Arch Hand Microsurg.
2024 Jun;29(2):82-89. 10.12790/ahm.24.0009.
A comparative analysis of antegrade and retrograde Kirschner wire fixation for proximal phalanx base fractures
- Affiliations
-
- 1Department of Plastic and Reconstructive Surgery, Gwangmyeong Sungae General Hospital, Gwangmyeong, Korea
- KMID: 2556357
- DOI: http://doi.org/10.12790/ahm.24.0009
Abstract
- Purpose
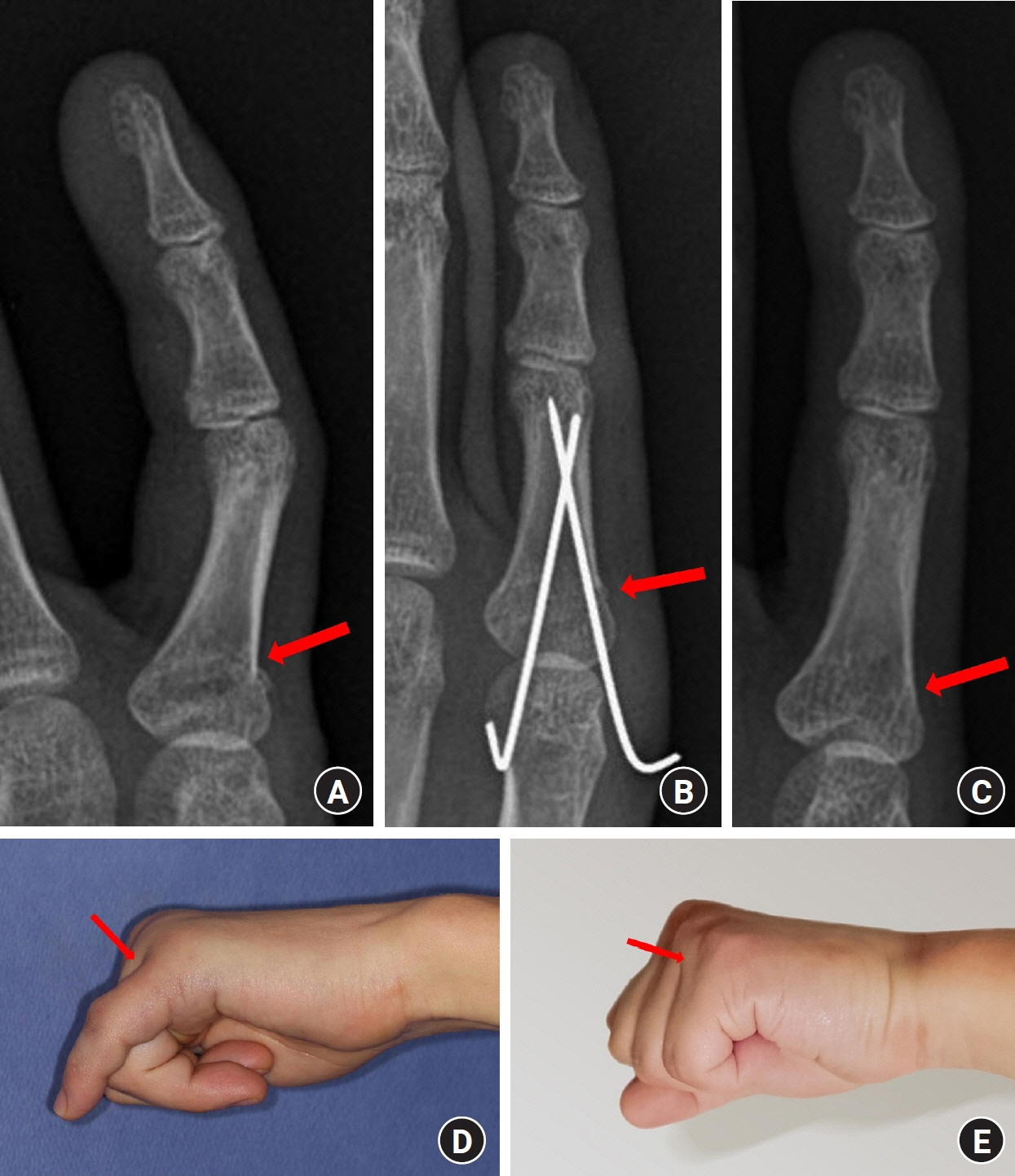
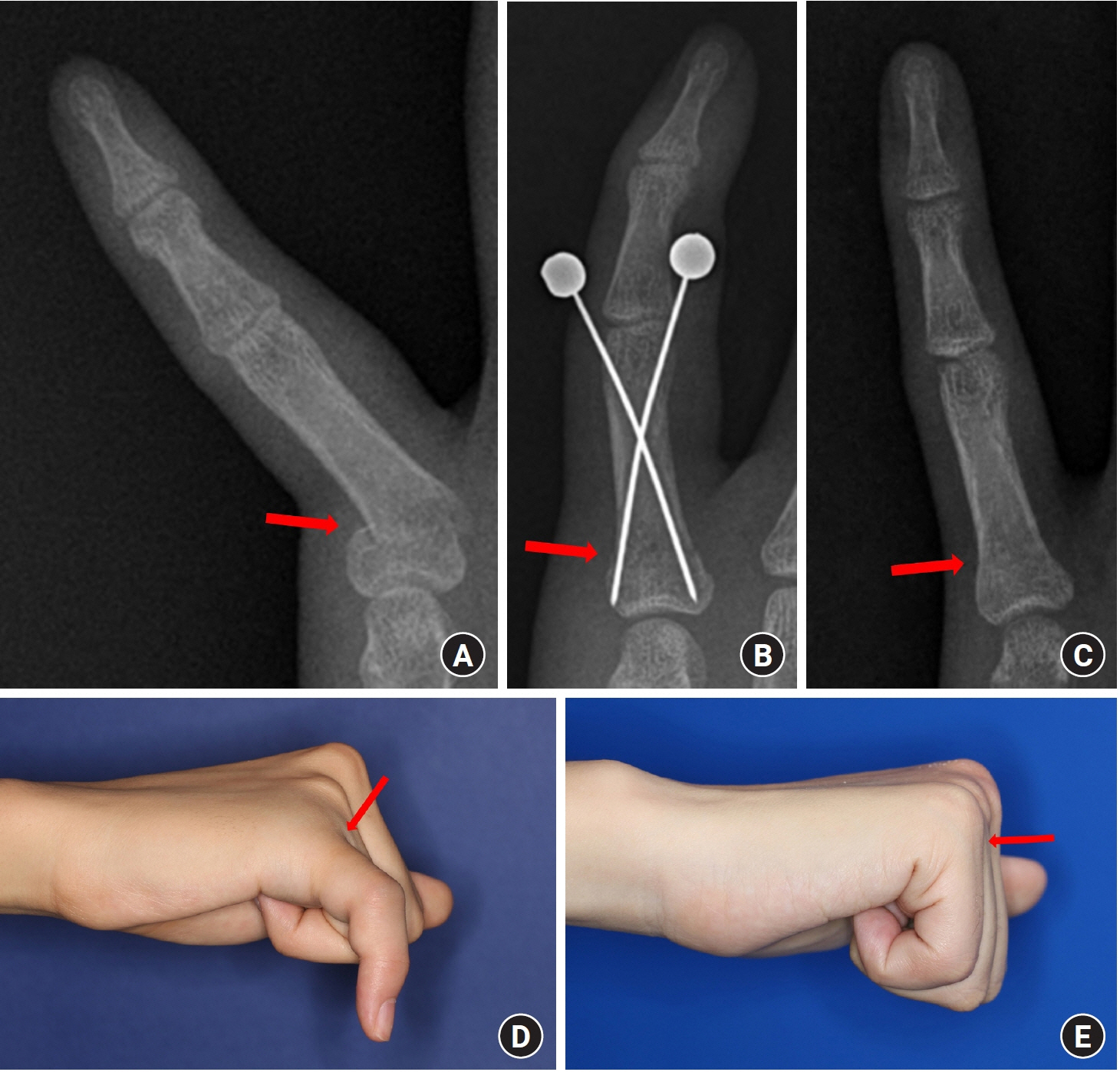
We aimed to determine whether the clinical outcomes of antegrade and retrograde extra-articular Kirschner wire (K-wire) pinning differed in proximal phalanx base fractures.
Methods
This retrospective study investigated 73 patients aged ≥18 years with extra-articular proximal phalanx base fractures that were treated by closed K-wire pinning between January 2014 and June 2023. Patients were analyzed according to whether the K-wire fixation was antegrade or retrograde. We analyzed demographics, injury characteristics, the number of K-wires applied, surgical duration, the interval before implant removal, and when physical therapy was started. Radiological outcomes included the amount of time required for radiographically confirmed bone union. Clinical outcomes consisted of complications, total active motion (TAM), and the Michigan Hand Outcomes Questionnaire (MHQ).
Results
We treated 29 and 44 patients using antegrade and retrograde K-wire fixation, respectively. The overall complication rate was higher in the antegrade group than in the retrograde group (13.8% vs. 9.1%), although this difference was not statistically significant. Similarly, no significant between-group differences were detected in the length of time required for bone union and implant removal, TAM, and MHQ scores.
