Ann Surg Treat Res.
2024 Jun;106(6):344-353. 10.4174/astr.2024.106.6.344.
Comparison between intermittent claudication versus chronic limb-threatening ischemia in peripheral arterial disease: a retrospective multicenter cohort study
- Affiliations
-
- 1Department of Surgery, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Surgery, Kyung Hee University Hospital, Seoul, Korea
- 3Department of Surgery, Gachon University Gil Medical Center, Inchon, Korea
- 4Department of Surgery, Chosun University College of Medicine, Gwangju, Korea
- 5Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2556326
- DOI: http://doi.org/10.4174/astr.2024.106.6.344
Abstract
- Purpose
The anatomical distribution, characteristics of lesions, and treatment modalities for peripheral artery disease (PAD) are diverse. Endovascular intervention is popular for symptomatic PAD, for both intermittent claudication (IC) and chronic limb-threatening ischemia (CLTI). We aimed to investigate the endovascular devices used by comparing patients with PAD referred for endovascular revascularization with IC and CLTI.
Methods
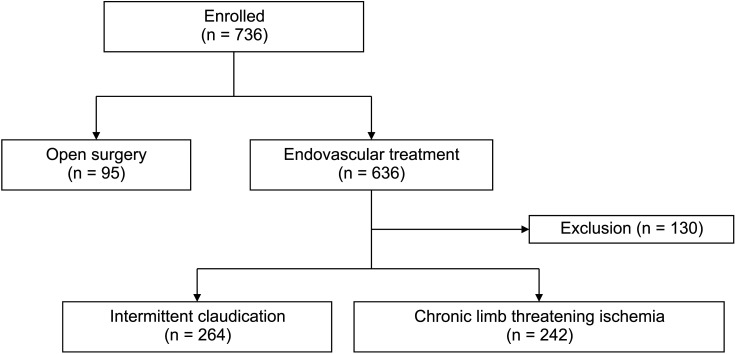
We identified 736 patients with PAD enrolled in the multicenter PAD registry in South Korea from 2019 to 2022. Of these patients, 636 received endovascular treatment at the time of this study. After excluding missing data, we analyzed 506 patients with IC or CLTI. Patients’ characteristics, target lesions, and endovascular device data such as type, length, balloon diameter, and stent, were examined. Procedure outcomes of the aortoiliac, femoropopliteal, and below-the-knee lesions were analyzed.
Results
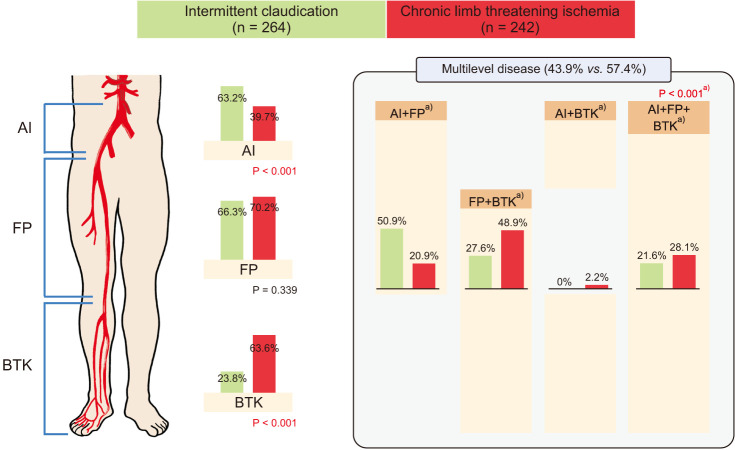
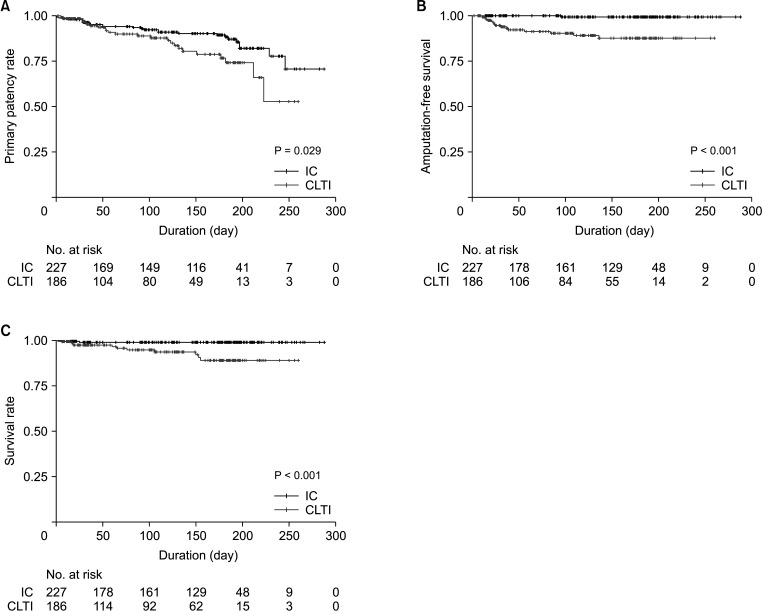
Patients with CLTI were more likely to have diabetes mellitus, below-the-knee interventions, and multilevel PAD than the IC group. Patients with IC had more aortoiliac artery lesions and underwent atherectomies than the CLTI group (63.3% and 61.1% vs. 39.7% and 40.6%, respectively; P < 0.001). In patients with femoropopliteal lesions, those with CLTI were more revascularized with stents than the patients with IC, without significant differences (35.3% vs. 29.1%, P = 0.161). Compared to the IC group, the CLTI patients showed significantly worse rates of primary patency, amputation, and mortality (P = 0.029, P < 0.001, and P < 0.001, respectively).
