Clin Exp Otorhinolaryngol.
2024 May;17(2):177-187. 10.21053/ceo.2023.00023.
Predictors of Difficult Laryngeal Exposure in Suspension Laryngoscopy: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Otolaryngology Head and Neck Surgery, Xiangya Hospital, Central South University, Changsha, China
- 2Otolaryngology Major Disease Research, Key Laboratory of Hunan Province, Changsha, China
- 3Clinical Research Center for Pharyngolaryngeal Diseases and Voice Disorders in Hunan Province, Changsha, China
- 4National Clinical Research Center for Geriatric Disorders (Xiangya Hospital), Changsha, China
- 5Department of Hematology, Third Xiangya Hospital, Central South University, Changsha, China
- KMID: 2556008
- DOI: http://doi.org/10.21053/ceo.2023.00023
Abstract
Objectives
. Considerable research has been focused on independent predictors of difficult laryngeal exposure (DLE) during suspension laryngoscopy. However, previous studies have yielded inconsistent results and conclusions. Consequently, we performed a meta-analysis of the existing literature with the aim of identifying significant parameters for a standardized preoperative DLE prediction system.
Methods
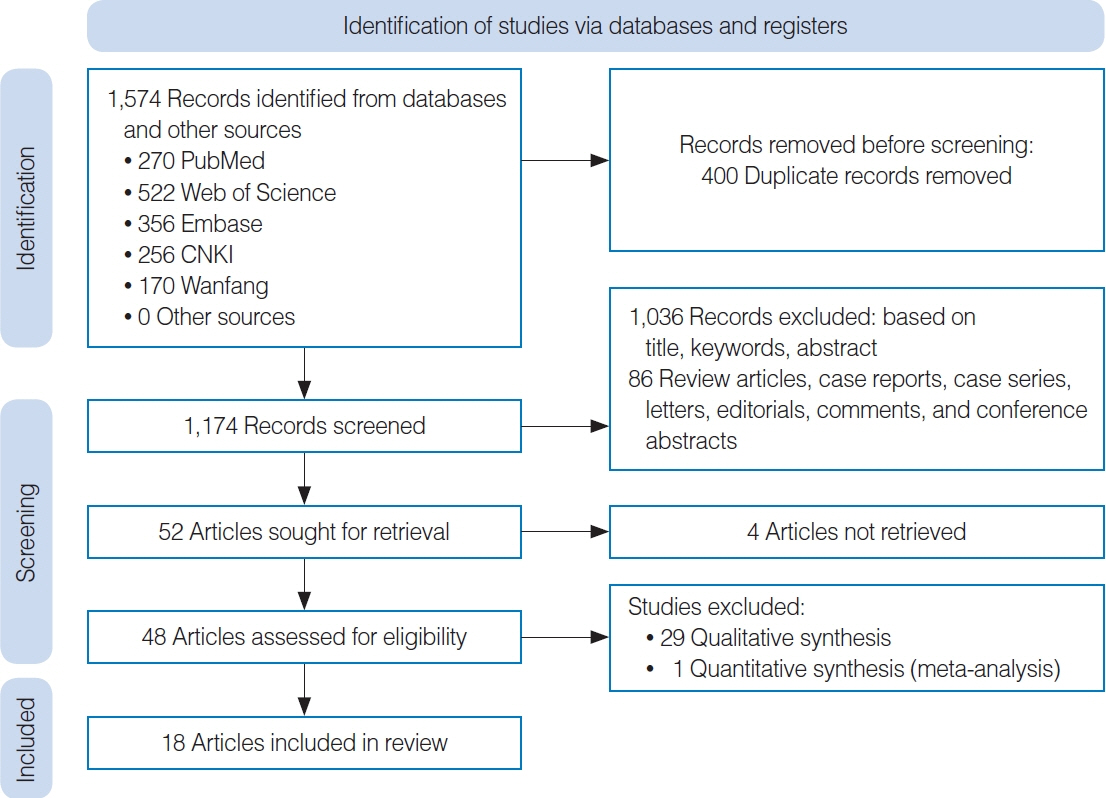
. We systematically retrieved articles from the PubMed, Embase, Web of Science, China National Knowledge Infrastructure, and Wanfang databases up to October 2022. Data from eligible studies were extracted and analyzed using the R programming language. The effect measures included odds ratios (ORs) with 95% confidence intervals (CIs) for dichotomous variables and mean differences (MDs) with 95% CIs for continuous variables.
