J Stroke.
2024 May;26(2):231-241. 10.5853/jos.2024.00367.
The Influence of Non-High-Density Lipoprotein Cholesterol on the Efficacy of Genotype-Guided Dual Antiplatelet Therapy in Preventing Stroke Recurrence
- Affiliations
-
- 1Department of Neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
- 2China National Clinical Research Center for Neurological Diseases, Beijing, China
- 3Department of Clinical Epidemiology and Clinical Trial, Capital Medical University, Beijing, China
- 4Beijing Municipal Key Laboratory of Clinical Epidemiology, Beijing, China
- 5Advanced Innovation Center for Human Brain Protection, Beijing Tiantan Hospital, Capital Medical University, Beijing, China
- KMID: 2556043
- DOI: http://doi.org/10.5853/jos.2024.00367
Abstract
- Background and Purpose
Non-high-density lipoprotein cholesterol (non-HDL-C), which represents the total cholesterol content of all pro-atherogenic lipoproteins, has recently been included as a new target for lipid-lowering therapy in high-risk atherosclerotic patients in multiple guidelines. Herein, we aimed to explore the relationship between non-HDL-C level and the efficacy and safety of ticagrelor-aspirin versus clopidogrel-aspirin in preventing stroke recurrence.
Methods
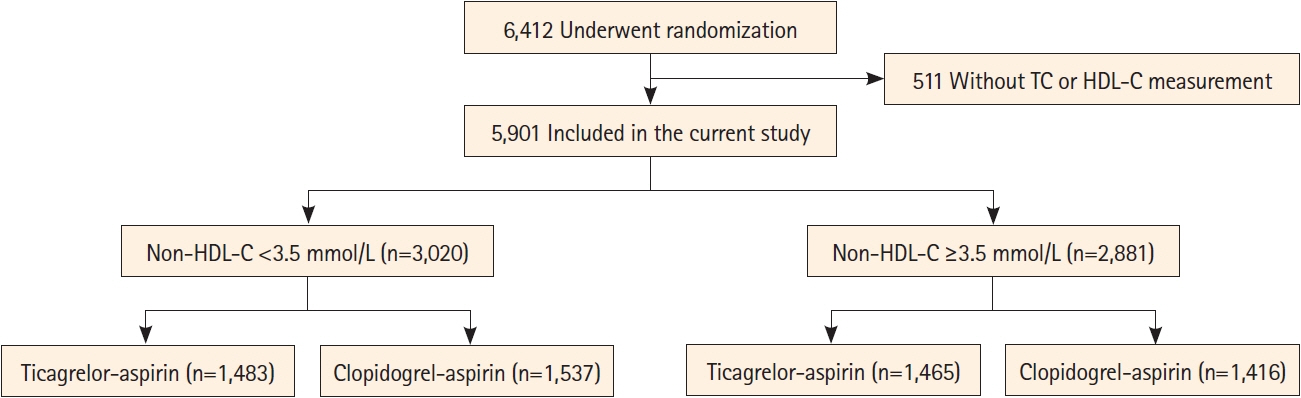
This study comprised a post hoc analysis of the CHANCE-2 (Ticagrelor or Clopidogrel in High-Risk Patients with Acute Nondisabling Cerebrovascular Events II) trial, from which 5,901 patients with complete data on non-HDL-C were included and categorized by median non-HDL-C levels, using a cutoff of 3.5 mmol/L. The primary efficacy and safety outcomes were recurrent stroke and severe or moderate bleeding within 90 days.
