Arch Hand Microsurg.
2024 Jun;29(2):110-115. 10.12790/ahm.24.0017.
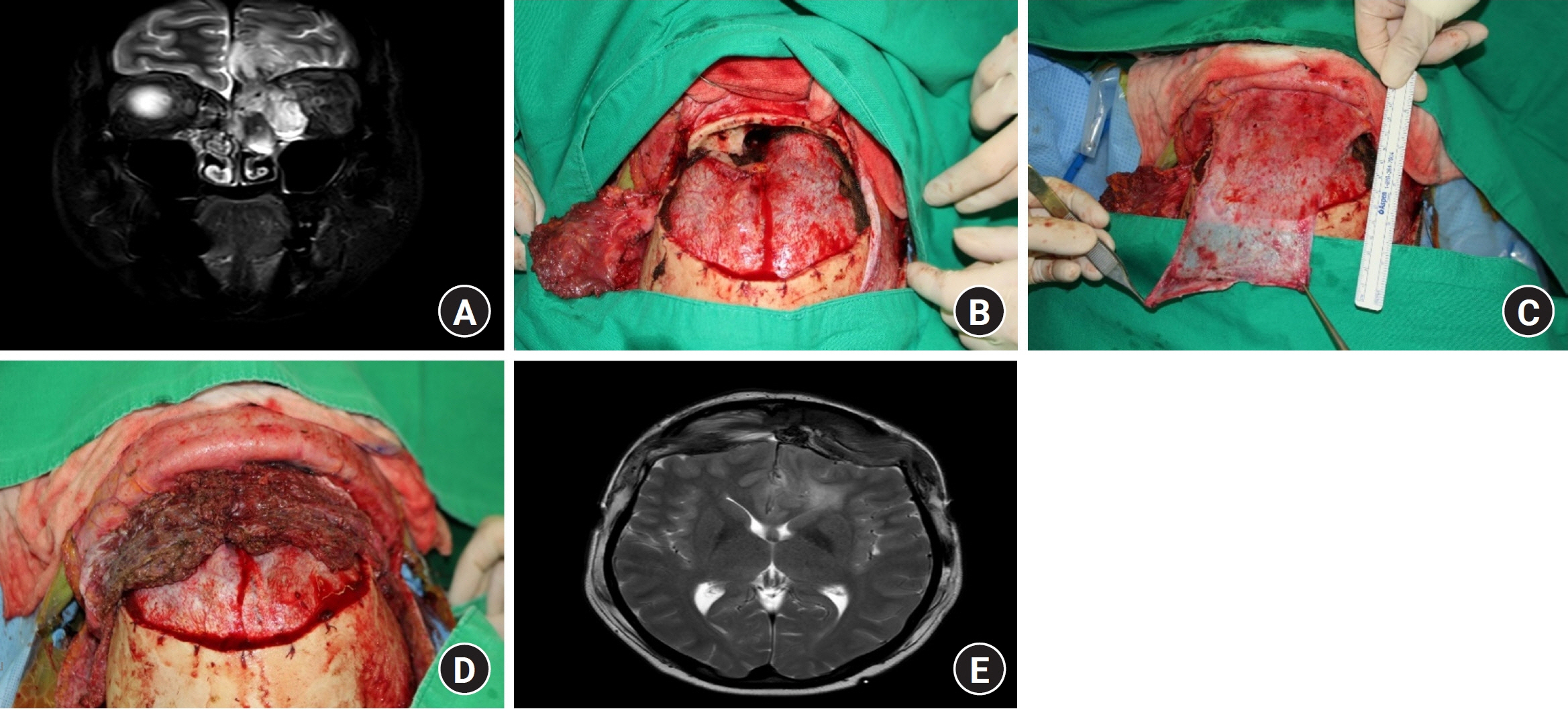
Reconstruction methods for large cranial-nasal communications: surgeons’ concerns about proper anterior skull base reconstruction
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Yonsei University College of Medicine, Seoul, Korea
- 2Institute for Human Tissue Restoration, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2556361
- DOI: http://doi.org/10.12790/ahm.24.0017
Abstract
- Purpose
Skull base reconstruction is one of the most difficult reconstructive surgical procedures. Due to its complexity, most surgeons have modified the reconstruction methods to minimize the postoperative complications and mortality rate. In the past, flap surgery was not usually performed, but it has recently become more common due to advances in medicine. In this study, we analyzed successful flap surgery methods in skull base reconstruction for large cranial-nasal communications.
Methods
Patients who underwent skull base reconstruction from April 2015 to January 2024 were eligible for this study. Of these patients, we included those who underwent reconstruction using a volumetric flap. Reconstructions that only used the conventional galeal flap, allograft skin, or bone substitute were excluded. The reconstruction methods used local flaps and free flaps.
Results
In total, 22 patients underwent skull base reconstruction. The most frequently used local flap was the bilateral reverse temporalis muscle flap (seven of 11 cases), and the most frequent free flap was the anterior lateral thigh flap (10 of 11 cases). Other local flap operations used the modified temporalis muscle flap and scalp flap. A rectus myocutaneous flap was also used. There were no cases of flap necrosis.
Conclusion
Flap surgery is needed for skull base reconstruction in patients with large cranial-nasal communications. As long as the flap volume is large enough to block and fill the defect, either a local flap or a free flap can be used for reconstruction.
