Korean Circ J.
2024 Jun;54(6):311-322. 10.4070/kcj.2023.0292.
Mitral Annular Tissue Velocity Predicts Survival in Patients With Primary Mitral Regurgitation
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 4Division of Cardiology, Department of Internal Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2556528
- DOI: http://doi.org/10.4070/kcj.2023.0292
Abstract
- Background and Objectives
Early diastolic mitral annular tissue (e’) velocity is a commonly used marker of left ventricular (LV) diastolic function. This study aimed to investigate the prognostic implications of e’ velocity in patients with mitral regurgitation (MR).
Methods
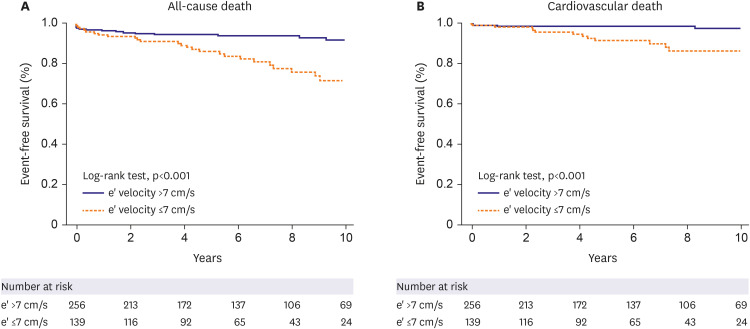
This retrospective cohort study included 1,536 consecutive patients aged <65 years with moderate or severe chronic primary MR diagnosed between 2009 and 2018. The primary and secondary outcomes were all-cause and cardiovascular mortality, respectively. According to the current guidelines, the cut-off value of e’ velocity was defined as 7 cm/s.
Results
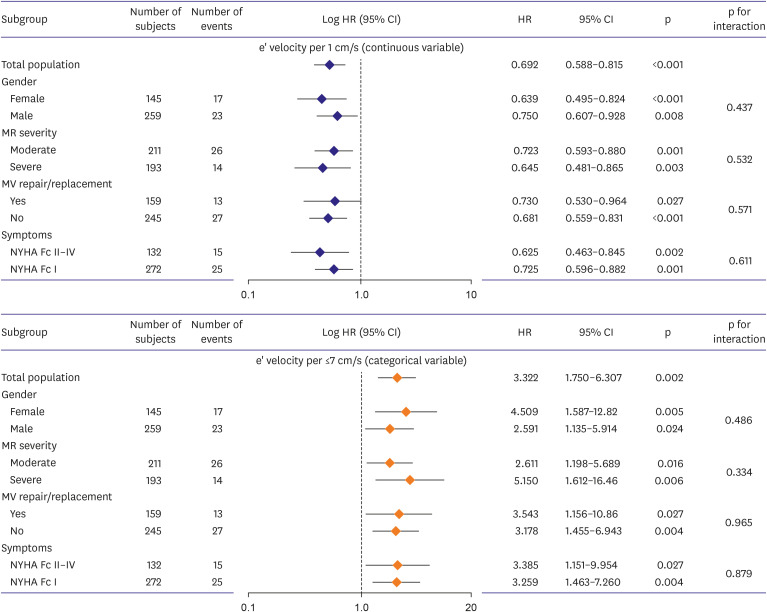
A total of 404 individuals were enrolled (median age, 51.0 years; 64.1% male; 47.8% severe MR). During a median 6.0-year follow-up, there were 40 all-cause mortality and 16 cardiovascular deaths. Multivariate analysis revealed a significant association between e’ velocity and all-cause death (adjusted hazard ratio [aHR], 0.770; 95% confidence interval [CI], 0.634–0.935; p=0.008) and cardiovascular death (aHR, 0.690; 95% CI, 0.477–0.998; p=0.049). Abnormal e’ velocity (≤7 cm/s) independently predicted all-cause death (aHR, 2.467; 95% CI, 1.170–5.200; p=0.018) and cardiovascular death (aHR, 5.021; 95% CI, 1.189–21.211; p=0.028), regardless of symptoms, LV dimension and ejection fraction. Subgroup analysis according to sex, MR severity, mitral valve replacement/repair, and symptoms, showed no significant interactions. Including e’ velocity in the 10-year risk score improved reclassification for mortality (net reclassification improvement [NRI], 0.154; 95% CI, 0.308– 0.910; p<0.001) and cardiovascular death (NRI, 1.018; 95% CI, 0.680–1.356; p<0.001).