Results
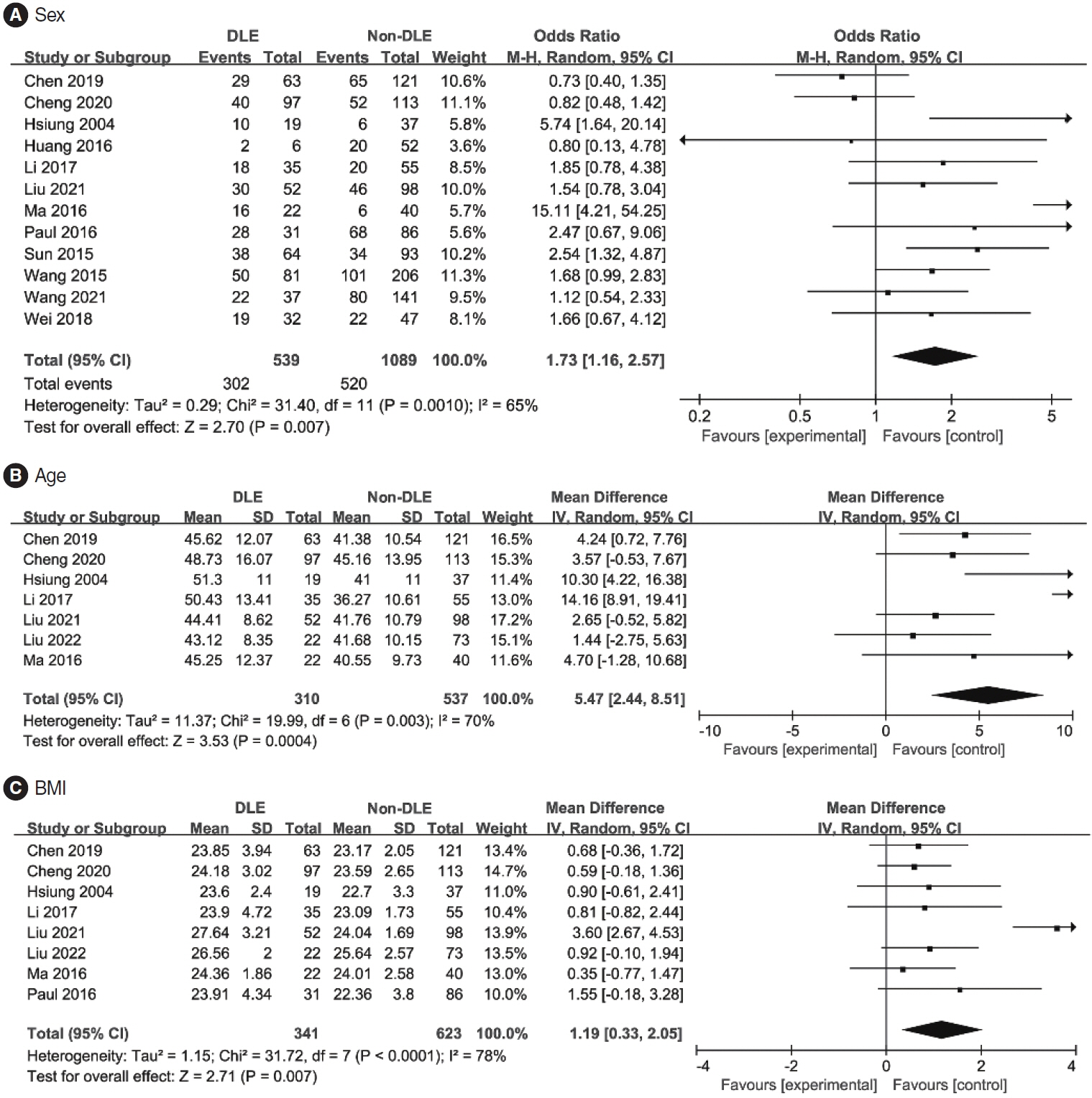
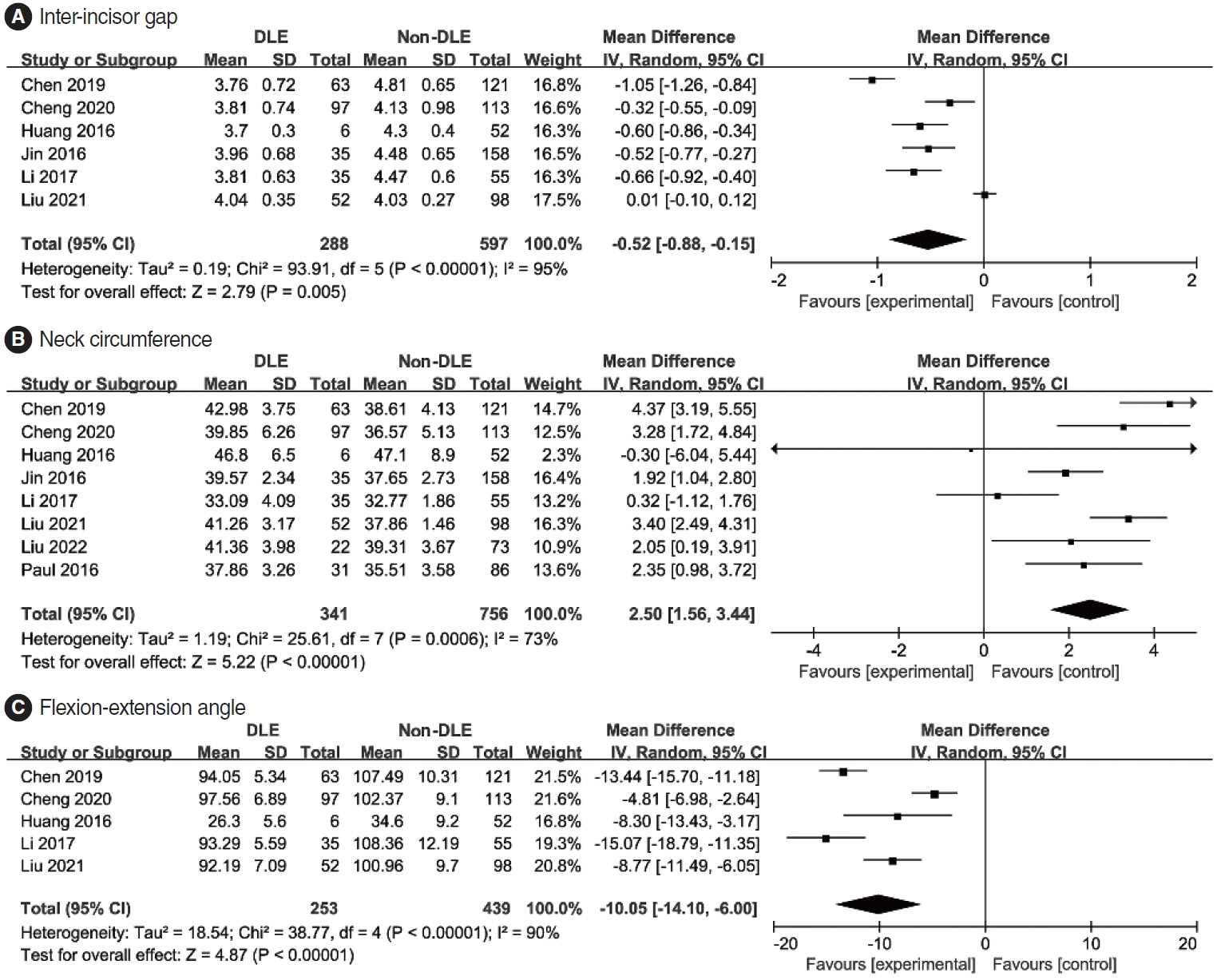
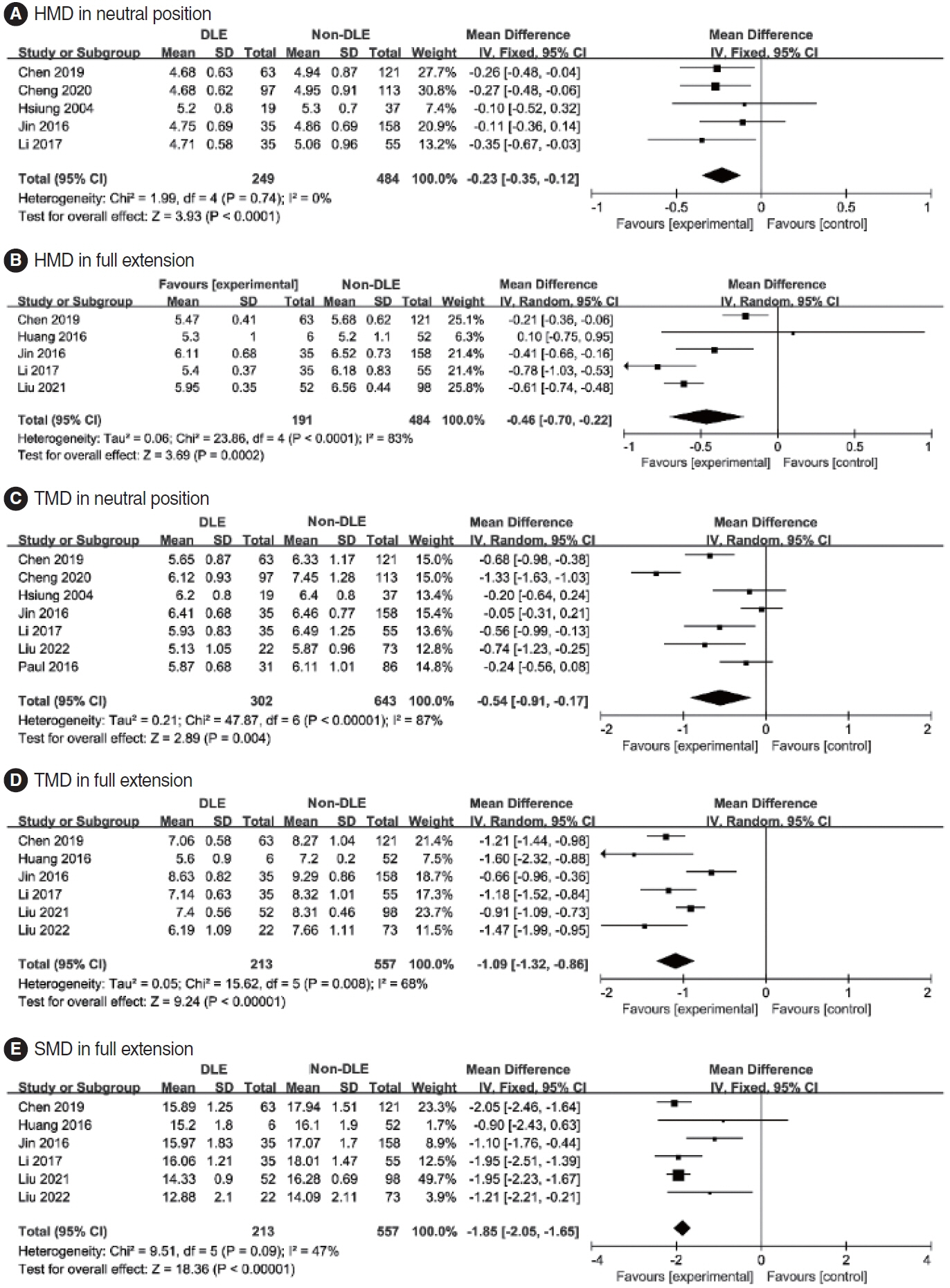
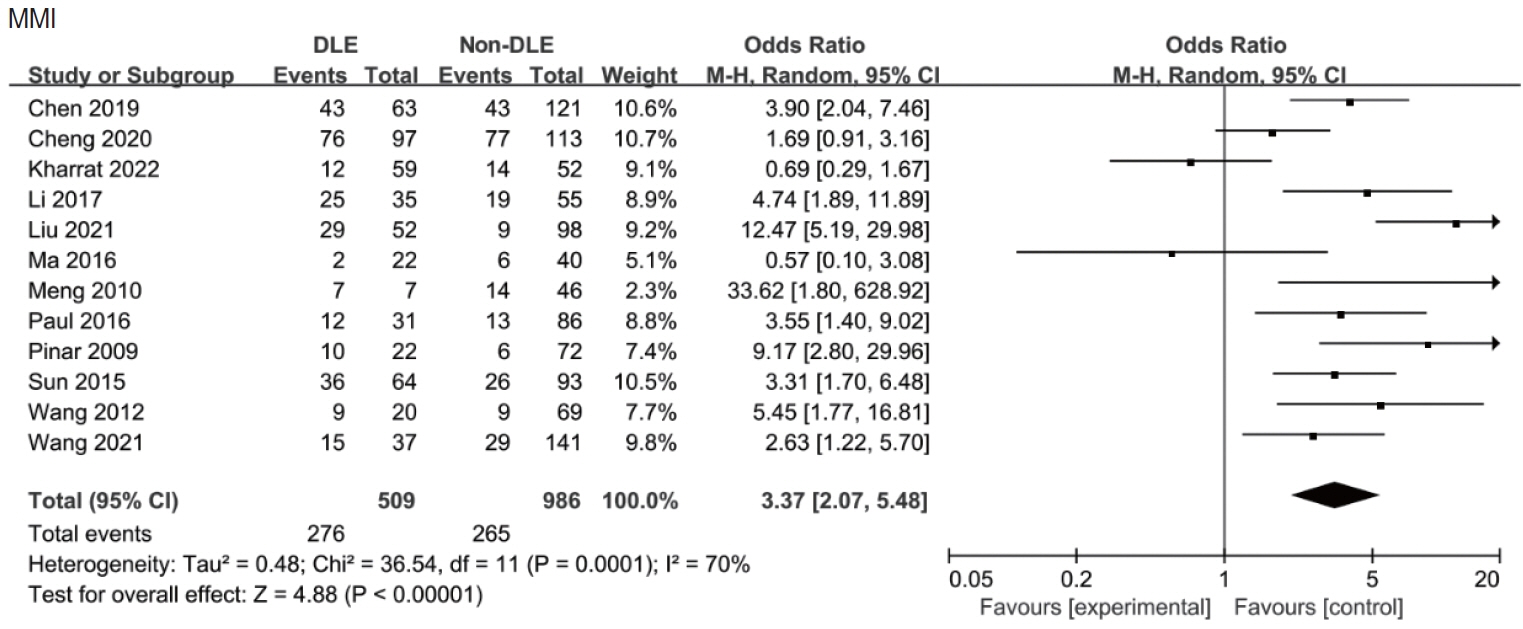
. The search yielded 1,574 studies, of which 18 (involving a total of 2,263 patients) were included. Pooled analysis demonstrated that patients with DLE during microsurgery tended to be male (OR, 1.73; 95% CI, 1.16–2.57); were older (MD, 5.47 years, 95% CI, 2.44–8.51 years); had a higher body mass index (BMI; MD, 1.19 kg/m2; 95% CI, 0.33–2.05 kg/m2); had a greater neck circumference (MD, 2.50 cm; 95% CI, 1.56–3.44 cm); exhibited limited mouth opening (MD, −0.52 cm; 95% CI, −0.88 to −0.15 cm); had limited neck flexibility (MD, −10.05 cm; 95% CI, −14.10 to −6.00 cm); displayed various other anatomical characteristics; and had a high modified Mallampati index (MMI) or test score (OR, 3.37; 95% CI, 2.07–5.48).
