Korean J Sports Med.
2024 Jun;42(2):126-135. 10.5763/kjsm.2024.42.2.126.
Associations of Step Volume and Intensity with Metabolic Syndrome among Korean Adults: A Cross-sectional Observational Study
- Affiliations
-
- 1Department of Physical Education, Seoul National University, Seoul, Korea
- 2Institute of Sport Science, Seoul National University, Seoul, Korea
- 3Department of Aero Fitness, Korea Air Force Academy, Cheongju, Korea
- 4Department of Physical Education, Korea Military Academy, Seoul, Korea
- 5School of Software Engineering, Joongbu University, Goyang, Korea
- 6Department of Physical Education, Dongguk University, Seoul, Korea
- 7Department of Psychology, Seoul National University, Seoul, Korea
- KMID: 2556278
- DOI: http://doi.org/10.5763/kjsm.2024.42.2.126
Abstract
- Purpose
This study was performed to investigate the association between step volume and intensity with the prevalence of metabolic syndrome (MS) in Korean adults.
Methods
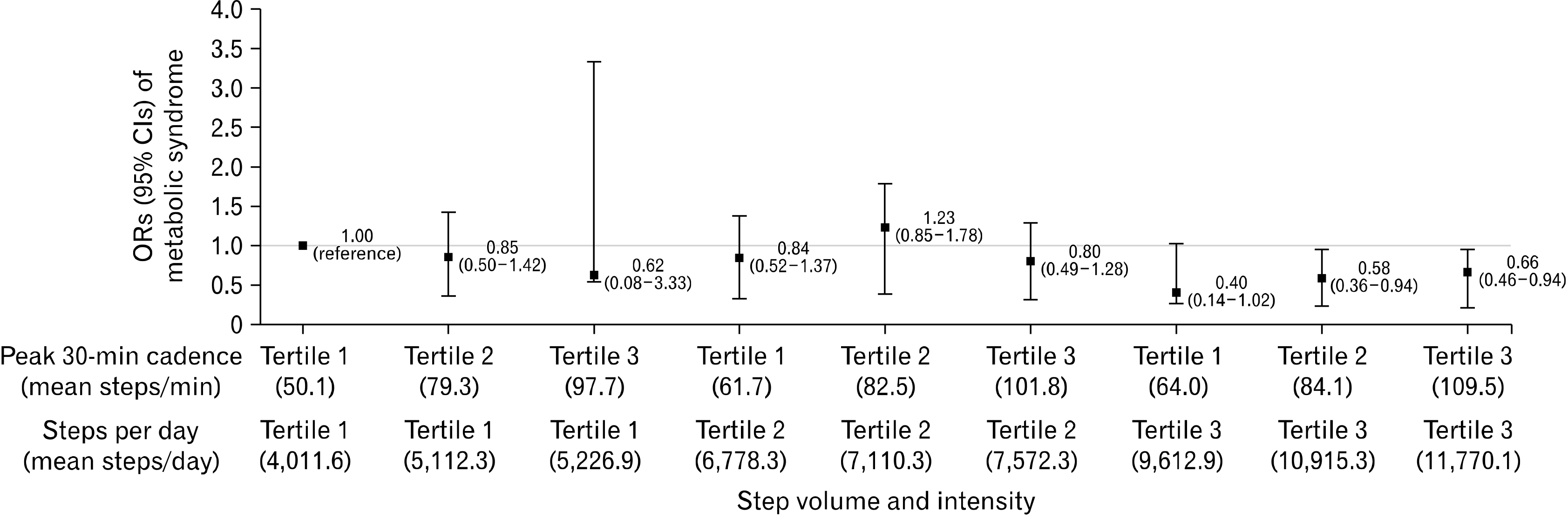
The study analyzed 2,038 adults from the 2014 to 2017 Korea National Health and Nutrition Examination Survey, defining MS based on waist circumference, blood pressure, triglycerides, glucose, and high-density lipoprotein cholesterols. Step volume and intensity were calculated using average number of steps per day and peak 30-minute cadence, respectively. Logistic regression analysis was used to calculate the odds ratios (ORs) and 95% confidence intervals (CIs) of MS by tertiles of step volume and intensity. A joint analysis was conducted to examine the combined association between step volume and intensity with the prevalence of MS. We divided the participants into nine groups according to their step volume (tertiles) and intensity (tertiles).