Results
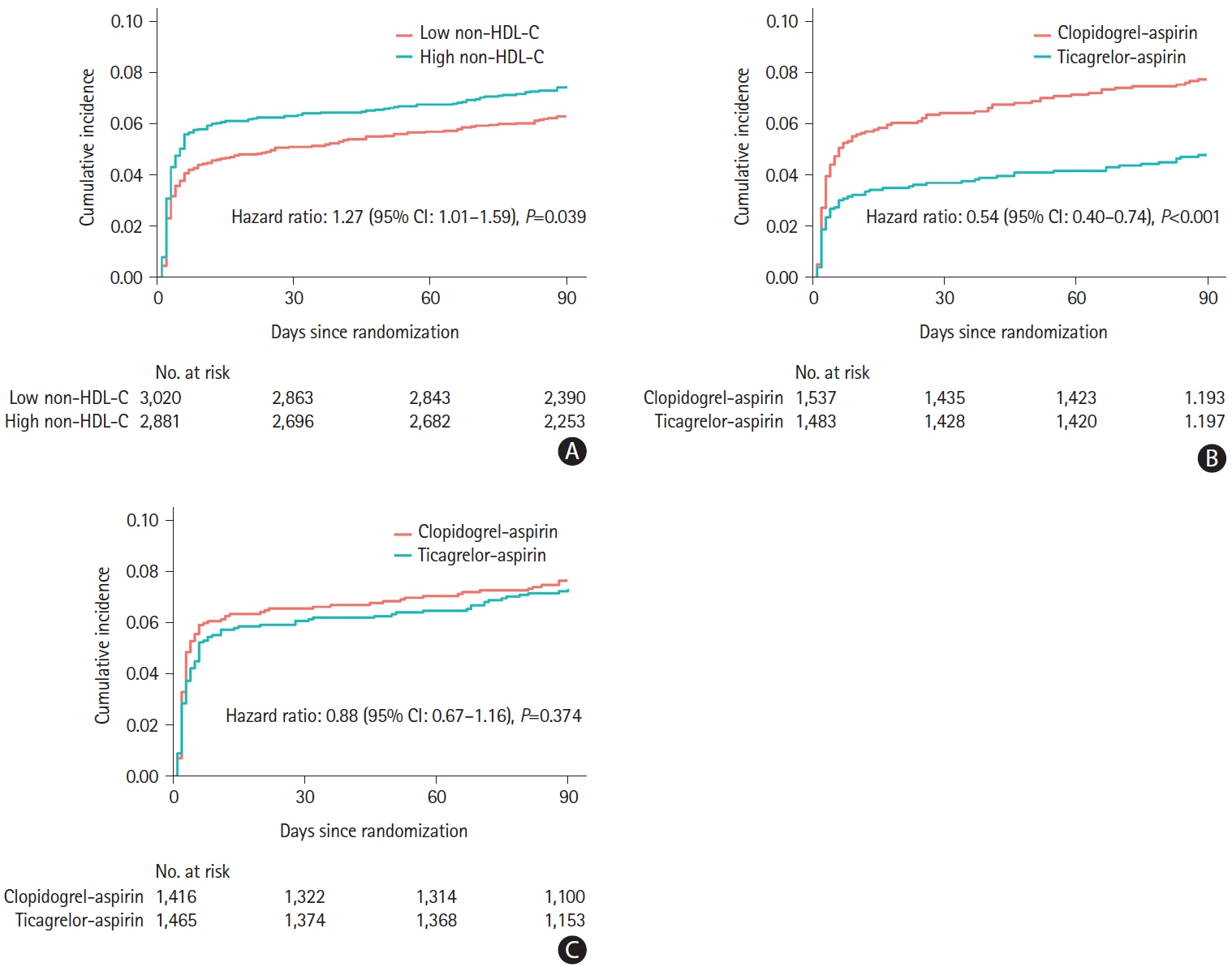
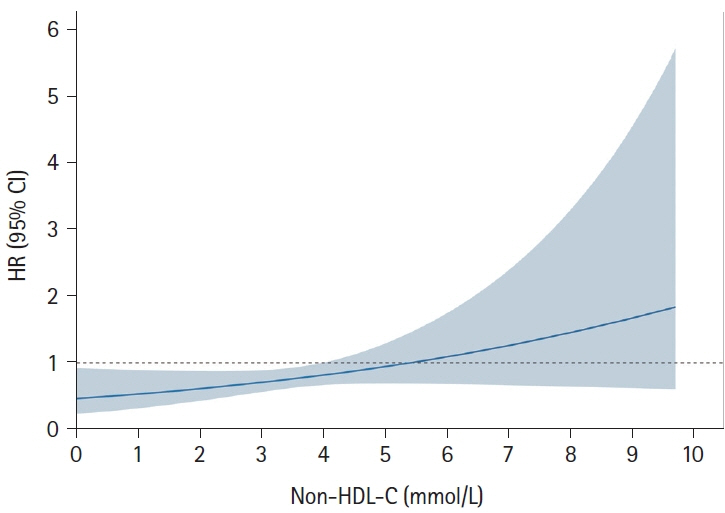
Ticagrelor-aspirin significantly reduced the risk of recurrent stroke in patients with low non-HDL-C (71 [4.8%] vs. 119 [7.7%]; adjusted hazard ratio [HR] 0.54; 95% confidence interval [CI], 0.40–0.74), but not in those with high non-HDL-C (107 [7.3%] vs. 108 [7.6%]; adjusted HR, 0.88; 95% CI, 0.67–1.16), compared with clopidogrel-aspirin (P for interaction=0.010). When analyzed as a continuous variable, the benefit of ticagrelor-aspirin for recurrent stroke decreased as non-HDL-C levels increased. No significant differences in the treatment assignments across the non-HDL-C groups were observed in terms of the rate of severe or moderate bleeding (5 [0.3%] vs. 8 [0.5%] in the low non-HDL-C group; 4 [0.3%] vs. 2 [0.1%] in the high non-HDL-C group; P for interaction=0.425).