Conclusion
. We conducted a comprehensive and systematic analysis of the factors relevant to DLE. Ultimately, we identified sex, age, BMI, neck circumference, MMI, inter-incisor gap, hyomental distance, thyromental distance, sternomental distance, and flexion-extension angle as factors highly correlated with DLE.
Keyword
Figure
Reference
-
1. Paul RR, Varghese AM, Mathew J, Chandrasekharan R, Amalanathan S, Asif SK, et al. Difficult laryngeal exposure in microlaryngoscopy: can it be predicted preoperatively. Indian J Otolaryngol Head Neck Surg. 2016; Mar. 68(1):65–70.
Article2. Pinar E, Calli C, Oncel S, Selek B, Tatar B. Preoperative clinical prediction of difficult laryngeal exposure in suspension laryngoscopy. Eur Arch Otorhinolaryngol. 2009; May. 266(5):699–703.
Article3. Arjun AP, Dutta A. A study of application of preoperative clinical predictors of difficult laryngeal exposure for microlaryngoscopy: the laryngoscore in the Indian population. Indian J Otolaryngol Head Neck Surg. 2019; Dec. 71(4):480–5.
Article4. Piazza C, Mangili S, Bon FD, Paderno A, Grazioli P, Barbieri D, et al. Preoperative clinical predictors of difficult laryngeal exposure for microlaryngoscopy: the Laryngoscore. Laryngoscope. 2014; Nov. 124(11):2561–7.
Article5. Hekiert AM, Mick R, Mirza N. Prediction of difficult laryngoscopy: does obesity play a role. Ann Otol Rhinol Laryngol. 2007; Nov. 116(11):799–804.
Article6. Roh JL, Lee YW. Prediction of difficult laryngeal exposure in patients undergoing microlaryngosurgery. Ann Otol Rhinol Laryngol. 2005; Aug. 114(8):614–20.
Article7. Maughan EF, Rotman A, Rouhani MJ, Thong G, Poncia J, Myatt J, et al. Suspension laryngoscopy experiences in a tertiary airway service: a prospective study of 150 procedures. Clin Otolaryngol. 2022; Jan. 47(1):52–60.
Article8. Hsiung MW, Pai L, Kang BH, Wang BL, Wong CS, Wang HW. Clinical predictors of difficult laryngeal exposure. Laryngoscope. 2004; Feb. 114(2):358–63.
Article9. Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; Jul. 6(7):e1000097.
Article10. Mallampati SR, Gatt SP, Gugino LD, Desai SP, Waraksa B, Freiberger D, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985; Jul. 32(4):429–34.
Article11. Koh LK, Kong CE, Ip-Yam PC. The modified Cormack-Lehane score for the grading of direct laryngoscopy: evaluation in the Asian population. Anaesth Intensive Care. 2002; Feb. 30(1):48–51.
Article12. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. 2010; Sep. 25(9):603–5.
Article13. Chen H, He Z, Li G, Liu C, Zhang D, Huang D, et al. Endoscopy-assisted transoral approach to resect parapharyngeal space tumors: a systematic review and meta-analysis. Laryngoscope. 2021; Oct. 131(10):2246–53.
Article14. Kharrat I, Achour I, Trabelsi JJ, Trigui M, Thabet W, Mnejja M, et al. Prediction of difficulty in direct laryngoscopy. Sci Rep. 2022; Jun. 12(1):10722.