Conclusion
Proximal phalanx base fractures were equally and effectively treated by antegrade and retrograde K-wire fixation. Therefore, the direction of K-wire fixation can be chosen based on surgeons’ preferences and experience.
Figure
Reference
-
References
1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001; 26:908–15.
Article2. van Onselen EB, Karim RB, Hage JJ, Ritt MJ. Prevalence and distribution of hand fractures. J Hand Surg Br. 2003; 28:491–5.
Article3. Ip WY, Ng KH, Chow SP. A prospective study of 924 digital fractures of the hand. Injury. 1996; 27:279–85.
Article4. Windolf J, Siebert H, Werber KD, Schädel-Höpfner M. Treatment of phalangeal fractures: recommendations of the Hand Surgery Group of the German Trauma Society. Unfallchirurg. 2008; 111:331–8.5. Kozin SH, Thoder JJ, Lieberman G. Operative treatment of metacarpal and phalangeal shaft fractures. J Am Acad Orthop Surg. 2000; 8:111–21.
Article6. Singh J, Jain K, Mruthyunjaya P, Ravishankar R. Outcome of closed proximal phalangeal fractures of the hand. Indian J Orthop. 2011; 45:432–8.
Article7. Heifner JJ, Rubio F. Fractures of the phalanges. J Hand Surg Eur Vol. 2023; 48(2 Suppl):18S–26S.
Article8. Belsky MR, Eaton RG, Lane LB. Closed reduction and internal fixation of proximal phalangeal fractures. J Hand Surg Am. 1984; 9:725–9.
Article9. Faruqui S, Stern PJ, Kiefhaber TR. Percutaneous pinning of fractures in the proximal third of the proximal phalanx: complications and outcomes. J Hand Surg Am. 2012; 37:1342–8.
Article10. Day C, Stern PJ. Fractures of the metacarpals and phalanges. In : Wolfe SW, Hotchkiss RN, Pederson WC, editors. Green’s operative hand surgery. 6th ed. Philadelphia, PA: Elsevier/Churchill Livingstone;2011. p. 239–90.11. Rajesh G, Ip WY, Chow SP, Fung BK. Dynamic treatment for proximal phalangeal fracture of the hand. J Orthop Surg (Hong Kong). 2007; 15:211–5.
Article12. Dijkman BG, Sprague S, Schemitsch EH, Bhandari M. When is a fracture healed? Radiographic and clinical criteria revisited. J Orthop Trauma. 2010; 24 Suppl 1:S76–80.
Article13. Onishi T, Omokawa S, Shimizu T, Fujitani R, Shigematsu K, Tanaka Y. Predictors of postoperative finger stiffness in unstable proximal phalangeal fractures. Plast Reconstr Surg Glob Open. 2015; 3:e431.
Article14. Chung KC, Hamill JB, Walters MR, Hayward RA. The Michigan Hand Outcomes Questionnaire (MHQ): assessment of responsiveness to clinical change. Ann Plast Surg. 1999; 42:619–22.
Article15. Horton TC, Hatton M, Davis TR. A prospective randomized controlled study of fixation of long oblique and spiral shaft fractures of the proximal phalanx: closed reduction and percutaneous Kirschner wiring versus open reduction and lag screw fixation. J Hand Surg Br. 2003; 28:5–9.
Article16. Lögters TT, Lee HH, Gehrmann S, Windolf J, Kaufmann RA. Proximal phalanx fracture management. Hand (N Y). 2018; 13:376–83.