Results
There were 478 MS cases. Compared to the lowest tertile of volume, the ORs of MS were 1.06 (95% CI, 0.79–1.42) and 0.64 (95% CI, 0.47–0.88) in the middle and highest tertile of volume. Compared to the lowest tertile of intensity, the ORs were 1.02 (95% CI, 0.76–1.36) and 0.74 (95% CI, 0.55–1.01) in the middle and highest tertile of intensity. In the joint analysis, compared to the group with both lowest volume and intensity, the ORs were significantly lower in all groups with the highest volume, except the group with the lowest intensity.
Conclusion
Although only greater step volume, not intensity, was independently related to MS, both step volume and intensity appear to be important for preventing MS.
Keyword
Figure
Reference
-
1. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. 2001; Executive summary of the third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA. 285:2486–97. DOI: 10.1001/jama.285.19.2486. PMID: 11368702.2. Mottillo S, Filion KB, Genest J, et al. 2010; The metabolic syndrome and cardiovascular risk a systematic review and meta-analysis. J Am Coll Cardiol. 56:1113–32. DOI: 10.1016/j.jacc.2010.05.034. PMID: 20863953.3. Zhang F, Liu L, Zhang C, Ji S, Mei Z, Li T. 2021; Association of metabolic syndrome and its components with risk of stroke recurrence and mortality: a meta-analysis. Neurology. 97:e695–705. DOI: 10.1212/WNL.0000000000012415.4. Chew NW, Ng CH, Tan DJ, et al. 2023; The global burden of metabolic disease: data from 2000 to 2019. Cell Metab. 35:414–28. DOI: 10.1016/j.cmet.2023.02.003. PMID: 36889281.5. Kim Mh, Lee Sh, Shin KS, et al. 2020; The change of metabolic syndrome prevalence and its risk factors in Korean adults for decade: Korea National Health and Nutrition Examination Survey for 2008-2017. Korean J Fam Pract. 10:44–52. DOI: 10.21215/kjfp.2020.10.1.44.
Article6. World Health Organization (WHO). 2020. Nov. 25. WHO guidelines on physical activity and sedentary behaviour [Internet]. WHO;Available from: https://www.who.int/publications/i/item/9789240015128. cited 2024 May 20.7. 2018 Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee scientific report. U.S. Department of Health and Human Services;2018.8. Ham SA, Kruger J, Tudor-Locke C. 2009; Participation by US adults in sports, exercise, and recreational physical activities. J Phys Act Health. 6:6–14. DOI: 10.1123/jpah.6.1.6. PMID: 19211953.
Article9. Tudor-Locke C, Rowe DA. 2012; Using cadence to study free-living ambulatory behaviour. Sports Med. 42:381–98. DOI: 10.2165/11599170-000000000-00000. PMID: 22462794.
Article10. Murtagh EM, Nichols L, Mohammed MA, Holder R, Nevill AM, Murphy MH. 2015; The effect of walking on risk factors for cardiovascular disease: an updated systematic review and meta-analysis of randomised control trials. Prev Med. 72:34–43. DOI: 10.1016/j.ypmed.2014.12.041. PMID: 25579505.
Article11. Patel AV, Hildebrand JS, Leach CR, et al. 2018; Walking in relation to mortality in a large prospective cohort of older U.S. adults. Am J Prev Med. 54:10–9. DOI: 10.1016/j.amepre.2017.08.019. PMID: 29056372.
Article12. Takahashi H, Kuriyama S, Tsubono Y, et al. 2007; Time spent walking and risk of colorectal cancer in Japan: the Miyagi Cohort study. Eur J Cancer Prev. 16:403–8. DOI: 10.1097/01.cej.0000236249.63489.05. PMID: 17923810.