Article15. Meng QX, Gao XH, Song JS, Li P, He L. Mult-factors analysis of the exposure of glottis area with suspend retaining laryngoscope. Clin Med. 2010; Jun. 30(6):41–3.16. Wang M, Xiao ZR, Yu JQ, Zeng RF, Tan GL. Related factors of difficult laryngeal exposure in suspension laryngoscopy under general anesthesia. Med Innov China. 2012; Mar. 9(9):1–2.17. Sun J, Zhang XG, Sun YH, Hu WL, Peng SD, Cui XB, et al. The related factors analysis of difficult laryngeal exposure under microlaryngoscopy. J Inner Mongolia Med Univ. 2015; Apr. 37(2):179–81.18. Wang J, Hu Y, Wang D, Zhao G, Li X, Li Y. The related factors analysis of difficult laryngeal exposure under retaining laryngoscope. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2015; Sep. 29(17):1519–21.19. Huang C, Mo J. Study on affect factors related to laryngeal exposure in self-retaining microscopic surgery. Chin J Otorhinolaryngol. 2016; Aug. 22(4):317–9.20. Wa YL, Xu XL, Zhou L, Wang RQ, Zhuang PY. A study on the X-ray measurement predictors of difficult laryngealexposure in patients undergoing microlaryngosurgery. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2016; Jul. 30(13):1042–6.21. Jin XF, Fan GK. Analysis of the relevant factors for the difficult laryngeal exposure in patients undergoing suspension laryngoscopy. Beijing Med J. 2016; Apr. 38(2):129–32.22. Li JJ, Chen WX, Zhu ZF, Zhang JL, He FY, Wang YJ. Prospective study of riskfactors of difficult laryngeal exposure in suspension laryngoscopy. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2017; Apr. 31(7):520–3.23. Liu YJ, Pang XH, Chu JS, Mao MR, Xu LY. An analysis of the related factors of difficult laryngeal exposure in microsurgical laryngoscope surgery. China Med Pharm. 2021; Dec. 11(24):156–8.24. Liu Y, Zhang Y, Chen Y, Yue L, Su T, Shi S. Sternum-mental angle: a new predictor of difficult: laryngeal exposure in suspension microsurgery: an observational study. Eur Ann Otorhinolaryngol Head Neck Dis. 2022; Aug. 139(4):202–7.25. Chen FS, Zhang ZX, Chen J, Zhang L. Influencing factors of glottis exposure difficulty in laryngoscopic surgery under selfretaining laryngoscope. Mod Instrum Med Treat. 2019; Aug. 25(1):17–20.26. Cheng JW, Ye YH, Wu WJ, Zeng YL. Logistic analysis of influencing factors of glottic exposure difficulty in support laryngoscope. Lingnan Mod Clin Surg. 2020; Feb. 20(1):93–7.27. Wei W, Yan JH, Wang H. Analysis on related influencing factors of glottis exposure difficulty under self-retaining laryngoscope. China Mod Med. 2018; Dec. 25(35):122–4.28. Wang S, Wang XC, Wang YH. Influencing factors of difficult glottic exposure during low-temperature plasma resection under suspension laryngoscope in laryngeal carcinoma patients. Clin Psychosom Dis. 2021; May. 27(3):138–41.29. Dvorak J, Antinnes JA, Panjabi M, Loustalot D, Bonomo M. Age and gender related normal motion of the cervical spine. Spine (Phila Pa 1976). 1992; Oct. 17(10 Suppl):S393–8.
Article30. Vasavada AN, Danaraj J, Siegmund GP. Head and neck anthropometry, vertebral geometry and neck strength in height-matched men and women. J Biomech. 2008; 41(1):114–21.
Article31. Catenaccio E, Mu W, Kaplan A, Fleysher R, Kim N, Bachrach T, et al. Characterization of neck strength in healthy young adults. PM R. 2017; Sep. 9(9):884–91.
Article32. Juvin P, Lavaut E, Dupont H, Lefevre P, Demetriou M, Dumoulin JL, et al. Difficult tracheal intubation is more common in obese than in lean patients. Anesth Analg. 2003; Aug. 97(2):595–600.
Article33. Wajekar AS, Chellam S, Toal PV. Prediction of ease of laryngoscopy and intubation-role of upper lip bite test, modified mallampati classification, and thyromental distance in various combination. J Family Med Prim Care. 2015; Jan-Mar. 4(1):101–5.