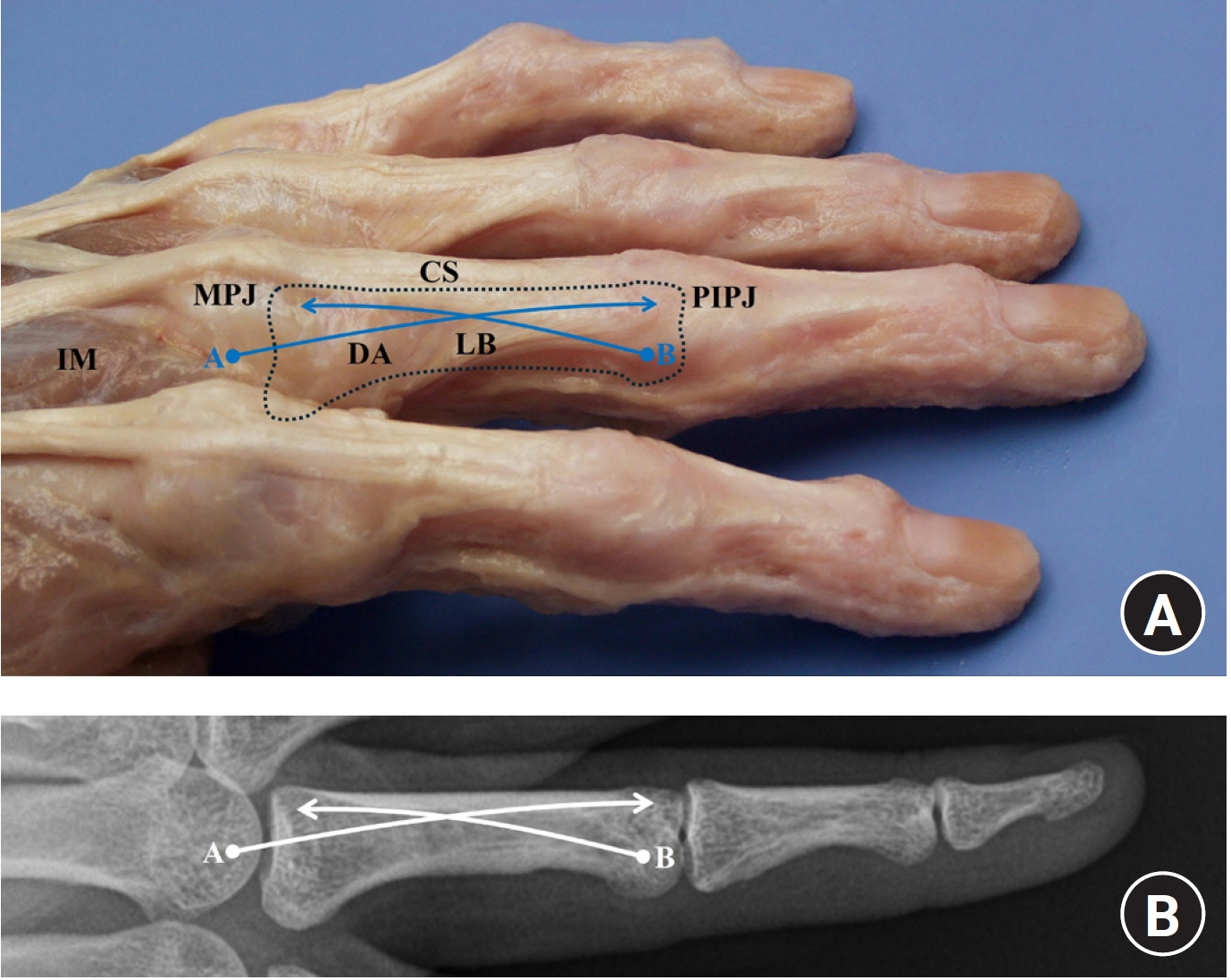
Article17. Gordon J, Andring N, Iannuzzi NP. K-wire fixation of metacarpal and phalangeal fractures: association between superficial landmarks and penetration of structures surrounding the metacarpophalangeal joint. J Hand Surg Glob Online. 2019; 1:214–7.
Article18. Sela Y, Peterson C, Baratz ME. Tethering the extensor apparatus limits pip flexion following K-wire placement for pinning extra-articular fractures at the base of the proximal phalanx. Hand (N Y). 2016; 11:433–7.
Article19. Dick H, Carlson E. Fractures of the fingers and thumb. In : Grabb WC, Smith JW, Aston SJ, editors. Grabb and Smith’s plastic surgery. 4th ed. Boston, MA: Little, Brown & Company;1991. p. 909–16.20. Lalonde D, Ayhan E, Ahmad AA, Koehler S. Important updates of finger fractures, entrapment neuropathies and wide-awake surgery of the upper extremity. J Hand Surg Eur Vol. 2022; 47:24–30.
Article21. Lalonde D. Preferred methods which are against traditional teachings. J Hand Surg Eur Vol. 2021; 46:327–30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative study on Kirschner-wire and screw fixation for intra-articular fractures of the proximal phalanx head
- Comparison between Two Kirschner Wire Fixation and Three Wire Fixation, in Treating of Metacarpal Neck Fracture Using Multiple Retrograde Kirschner Wire Fixation
- Treatment of Metacarpal Shaft Fractures with Retrograde Intramedullary Kirschner-Wire Fixation
- Kirschner Wire Fixation for Immobilization of the Thenar Flap in an Uncooperative Pediatric Patient: A Case Report
- Treatment of the Clavicle Lateral End Fracture by Kirschner wire and Wire fixation