Conclusions
In patients aged <65 years with primary MR, e’ velocity served as an independent predictor of all-cause and cardiovascular deaths.
Figure
Reference
-
1. Nkomo VT, Gardin JM, Skelton TN, Gottdiener JS, Scott CG, Enriquez-Sarano M. Burden of valvular heart diseases: a population-based study. Lancet. 2006; 368:1005–1011. PMID: 16980116.2. Goel SS, Bajaj N, Aggarwal B, et al. Prevalence and outcomes of unoperated patients with severe symptomatic mitral regurgitation and heart failure: comprehensive analysis to determine the potential role of MitraClip for this unmet need. J Am Coll Cardiol. 2014; 63:185–186. PMID: 24036029.3. Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022; 43:561–632. PMID: 34453165.4. Otto CM, Nishimura RA, Bonow RO, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: executive summary: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2021; 143:e35–e71. PMID: 33332149.5. Baumgartner H, Iung B, Otto CM. Timing of intervention in asymptomatic patients with valvular heart disease. Eur Heart J. 2020; 41:4349–4356. PMID: 32901279.6. Kim HM, Cho GY, Hwang IC, et al. Myocardial strain in prediction of outcomes after surgery for severe mitral regurgitation. JACC Cardiovasc Imaging. 2018; 11:1235–1244. PMID: 29778855.7. Choi YJ, Park J, Hwang D, et al. Network analysis of cardiac remodeling by primary mitral regurgitation emphasizes the role of diastolic function. JACC Cardiovasc Imaging. 2022; 15:974–986. PMID: 35680229.8. Olson JJ, Costa SP, Young CE, Palac RT. Early mitral filling/diastolic mitral annular velocity ratio is not a reliable predictor of left ventricular filling pressure in the setting of severe mitral regurgitation. J Am Soc Echocardiogr. 2006; 19:83–87. PMID: 16423674.9. Bruch C, Stypmann J, Gradaus R, Breithardt G, Wichter T. Usefulness of tissue Doppler imaging for estimation of filling pressures in patients with primary or secondary pure mitral regurgitation. Am J Cardiol. 2004; 93:324–328. PMID: 14759382.10. Rossi A, Cicoira M, Golia G, Anselmi M, Zardini P. Mitral regurgitation and left ventricular diastolic dysfunction similarly affect mitral and pulmonary vein flow Doppler parameters: the advantage of end-diastolic markers. J Am Soc Echocardiogr. 2001; 14:562–568. PMID: 11391284.11. Sohn DW, Chai IH, Lee DJ, et al. Assessment of mitral annulus velocity by Doppler tissue imaging in the evaluation of left ventricular diastolic function. J Am Coll Cardiol. 1997; 30:474–480. PMID: 9247521.12. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.e14. PMID: 25559473.13. Mitchell C, Rahko PS, Blauwet LA, et al. Guidelines for performing a comprehensive transthoracic echocardiographic examination in adults: recommendations from the American Society of Echocardiography. J Am Soc Echocardiogr. 2019; 32:1–64. PMID: 30282592.14. Zoghbi WA, Enriquez-Sarano M, Foster E, et al. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr. 2003; 16:777–802. PMID: 12835667.15. Nagueh SF, Smiseth OA, Appleton CP, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2016; 29:277–314. PMID: 27037982.16. Haruki N, Takeuchi M, Gerard O, et al. Accuracy of measuring mitral annular velocity by 2D speckle tracking imaging. J Cardiol. 