Clin Transplant Res.
2024 Mar;38(1):63-69. 10.4285/kjt.23.0064.
Hepatic artery vasospasm masquerading as early hepatic artery thrombosis in progressive familial intrahepatic cholestasis 3: a case report
- Affiliations
-
- 1Department of General Surgery, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India
- KMID: 2555999
- DOI: http://doi.org/10.4285/kjt.23.0064
Abstract
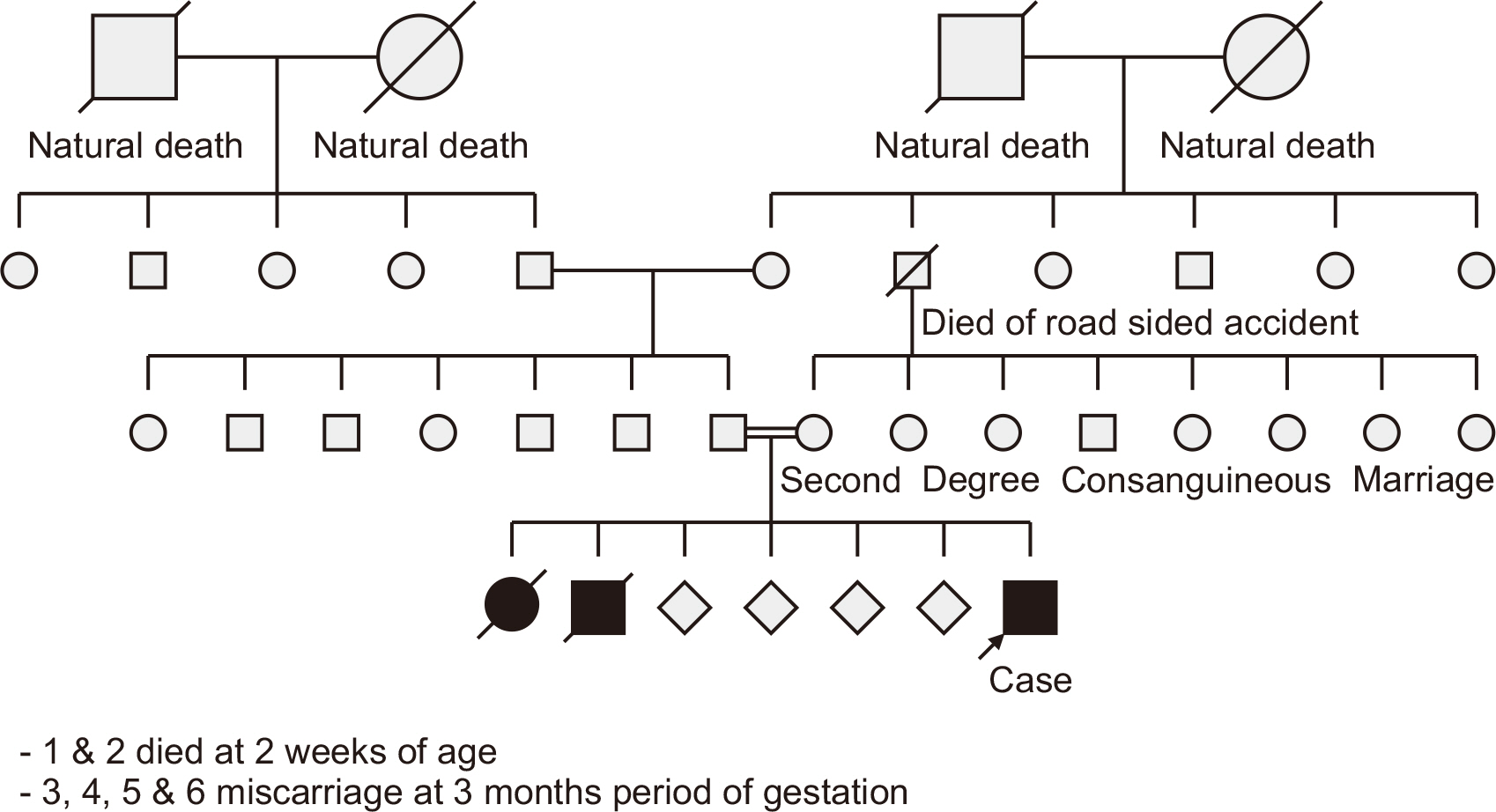
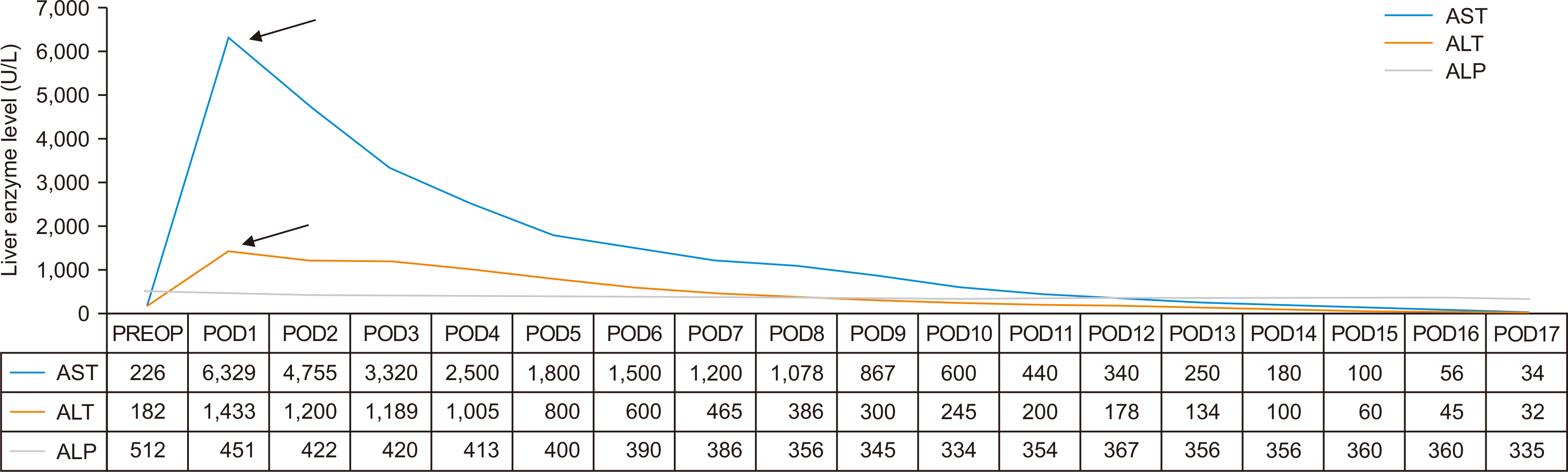
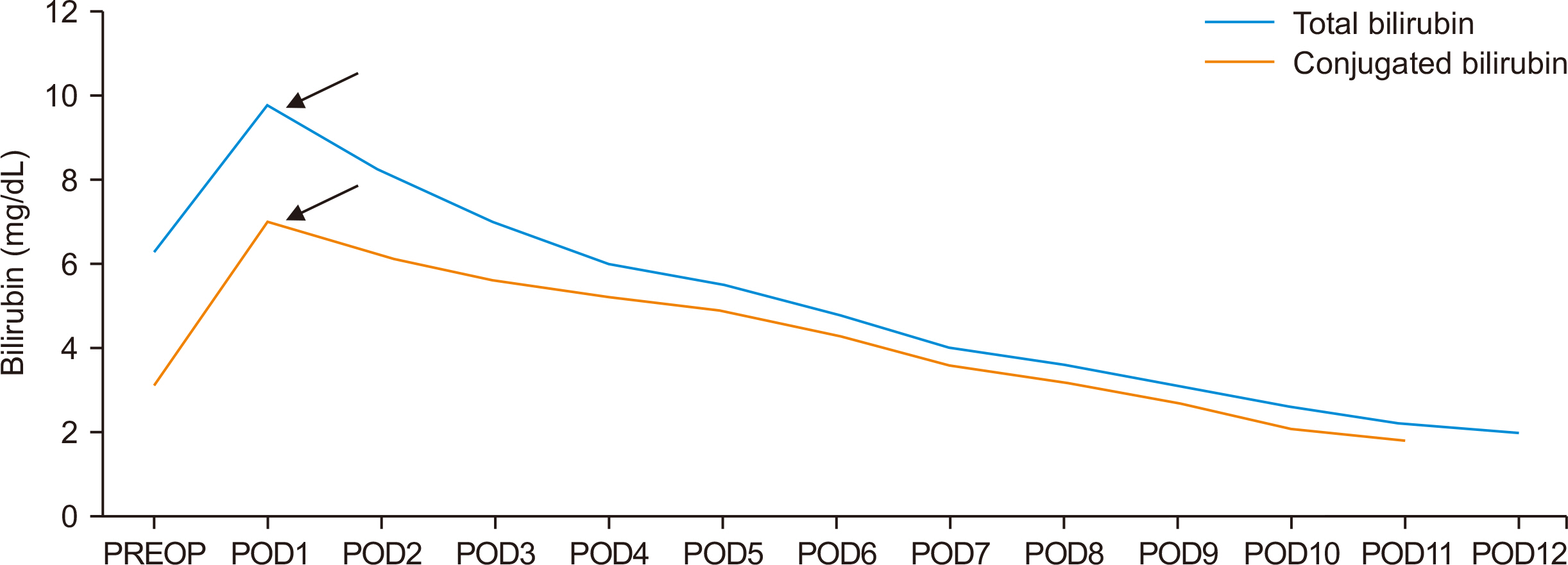