Conclusion
CHANCE-2 participants with low non-HDL-C levels received more clinical benefit from ticagrelor-aspirin versus clopidogrel-aspirin compared to those with high non-HDL-C, following minor ischemic stroke or transient ischemic attack.
Figure
Reference
-
References
1. Xu J, Tao Y, Li H, Gu H, Xie X, Meng X, et al. Different levels of blood pressure, different benefit from dual antiplatelet therapy in minor stroke or TIA patients. Sci Rep. 2017; 7:3884.
Article2. Li J, Wang Y, Wang D, Lin J, Wang A, Zhao X, et al. Glycated albumin predicts the effect of dual and single antiplatelet therapy on recurrent stroke. Neurology. 2015; 84:1330–1336.
Article3. Zhou Y, Pan Y, Wu Y, Zhao X, Li H, Wang D, et al. Effect of estimated glomerular filtration rate decline on the efficacy and safety of clopidogrel with aspirin in minor stroke or transient ischemic attack: CHANCE substudy (clopidogrel in high-risk patients with acute nondisabling cerebrovascular events). Stroke. 2016; 47:2791–2796.
Article4. de Havenon A, Johnston SC, Easton JD, Kim AS, Sheth KN, Lansberg M, et al. Evaluation of systolic blood pressure, use of aspirin and clopidogrel, and stroke recurrence in the plateletoriented inhibition in new TIA and minor ischemic stroke trial. JAMA Netw Open. 2021; 4:e2112551.
Article5. Mac Grory B, Piccini JP, Yaghi S, Poli S, De Havenon A, Rostanski SK, et al. Hyperglycemia, risk of subsequent stroke, and efficacy of dual antiplatelet therapy: a post hoc analysis of the point trial. J Am Heart Assoc. 2022; 11:e023223.
Article6. Wang A, Meng X, Tian X, Johnston SC, Li H, Bath PM, et al. Effect of hypertension on efficacy and safety of ticagreloraspirin versus clopidogrel-aspirin in minor stroke or transient ischemic attack. Stroke. 2022; 53:2799–2808.
Article7. Wang A, Xie X, Tian X, Johnston SC, Li H, Bath PM, et al. Ticagrelor-aspirin versus clopidogrel-aspirin among CYP2C19 loss-of-function carriers with minor stroke or transient ischemic attack in relation to renal function: a post hoc analysis of the CHANCE-2 trial. Ann Intern Med. 2022; 175:1534–1542.
Article8. Helgadottir A, Thorleifsson G, Snaebjarnarson A, Stefansdottir L, Sveinbjornsson G, Tragante V, et al. Cholesterol not particle concentration mediates the atherogenic risk conferred by apolipoprotein B particles: a Mendelian randomization analysis. Eur J Prev Cardiol. 2022; 29:2374–2385.
Article9. Ridker PM, Rifai N, Cook NR, Bradwin G, Buring JE. Non-HDL cholesterol, apolipoproteins A-I and B100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in women. JAMA. 2005; 294:326–333.
