J Korean Med Sci.
2024 Jun;39(22):e186. 10.3346/jkms.2024.39.e186.
Late Parasitological Failure and Subsequent Isolated Gametocytemia of Uncomplicated Plasmodium falciparum Malaria in a Returned Traveler From Ghana, 2023
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 2Department of Laboratory Medicine, Ewha Womans University Mokdong Hospital, Seoul, Korea
- KMID: 2556300
- DOI: http://doi.org/10.3346/jkms.2024.39.e186
Abstract
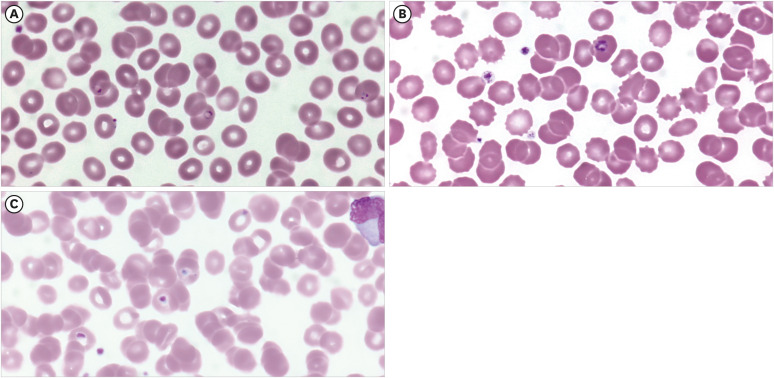
- Herein, we report a case of uncomplicated falciparum malaria with late parasitological failure in a 45-year-old businessman returning from Ghana. The patient visited the emergency department with high fever, headache, and dizziness. He traveled without antimalarial chemoprophylaxis. Laboratory tests led to the diagnosis of uncomplicated falciparum malaria with an initial density of 37,669 parasites per μL of blood (p/μL). The patient was treated with intravenous artesunate followed by atovaquone/proguanil. He was discharged with improved condition and decreased parasite density of 887 p/μL. However, at follow-up, parasite density increased to 7,630 p/μL despite the absence of any symptoms. Suspecting treatment failure, the patient was administered intravenous artesunate and doxycycline for seven days and then artemether/lumefantrine for three days. Blood smear was negative for asexual parasitemia after re-treatment but positive for gametocytemia until day 101 from the initial diagnosis. Overall, this case highlights the risk of late parasitological failure in patients with imported uncomplicated falciparum malaria.
Figure
Reference
-
1. Venkatesan P. The 2023 WHO world malaria report. Lancet Microbe. 2024; 5(3):e214. PMID: 38309283.2. Korea Disease Control and Prevention Agency. Statistics of infectious diseases. Updated 2024. Accessed April 10, 2024. https://dportal.kdca.go.kr/pot/is/rgin.do .3. Angelo KM, Libman M, Caumes E, Hamer DH, Kain KC, Leder K, et al. Malaria after international travel: a GeoSentinel analysis, 2003–2016. Malar J. 2017; 16(1):293. PMID: 28728595.4. Jeon BH, Park K, Kwon JR, Cho EH. Epidemiological characteristics of reported malaria cases in South Korea in 2018. Public Health Wkly Rep. 2018; 12(19):599–605.5. World Health Organization. WHO Guidelines for Malaria. Geneva, Switzerland: WHO;2023.6. Sinclair D, Zani B, Donegan S, Olliaro P, Garner P. Artemisinin-based combination therapy for treating uncomplicated malaria. Cochrane Database Syst Rev. 2009; 2009(3):CD007483. PMID: 19588433.7. World Health Organization. Methods for Surveillance of Antimalarial Drug Efficacy. Geneva, Switzerland: WHO;2009.8. Mumtaz R, Okell LC, Challenger JD. Asymptomatic recrudescence after artemether-lumefantrine treatment for uncomplicated falciparum malaria: a systematic review and meta-analysis. Malar J. 2020; 19(1):453. PMID: 33298080.9. Amoah LE, Asare KK, Dickson D, Anang SF, Busayo A, Bredu D, et al. Nationwide molecular surveillance of three Plasmodium species harboured by symptomatic malaria patients living in Ghana. Parasit Vectors. 2022; 15(1):40. PMID: 35090545.10. Dieng CC, Morrison V, Donu D, Cui L, Amoah L, Afrane Y, et al. Distribution of Plasmodium falciparum K13 gene polymorphisms across transmission settings in Ghana. BMC Infect Dis. 2023; 23(1):801. PMID: 37974079.11. Kuhn S, Gill MJ, Kain KC. Emergence of atovaquone-proguanil resistance during treatment of Plasmodium falciparum malaria acquired by a non-immune north American traveller to west Africa. Am J Trop Med Hyg. 2005; 72(4):407–409. PMID: 15827276.12. Stepniewska K, Ashley E, Lee SJ, Anstey N, Barnes KI, Binh TQ, et al. In vivo parasitological measures of artemisinin susceptibility. J Infect Dis. 2010; 201(4):570–579. PMID: 20085495.13. Makanga M, Krudsood S. The clinical efficacy of artemether/lumefantrine (Coartem). Malar J. 2009; 8(Suppl 1):S5.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Plasmodium falciparum Gametocytemia Successfully Treated with Primaquine
- Predictive score of uncomplicated falciparum malaria patients turning to severe malaria
- Primaquine Administration after Falciparum Malaria Treatment in Malaria Hypoendemic Areas with High Incidence of Falciparum and Vivax Mixed Infection: Pros and Cons
- A Case of Cerebral Malaria Associated with Renal Failure due to Plasmodium falciparum
- Multiple Cerebral Infarcts Following Acute Plasmodium vivax Infection