Article34. Tomlinson DJ, Erskine RM, Morse CI, Winwood K, Onambele-Pearson G. The impact of obesity on skeletal muscle strength and structure through adolescence to old age. Biogerontology. 2016; Jun. 17(3):467–83.
Article35. Rahemi H, Nigam N, Wakeling JM. The effect of intramuscular fat on skeletal muscle mechanics: implications for the elderly and obese. J R Soc Interface. 2015; Aug. 12(109):20150365.
Article36. Martin SE, Mathur R, Marshall I, Douglas NJ. The effect of age, sex, obesity and posture on upper airway size. Eur Respir J. 1997; Sep. 10(9):2087–90.
Article37. Kletzien H, Hare AJ, Leverson G, Connor NP. Age-related effect of cell death on fiber morphology and number in tongue muscle. Muscle Nerve. 2018; Jan. 57(1):E29–37.
Article38. Hsu PC, Wu HK, Huang YC, Chang HH, Chen YP, Chiang JY, et al. Gender- and age-dependent tongue features in a community-based population. Medicine (Baltimore). 2019; Dec. 98(51):e18350.
Article39. Clarysse C, Meulemans J, van Lierde C, Laenen A, Delaere P, Vander Poorten V. Prospective evaluation and validation of the laryngoscore and the mini-laryngoscore. Laryngoscope. 2024; Apr. 134(4):1807–12.
Article40. Nautiyal S, Kumar Agarwal V, Bist SS, Kumar L, Luthra M. Assessment of preoperative predictors for difficult laryngeal exposure in endolaryngeal surgery. Indian J Otolaryngol Head Neck Surg. 2024; Feb. 76(1):490–4.
Article41. Vaughan CW. Vocal fold exposure in phonosurgery. J Voice. 1993; Jun. 7(2):189–94.
Article42. Merah NA, Wong DT, Ffoulkes-Crabbe DJ, Kushimo OT, Bode CO. Modified Mallampati test, thyromental distance and inter-incisor gap are the best predictors of difficult laryngoscopy in West Africans. Can J Anaesth. 2005; Mar. 52(3):291–6.43. Schmitt HJ, Kirmse M, Radespiel-Troger M. Ratio of patient’s height to thyromental distance improves prediction of difficult laryngoscopy. Anaesth Intensive Care. 2002; Dec. 30(6):763–5.
Article44. Best SR, Kobler JB, Friedman AD, Barbu AM, Zeitels SM, Burns JA. Effect of mandibular tori on glottic exposure during simulated suspension microlaryngoscopy. Ann Otol Rhinol Laryngol. 2014; Mar. 123(3):188–94.
Article45. Ji C, Ni Q, Chen W. Diagnostic accuracy of radiology (CT, X-ray, US) for predicting difficult intubation in adults: a meta-analysis. J Clin Anesth. 2018; Mar. 45:79–87.
Article46. Tirelli G, Gatto A, Fortunati A, Marzolino R, Giudici F, Boscolo Nata F. Predicting laryngeal exposure in microlaryngoscopy: external validation of the laryngoscore. Laryngoscope. 2019; Jun. 129(6):1438–43.
Article47. Incandela F, Paderno A, Missale F, Laborai A, Filauro M, Mora F, et al. Glottic exposure for transoral laser microsurgery: proposal of a mini-version of the laryngoscore. Laryngoscope. 2019; Jul. 129(7):1617–22.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiological Predictors of Difficult Laryngeal Exposure in Laryngomicrosurgery
- Severe bradycardia during suspension laryngoscopy performed after tracheal intubation using a direct laryngoscope with a curved blade: A case report
- Physical and Radiological Parameters to Predict Difficult Laryngeal Exposure in Patients Undergoing microlaryngeal Surgery
- An Introduction of the Systematic Review and Meta-Analysis
- Continuous Measurement of Suspension Force during Suspension Laryngoscopy: Preliminary Report