2009; 53:188–195. PMID: 19304121.17. Grigioni F, Clavel MA, Vanoverschelde JL, et al. The MIDA mortality risk score: development and external validation of a prognostic model for early and late death in degenerative mitral regurgitation. Eur Heart J. 2018; 39:1281–1291. PMID: 29020352.18. Harrell FE. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. New York (NY): Springer International Publishing;2015.19. Suri RM, Vanoverschelde JL, Grigioni F, et al. Association between early surgical intervention vs watchful waiting and outcomes for mitral regurgitation due to flail mitral valve leaflets. JAMA. 2013; 310:609–616. PMID: 23942679.20. Corin WJ, Murakami T, Monrad ES, Hess OM, Krayenbuehl HP. Left ventricular passive diastolic properties in chronic mitral regurgitation. Circulation. 1991; 83:797–807. PMID: 1825625.21. Zaid RR, Barker CM, Little SH, Nagueh SF. Pre- and post-operative diastolic dysfunction in patients with valvular heart disease: diagnosis and therapeutic implications. J Am Coll Cardiol. 2013; 62:1922–1930. PMID: 24055747.22. Maganti K, Rigolin VH, Sarano ME, Bonow RO. Valvular heart disease: diagnosis and management. Mayo Clin Proc. 2010; 85:483–500. PMID: 20435842.23. Tsutsui H, Urabe Y, Mann DL, et al. Effects of chronic mitral regurgitation on diastolic function in isolated cardiocytes. Circ Res. 1993; 72:1110–1123. PMID: 8477523.24. Barbone A, Oz MC, Burkhoff D, Holmes JW. Normalized diastolic properties after left ventricular assist result from reverse remodeling of chamber geometry. Circulation. 2001; 104:I229–I232. PMID: 11568061.25. Borg AN, Harrison JL, Argyle RA, Pearce KA, Beynon R, Ray SG. Left ventricular filling and diastolic myocardial deformation in chronic primary mitral regurgitation. Eur J Echocardiogr. 2010; 11:523–529. PMID: 20185526.26. Hollingsworth KG, Blamire AM, Keavney BD, Macgowan GA. Left ventricular torsion, energetics, and diastolic function in normal human aging. Am J Physiol Heart Circ Physiol. 2012; 302:H885–H892. PMID: 22180656.27. Gao X, Jakovljevic DG, Beard DA. Cardiac metabolic limitations contribute to diminished performance of the heart in aging. Biophys J. 2019; 117:2295–2302. PMID: 31395314.28. Kitzman DW. Diastolic dysfunction in the elderly. Genesis and diagnostic and therapeutic implications. Cardiol Clin. 2000; 18:597–617. PMID: 10986592.29. Yamada H, Oki T, Mishiro Y, et al. Effect of aging on diastolic left ventricular myocardial velocities measured by pulsed tissue Doppler imaging in healthy subjects. J Am Soc Echocardiogr. 1999; 12:574–581. PMID: 10398916.30. Markar SR, Sadat U, Edmonds L, Nair SK. Mitral valve repair versus replacement in the elderly population. J Heart Valve Dis. 2011; 20:265–271. PMID: 21714415.31. Mitter SS, Shah SJ, Thomas JD. A test in context: E/A and E/e′ to assess diastolic dysfunction and LV filling pressure. J Am Coll Cardiol. 2017; 69:1451–1464. PMID: 28302294.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Echocardiographic Assessment of Mitral Valve Regurgitation
- Abnormal Mitral Regurgitation Flow Velocity Spectra by Continuous Wave Doppler in Flail Mitral Valve
- Assessment of Mitral Stenosis by Doppler Echocardiography: Influence of Regurgitation on Doppler Pressure Half-Time
- Mitral Valve Repair for Barlow’s Disease with Mitral Annular and Subvalvular Calcification: A Case Report
- Mitral Valve Replacement for Bulky, Calcified Mitral Annulus: A Case Report