometrics. 33:159–74. doi: 10.2307/2529310. DOI: 10.2307/2529310. PMID: 843571.
Article25. Martus JE, Femino JE, Caird MS, Hughes RE, Browne RH, Farley FA. 2008; Accessory anterolateral facet of the pediatric talus. An anatomic study. J Bone Joint Surg Am. 90:2452–9. doi: 10.2106/JBJS.G.01230. DOI: 10.2106/JBJS.G.01230. PMID: 18978415.26. Hattori K, Sakuma E, Nakayama M, Kozaki A, Wada I, Otsuka T. 2015; An anatomic study of the accessory anterolateral talar facet. Folia Morphol (Warsz). 74:61–4. doi: 10.5603/FM.2015.0010. DOI: 10.5603/FM.2015.0010. PMID: 25792397.
Article27. Hirano T, Niki H, Akiyama Y, Beppu M. 2015; Anatomical characteristics of the accessory antero-lateral talar facet. J Orthop Sci. 20:124–8. doi: 10.1007/s00776-014-0649-5. DOI: 10.1007/s00776-014-0649-5. PMID: 25277070.
Article28. Akiyama K, Takakura Y, Tomita Y, Sugimoto K, Tanaka Y, Tamai S. 1999; Neurohistology of the sinus tarsi and sinus tarsi syndrome. J Orthop Sci. 4:299–303. doi: 10.1007/s007760050107. DOI: 10.1007/s007760050107. PMID: 10436278.
Article29. Kjaersgaard-Andersen P, Wethelund JO, Helmig P, Søballe K. 1988; The stabilizing effect of the ligamentous structures in the sinus and canalis tarsi on movements in the hindfoot. An experimental study. Am J Sports Med. 16:512–6. doi: 10.1177/036354658801600514. DOI: 10.1177/036354658801600514. PMID: 3189685.30. Mullen JE, O'Malley MJ. 2004; Sprains--residual instability of subtalar, Lisfranc joints, and turf toe. Clin Sports Med. 23:97–121. doi: 10.1016/S0278-5919(03)00089-9. DOI: 10.1016/S0278-5919(03)00089-9. PMID: 15062586.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Extensile Lateral Approach and Sinus Tarsi Approach for the Sanders Type II Calcaneal Fracture
- The Sinus Tarsi Approach for the Treatment of Intra-Articular Calcaneal Fractures
- “Locked-Lateral” Calcaneal Fracture-Dislocation Treated by Sinus Tarsi Approach
- Accessory Talar Facet Impingement due to Accessory Anterolateral Talar Facet Misdiagnosed as Sinus Tarsi Syndrome
- Intraoperative Arthroscopic Findings of Ulnar Impaction Syndrome