Figure
Reference
-
References
1. Kwon SG, Kim YO, Rah DK. Anterior cranial base reconstruction with a reverse temporalis muscle flap and calvarial bone graft. Arch Plast Surg. 2012; 39:345–51.
Article2. Liu JK, Niazi Z, Couldwell WT. Reconstruction of the skull base after tumor resection: an overview of methods. Neurosurg Focus. 2002; 12:e9.
Article3. Bell EB, Cohen ER, Sargi Z, Leibowitz J. Free tissue reconstruction of the anterior skull base: a review. World J Otorhinolaryngol Head Neck Surg. 2020; 6:132–6.
Article4. Won J, Hong JW, Kim MJ, et al. Methodology in conventional head and neck reconstruction following robotic cancer surgery: a bridgehead robotic head and neck reconstruction. Yonsei Med J. 2022; 63:759–66.
Article5. Garcia-Navarro V, Anand VK, Schwartz TH. Gasket seal closure for extended endonasal endoscopic skull base surgery: efficacy in a large case series. World Neurosurg. 2013; 80:563–8.
Article6. Pusic AL, Chen CM, Patel S, Cordeiro PG, Shah JP. Microvascular reconstruction of the skull base: a clinical approach to surgical defect classification and flap selection. Skull Base. 2007; 17:5–15.
Article7. Hoffmann TK, El Hindy N, Müller OM, et al. Vascularised local and free flaps in anterior skull base reconstruction. Eur Arch Otorhinolaryngol. 2013; 270:899–907.
Article8. Ein L, Sargi Z, Nicolli EA. Update on anterior skull base reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2019; 27:426–30.
Article9. Wang W, Vincent A, Sokoya M, Kohlert S, Kadakia S, Ducic Y. Free-flap reconstruction of skull base and orbital defects. Semin Plast Surg. 2019; 33:72–7.
Article10. Moyer JS, Chepeha DB, Teknos TN. Contemporary skull base reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2004; 12:294–9.
Article11. Imola MJ, Sciarretta V, Schramm VL. Skull base reconstruction. Curr Opin Otolaryngol Head Neck Surg. 2003; 11:282–90.
Article12. Shin D, Yang CE, Kim YO, et al. Huge anterior skull base defect reconstruction on communicating between cranium and nasal cavity: combination flap of galeal flap and reverse temporalis flap. J Craniofac Surg. 2020; 31:436–9.
Article13. Yong M, Wu YQ, Su S, et al. The effect of prior radiation on the success of ventral skull base reconstruction: a systematic review and meta-analysis. Head Neck. 2021; 43:2795–806.
Article14. Hanasono MM, Silva A, Skoracki RJ, et al. Skull base reconstruction: an updated approach. Plast Reconstr Surg. 2011; 128:675–86.15. Soudry E, Psaltis AJ, Lee KH, Vaezafshar R, Nayak JV, Hwang PH. Complications associated with the pedicled nasoseptal flap for skull base reconstruction. Laryngoscope. 2015; 125:80–5.
Article16. Eldaly A, Magdy EA, Nour YA, Gaafar AH. Temporalis myofascial flap for primary cranial base reconstruction after tumor resection. Skull Base. 2008; 18:253–63.
Article17. Mady LJ, Kaffenberger TM, Baddour K, et al. Anatomic considerations of microvascular free tissue transfer in endoscopic endonasal skull base surgery. J Neurol Surg B Skull Base. 2022; 83:e143–51.
Article18. Patel MR, Shah RN, Snyderman CH, et al. Pericranial flap for endoscopic anterior skull-base reconstruction: clinical outcomes and radioanatomic analysis of preoperative planning. Neurosurgery. 2010; 66:506–12.19. Atabey A, Vayvada H, Menderes A, Kirişoğlu U, Barutçu A. A combined reverse temporalis muscle flap and pericranial flap for reconstruction of an anterior cranial base defect: a case report. Ann Plast Surg. 1997; 39:190–2.
Article20. Guinto G, Guinto Y. Reconstruction techniques in skull base surgery. World Neurosurg. 2015; 83:17–8.
Article21. Nameki H, Kato T, Nameki I, Ajimi Y. Selective reconstructive options for the anterior skull base. Int J Clin Oncol. 2005; 10:223–8.
Article22. Kim SH, Lee WJ, Chang JH, et al. Anterior skull base reconstruction using an anterolateral thigh free flap. Arch Craniofac Surg. 2021; 22:232–8.
Article23. Kwon D, Iloreta A, Miles B, Inman J. Open anterior skull base reconstruction: a contemporary review. Semin Plast Surg. 2017; 31:189–96.
Article24. Hanasono MM, Utley DS, Goode RL. The temporalis muscle flap for reconstruction after head and neck oncologic surgery. Laryngoscope. 2001; 111:1719–25.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Reconstruction of a skull base defect with cutaneous nasocranial communication using a combination of an anterolateral thigh free flap and galeal flap division: a case report
- Reconstruction of Anterior Skull Base Fracture Using Autologous Fractured Fragments: A Simple Stitching-Up Technique
- Endoscopic Skull Reconstruction: Nasoseptal Flap Based Reconstructive Options
- Reconstruction Strategy After Endoscopic Skull-Base Surgery
- Extended temporalis flap for skull base reconstruction