Article10. Pischon T, Girman CJ, Sacks FM, Rifai N, Stampfer MJ, Rimm EB. Non-high-density lipoprotein cholesterol and apolipoprotein B in the prediction of coronary heart disease in men. Circulation. 2005; 112:3375–3383.
Article11. Brunner FJ, Waldeyer C, Ojeda F, Salomaa V, Kee F, Sans S, et al. Application of non-HDL cholesterol for population-based cardiovascular risk stratification: results from the Multinational Cardiovascular Risk Consortium. Lancet. 2019; 394:2173–2183.
Article12. Johannesen CDL, Mortensen MB, Langsted A, Nordestgaard BG. Apolipoprotein B and non-HDL cholesterol better reflect residual risk than LDL cholesterol in statin-treated patients. J Am Coll Cardiol. 2021; 77:1439–1450.
Article13. Kastelein JJ, van der Steeg WA, Holme I, Gaffney M, Cater NB, Barter P, et al. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation. 2008; 117:3002–3009.14. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelines. Circulation. 2019; 139:e1082–e1143.15. Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020; 41:111–188.16. Pearson GJ, Thanassoulis G, Anderson TJ, Barry AR, Couture P, Dayan N, et al. 2021 Canadian Cardiovascular Society guidelines for the management of dyslipidemia for the prevention of cardiovascular disease in adults. Can J Cardiol. 2021; 37:1129–1150.
Article17. Đukanovic´ N, Obradovic´ S, Zdravkovic´ M, Đuraševic´ S, Stojkovic´ M, Tosti T, et al. Lipids and antiplatelet therapy: important considerations and future perspectives. Int J Mol Sci. 2021; 22:3180.
Article18. Scioli MG, Storti G, D’Amico F, Rodríguez Guzmán R, Centofanti F, Doldo E, et al. Oxidative stress and new pathogenetic mechanisms in endothelial dysfunction: potential diagnostic biomarkers and therapeutic targets. J Clin Med. 2020; 9:1995.
Article19. Yang M, Kholmukhamedov A. Platelet reactivity in dyslipidemia: atherothrombotic signaling and therapeutic implications. Rev Cardiovasc Med. 2021; 22:67–81.
Article20. Kim JD, Park CY, Ahn KJ, Cho JH, Choi KM, Kang JG, et al. Non-HDL cholesterol is an independent risk factor for aspirin resistance in obese patients with type 2 diabetes. Atherosclerosis. 2014; 234:146–151.
Article21. Wang Y, Meng X, Wang A, Xie X, Pan Y, Johnston SC, et al. Ticagrelor versus clopidogrel in CYP2C19 loss-of-function carriers with stroke or TIA. N Engl J Med. 2021; 385:2520–2530.
Article22. Wang Y, Johnston C, Bath PM, Meng X, Jing J, Xie X, et al. Clopidogrel with aspirin in high-risk patients with acute nondisabling cerebrovascular events II (CHANCE-2): rationale and design of a multicentre randomised trial. Stroke Vasc Neurol. 2021; 6:280–285.
Article23. GUSTO investigators. An international randomized trial comparing four thrombolytic strategies for acute myocardial infarction. N Engl J Med. 1993; 329:673–682.24. Shen H, Herzog W, Drolet M, Pakyz R, Newcomer S, Sack P, et al. Aspirin resistance in healthy drug-naive men versus women (from the heredity and phenotype intervention heart study). Am J Cardiol. 2009; 104:606–612.
Article25. Bobescu E, Covaciu A, Rus H, Rogozea LM, Badea M, Marceanu LG. Low response to clopidogrel in coronary artery disease. Am J Ther. 2020; 27:e133–e141.
Article26. Bornstein NM, Karepov VG, Aronovich BD, Gorbulev AY, Treves TA, Korczyn AD. Failure of aspirin treatment after stroke. Stroke. 1994; 25:275–277.
Article27. Jäger B, Piackova E, Haller PM, Andric T, Kahl B, Christ G, et al. Increased platelet reactivity in dyslipidemic patients with coronary artery disease on dual anti-platelet therapy. Arch Med Sci. 2019; 15:65–71.