Article13. An KY. 2020; Comparison between walking and moderate-to-vigorous physical activity: associations with metabolic syndrome components in Korean older adults. Epidemiol Health. 42:e2020066. DOI: 10.4178/epih.e2020066. PMID: 33147901. PMCID: PMC7871155.14. Peterson MJ, Morey MC, Giuliani C, et al. 2010; Walking in old age and development of metabolic syndrome: the health, aging, and body composition study. Metab Syndr Relat Disord. 8:317–22. DOI: 10.1089/met.2009.0090. PMID: 20367219. PMCID: PMC3072703.
Article15. Woolf-May K, Scott A, Kearney E, Jones DW. 2011; The effect of 24 weeks of moderate intensity walking upon metabolic syndrome risk factors in previously sedentary/low active men. J Exerc Physiol Online. 14:145–56.16. Sisson SB, Camhi SM, Church TS, Tudor-Locke C, Johnson WD, Katzmarzyk PT. 2010; Accelerometer-determined steps/day and metabolic syndrome. Am J Prev Med. 38:575–82. DOI: 10.1016/j.amepre.2010.02.015. PMID: 20494233.
Article17. Tudor-Locke C, Craig CL, Brown WJ, et al. 2011; How many steps/day are enough? For adults. Int J Behav Nutr Phys Act. 8:79. DOI: 10.1186/1479-5868-8-79. PMID: 21798015. PMCID: PMC3197470.
Article18. Tudor-Locke C, Han H, Aguiar EJ, et al. 2018; How fast is fast enough? Walking cadence (steps/min) as a practical estimate of intensity in adults: a narrative review. Br J Sports Med. 52:776–88. DOI: 10.1136/bjsports-2017-097628. PMID: 29858465. PMCID: PMC6029645.
Article19. Adams B, Fidler K, Demoes N, et al. 2019; Cardiometabolic thresholds for peak 30-min cadence and steps/day. PLoS One. 14:e0219933. DOI: 10.1371/journal.pone.0219933. PMID: 31374078. PMCID: PMC6677301.
Article20. Cuthbertson CC, Moore CC, Sotres-Alvarez D, et al. 2022; Associations of steps per day and step intensity with the risk of diabetes: the Hispanic Community Health Study /Study of Latinos (HCHS/SOL). Int J Behav Nutr Phys Act. 19:46. DOI: 10.1186/s12966-022-01284-2. PMID: 35428253. PMCID: PMC9013106.21. Saint-Maurice PF, Troiano RP, Bassett DR, et al. 2020; Association of daily step count and step intensity with mortality among US adults. JAMA. 323:1151–60. DOI: 10.1001/jama.2020.1382. PMID: 32207799. PMCID: PMC7093766.
Article22. Del Pozo Cruz B, Ahmadi MN, Lee IM, Stamatakis E. 2022; Prospective associations of daily step counts and intensity with cancer and cardiovascular disease incidence and mortality and all-cause mortality. JAMA Intern Med. 182:1139–48. DOI: 10.1001/jamainternmed.2022.4000. PMID: 36094529. PMCID: PMC9468953.
Article23. Stens NA, Bakker EA, Mañas A, et al. 2023; Relationship of daily step counts to all-cause mortality and cardiovascular events. J Am Coll Cardiol. 82:1483–94. DOI: 10.1016/j.jacc.2023.07.029. PMID: 37676198.24. Troiano RP, Berrigan D, Dodd KW, Mâsse LC, Tilert T, McDowell M. 2008; Physical activity in the United States measured by accelerometer. Med Sci Sports Exerc. 40:181–8. DOI: 10.1249/mss.0b013e31815a51b3. PMID: 18091006.