Conclusion
Among Korean patients with PAD, there is a significant difference in baseline and lesion characteristics, endovascular strategies, and short-term follow-up outcomes among those with IC and CLTI.
Keyword
Figure
Reference
-
1. Criqui MH, Aboyans V. Epidemiology of peripheral artery disease. Circ Res. 2015; 116:1509–1526. PMID: 25908725.2. Song P, Rudan D, Zhu Y, Fowkes FJ, Rahimi K, Fowkes FG, et al. Global, regional, and national prevalence and risk factors for peripheral artery disease in 2015: an updated systematic review and analysis. Lancet Glob Health. 2019; 7:e1020–e1030. PMID: 31303293.3. Bauersachs R, Brodmann M, Clark C, Debus S, De Carlo M, Gomez-Cerezo JF, et al. International public awareness of peripheral artery disease. Vasa. 2021; 50:294–300. PMID: 33645232.4. Aboyans V, Ricco JB, Bartelink ME, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J. 2018; 39:763–816. PMID: 28886620.5. Gerhard-Herman MD, Gornik HL, Barrett C, Barshes NR, Corriere MA, Drachman DE, et al. 2016 AHA/ACC Guideline on the management of patients with lower extremity peripheral artery disease: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2017; 135:e686–e725. PMID: 27840332.6. Hong MS, Beck AW, Nelson PR. Emerging national trends in the management and outcomes of lower extremity peripheral arterial disease. Ann Vasc Surg. 2011; 25:44–54. PMID: 21172580.7. Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FG, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J Vasc Surg. 2007; 45 Suppl S:S5–S67. PMID: 17223489.8. Fowkes FG, Rudan D, Rudan I, Aboyans V, Denenberg JO, McDermott MM, et al. Comparison of global estimates of prevalence and risk factors for peripheral artery disease in 2000 and 2010: a systematic review and analysis. Lancet. 2013; 382:1329–1340. PMID: 23915883.9. Ogurtsova K, da Rocha Fernandes JD, Huang Y, Linnenkamp U, Guariguata L, Cho NH, et al. IDF Diabetes Atlas: global estimates for the prevalence of diabetes for 2015 and 2040. Diabetes Res Clin Pract. 2017; 128:40–50. PMID: 28437734.10. Prasad N, Jha V. Hemodialysis in Asia. Kidney Dis (Basel). 2015; 1:165–177. PMID: 27536677.11. Soon SX, Patel A, Chong TT, Yap CJ, Tay HT, Tay KH, et al. Distribution of peripheral arterial disease in patients undergoing endovascular revascularization for chronic limb threatening ischaemia: insights from the Vascular Quality Initiative in Singapore. Vasc Specialist Int. 2021; 37:13. PMID: 34112741.12. Chen P, Patel PB, Ding J, Krimbill J, Siracuse JJ, O’Donnell TF, et al. Asian race is associated with peripheral arterial disease severity and postoperative outcomes. J Vasc Surg. 2023; 78:175–183. PMID: 36889608.13. Arya S, Binney Z, Khakharia A, Brewster LP, Goodney P, Patzer R, et al. Race and socioeconomic status independently affect risk of major amputation in peripheral artery disease. J Am Heart Assoc. 2018; 7:e007425. PMID: 29330260.14. Hicks CW, Wang P, Bruhn WE, Abularrage CJ, Lum YW, Perler BA, et al. Race and socioeconomic differences associated with endovascular peripheral vascular interventions for newly diagnosed claudication. J Vasc Surg. 2020; 72:611–621. PMID: 31902593.15. Hughes K, Sehgal N. Racial/ethnic disparities in lower extremity amputation vs revascularization: a brief review. J Natl Med Assoc. 2018; 110:560–563. PMID: 30129498.16. Paro A, Hyer JM, Diaz A, Tsilimigras DI, Pawlik TM. Profiles in social vulnerability: the association of social determinants of health with postoperative surgical outcomes. Surgery. 2021; 170:1777–1784. PMID: 34183179.17. Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL, et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation. 2006; 113:e463–e654. PMID: 16549646.18. The Korea Disease Control and Prevention Agency. Chronic disease statistics: current smoking rate trends, 2010-2020. Public Health Weekly Rep. 2022; 15:1485–1486.19. Farber A, Eberhardt RT. The current state of critical limb ischemia: a systematic review. JAMA Surg. 2016; 151:1070–1077. PMID: 27551978.20. Howard DP, Banerjee A, Fairhead JF, Hands L, Silver LE, Rothwell PM, et al. Population-based study of incidence, risk factors, outcome, and prognosis of ischemic peripheral arterial events: implications for prevention. Circulation. 2015; 132:1805–1815. PMID: 26350058.21. Ko YG, Ahn CM, Min PK, Lee JH, Yoon CH, Yu CW, et al. Baseline characteristics of a retrospective patient cohort in the Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases (K-VIS ELLA) Registry. Korean Circ J. 2017; 47:469–476. PMID: 28765738.22. Varu VN, Hogg ME, Kibbe MR. Critical limb ischemia. J Vasc Surg. 2010; 51:230–241. PMID: 20117502.23. Duni A, Liakopoulos V, Roumeliotis S, Peschos D, Dounousi E. Oxidative stress in the pathogenesis and evolution of chronic kidney disease: untangling Ariadne’s thread. Int J Mol Sci. 2019; 20:3711. PMID: 31362427.24. Hu CT, Shao YD, Liu YZ, Xiao X, Cheng ZB, Qu SL, et al. Oxidative stress in vascular calcification. Clin Chim Acta. 2021; 519:101–110. PMID: 33887264.25. Bosch JL, Hunink MG. Meta-analysis of the results of percutaneous transluminal angioplasty and stent placement for aortoiliac occlusive disease. Radiology. 1997; 204:87–96. PMID: 9205227.26. Banerjee S, Jeon-Slaughter H, Armstrong EJ, Bajzer C, Abu-Fadel M, Khalili H, et al. Clinical outcomes and cost comparisons of stent and non-stent interventions in infrainguinal peripheral artery disease: insights from the Excellence in Peripheral Artery Disease (XLPAD) Registry. J Invasive Cardiol. 2019; 31:1–9. PMID: 30611122.27. Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med. 2006; 354:1879–1888. PMID: 16672699.28. Shammas NW, Coiner D, Shammas GA, Dippel EJ, Christensen L, Jerin M. Percutaneous lower-extremity arterial interventions with primary balloon angioplasty versus Silverhawk atherectomy and adjunctive balloon angioplasty: randomized trial. J Vasc Interv Radiol. 2011; 22:1223–1228. PMID: 21757372.29. Dattilo R, Himmelstein SI, Cuff RF. The COMPLIANCE 360° Trial: a randomized, prospective, multicenter, pilot study comparing acute and long-term results of orbital atherectomy to balloon angioplasty for calcified femoropopliteal disease. J Invasive Cardiol. 2014; 26:355–360. PMID: 25091093.30. Baubeta Fridh E, Andersson M, Thuresson M, Sigvant B, Kragsterman B, Johansson S, et al. Amputation rates, mortality, and pre-operative comorbidities in patients revascularised for intermittent claudication or critical limb ischaemia: a population based study. Eur J Vasc Endovasc Surg. 2017; 54:480–486. PMID: 28797662.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Intermittent Claudication in Peripheral Arterial Disease
- Interventional and Surgical Treatment of Peripheral Artery Disease in Diabetic Patients
- Outcomes of Infrainguinal Arterial Bypasses for the Patients with Atherosclerotic Lower Extremity Arterial Occlusive Disease
- Catheter-Directed Thrombolysis for Persistent Sciatic Artery Presenting with Acute Limb Ischemia
- Diagnosis of Peripheral Artery Disease: Focus on the 2016 American Heart Association/American College of Cardiology and 2017 European Society of Cardiology Guidelines