Article28. Carvalho AC, Colman RW, Lees RS. Platelet function in hyperlipoproteinemia. N Engl J Med. 1974; 290:434–438.
Article29. Harmon JT, Tandon NN, Hoeg JM, Jamieson GA. Thrombin binding and response in platelets from patients with dyslipoproteinemias: increased stimulus-response coupling in type II hyperlipoproteinemia. Blood. 1986; 68:498–505.
Article30. Wang N, Tall AR. Cholesterol in platelet biogenesis and activation. Blood. 2016; 127:1949–1953.
Article31. Fessler MB, Rose K, Zhang Y, Jaramillo R, Zeldin DC. Relationship between serum cholesterol and indices of erythrocytes and platelets in the US population. J Lipid Res. 2013; 54:3177–3188.32. Kameda S, Sakata T, Kokubo Y, Mitsuguro M, Okamoto A, Sano M, et al. Association of platelet aggregation with lipid levels in the Japanese population: the Suita study. J Atheroscler Thromb. 2011; 18:560–567.
Article33. Schrör K, Verheugt FWA, Trenk D. Drug-drug interaction between antiplatelet therapy and lipid-lowering agents (statins and PCSK9 inhibitors). Thromb Haemost. 2023; 123:166–176.
Article34. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; 52:e364–e467.
Article35. Elshazly MB, Martin SS, Blaha MJ, Joshi PH, Toth PP, McEvoy JW, et al. Non-high-density lipoprotein cholesterol, guideline targets, and population percentiles for secondary prevention in 1.3 million adults: the VLDL-2 study (very large database of lipids). J Am Coll Cardiol. 2013; 62:1960–1965.
Article36. Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive summary of the third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (adult treatment panel III). JAMA. 2001; 285:2486–2497.37. Wu J, Zhang J, Wang A, Chen S, Wu S, Zhao X. Association between non-high-density lipoprotein cholesterol levels and asymptomatic vulnerable carotid atherosclerotic plaques. Eur J Neurol. 2019; 26:1433–1438.
Article38. Zhao Z, Wang H, Hou Q, Zhou Y, Zhang Y. Non-traditional lipid parameters as potential predictors of carotid plaque vulnerability and stenosis in patients with acute ischemic stroke. Neurol Sci. 2023; 44:835–843.
Article39. Kamtchum-Tatuene J, Noubiap JJ, Wilman AH, Saqqur M, Shuaib A, Jickling GC. Prevalence of high-risk plaques and risk of stroke in patients with asymptomatic carotid stenosis: a meta-analysis. JAMA Neurol. 2020; 77:1524–1535.
Article40. Marnane M, Prendeville S, McDonnell C, Noone I, Barry M, Crowe M, et al. Plaque inflammation and unstable morphology are associated with early stroke recurrence in symptomatic carotid stenosis. Stroke. 2014; 45:801–806.
Article41. Wang G, Jing J, Wang A, Zhang X, Zhao X, Li Z, et al. Non-high-density lipoprotein cholesterol predicts adverse outcomes in acute ischemic stroke. Stroke. 2021; 52:2035–2042.
Article42. VanderWeele TJ, Knol MJ. Interpretation of subgroup analyses in randomized trials: heterogeneity versus secondary interventions. Ann Intern Med. 2011; 154:680–683.
Article43. Pencina KM, Thanassoulis G, Wilkins JT, Vasan RS, Navar AM, Peterson ED, et al. Trajectories of non-HDL cholesterol across midlife: implications for cardiovascular prevention. J Am Coll Cardiol. 2019; 74:70–79.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiplatelet Therapy for Secondary Stroke Prevention in Patients with Ischemic Stroke or Transient Ischemic Attack
- Dual Antiplatelet Therapy after Noncardioembolic Ischemic Stroke or Transient Ischemic Attack: Pros and Cons
- Changes of Plasma Lipids in Stroke Patients
- Hypolipidemic Effects and Safety of Lovastatin in Patients with Primary Hypercholesterolemia
- A Study of Estrogen only Therapy and Estrogen Plus Androgen Combination Therapy in Surgical Menopause Patients