Article25. Lee H, Lee M, Choi JY, Oh KK, Kim Y, Kim S. 2018; KNHANES activity raw data processing. Korea J Meas Eval Phys Educ Sport Sci. 20:83–94. DOI: 10.21797/ksme.2018.20.2.008.26. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). 2002; Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 106:3143–421. DOI: 10.1161/circ.106.25.3143. PMID: 12485966.27. Kim BY, Kang SM, Kang JH, et al. 2021; 2020 Korean Society for the Study of Obesity Guidelines for the Management of Obesity in Korea. J Obes Metab Syndr. 30:81–92. DOI: 10.7570/jomes21022. PMID: 34045368. PMCID: PMC8277596.
Article28. Lee SH, Lee Y, Seo JH, Kim YA. 2018; Association between exercise and metabolic syndrome in Koreans. J Obes Metab Syndr. 27:117–24. DOI: 10.7570/jomes.2018.27.2.117. PMID: 31089551. PMCID: PMC6489454.29. Amirfaiz S, Shahril MR. 2019; Objectively measured physical activity, sedentary behavior, and metabolic syndrome in adults: systematic review of observational evidence. Metab Syndr Relat Disord. 17:1–21. DOI: 10.1089/met.2018.0032. PMID: 30272527.
Article30. Newton RL, Han H, Johnson WD, et al. 2013; Steps/day and metabolic syndrome in African American adults: the Jackson Heart Study. Prev Med. 57:855–9. DOI: 10.1016/j.ypmed.2013.09.018. PMID: 24096141. PMCID: PMC4001862.
Article31. Sagawa N, Rockette-Wagner B, Azuma K, et al. 2020; Physical activity levels in American and Japanese men from the ERA-JUMP Study and associations with metabolic syndrome. J Sport Health Sci. 9:170–8. DOI: 10.1016/j.jshs.2019.09.007. PMID: 32099725. PMCID: PMC7031775.
Article32. Cabral LL, Browne RA, Freire YA, et al. 2023; Association of daily step volume and intensity with cardiometabolic risk in older adults. Exp Gerontol. 179:112245. DOI: 10.1016/j.exger.2023.112245. PMID: 37356466.
Article33. Sumner J, Uijtdewilligen L, Yee AC, et al. 2020; Volume and intensity of stepping activity and cardiometabolic risk factors in a multi-ethnic Asian population. Int J Environ Res Public Health. 17:863. DOI: 10.3390/ijerph17030863. PMID: 32019086. PMCID: PMC7037023.
Article34. Tudor-Locke C, Schuna JM, Han HO, et al. 2017; Step-based physical activity metrics and cardiometabolic risk: NHANES 2005-2006. Med Sci Sports Exerc. 49:283–91. DOI: 10.1249/MSS.0000000000001100. PMID: 27669450. PMCID: PMC5412514.35. Aguiar EJ, Gould ZR, Ducharme SW, Moore CC, McCullough AK, Tudor-Locke C. 2019; Cadence-based classification of minimally moderate intensity during overground walking in 21- to 40-year-old adults. J Phys Act Health. 16:1092–7. DOI: 10.1123/jpah.2019-0261. PMID: 31698337. PMCID: PMC7200288.
Article36. Garber CE, Blissmer B, Deschenes MR, et al. 2011; American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc. 43:1334–59. DOI: 10.1249/MSS.0b013e318213fefb. PMID: 21694556.37. Seo MW, Eum Y, Jung HC. 2023; Leisure time physical activity: a protective factor against metabolic syndrome development. BMC Public Health. 23:2449. DOI: 10.1186/s12889-023-17340-w. PMID: 38062414. PMCID: PMC10701969.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associations of type and intensity of social participation with depression, self-rated health, and life satisfaction among community-dwelling older adults in the Republic of Korea: a nationwide cross-sectional study
- Association between Exercise and Metabolic Syndrome in Koreans
- Relationships between Walking, Body Mass Index, and Risk Factors of Metabolic Syndrome among Korean Adults: Data from the Fifth Korea National Health and Nutrition Examination Survey (2010-2012)
- Serum vitamin D status and metabolic syndrome: a systematic review and dose-response meta-analysis
- Association between Metabolic Syndrome and Microalbuminuria in Korean Adults