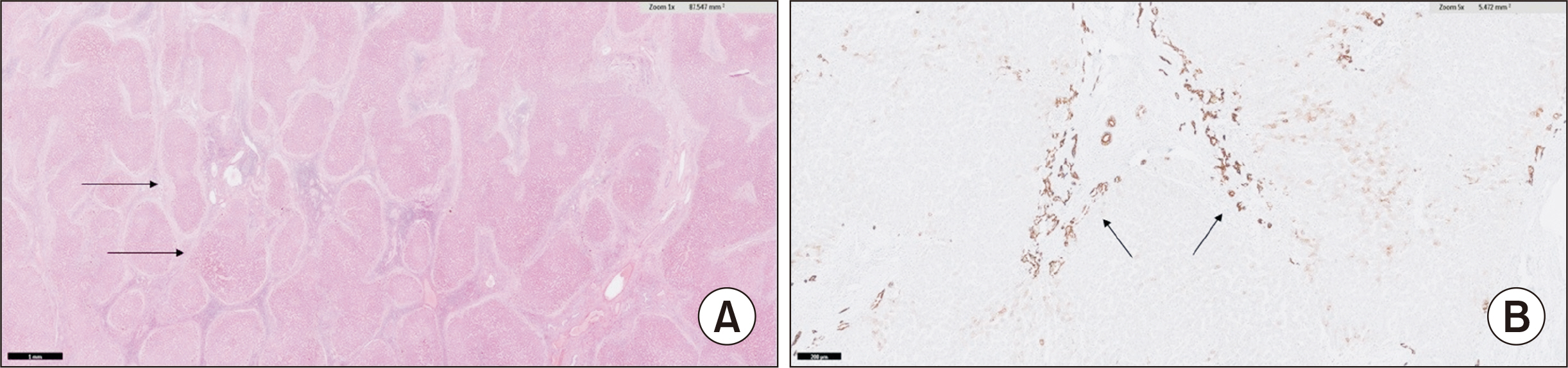
- Post-liver transplant (LT) hepatic artery vasospasm is a vascular complication that is not well recognized and its incidence is not known. As a possible sequela to vasospasm, hepatic artery thrombosis is the second major cause of allograft failure after primary nonfunction and its reported incidence is 2.9% in adults and 8.3% in pediatric LT. Lacuna in knowledge regarding early hepatic artery vasospasm post-LT makes it a difficult condition to diagnose and treat, as the initial ischemic insult on graft can have devastating consequences. We report a case of pediatric progressive familial intrahepatic cholestasis type 3-related chronic liver disease who underwent cadaveric orthotopic LT and postoperatively developed fever, worsening hypotension, and elevated liver enzymes with an absence of arterial flow in intrahepatic branches on Doppler ultrasound. Suspecting early hepatic artery thrombosis, the patient was re-explored and the graft hepatic artery was found to be in a state of vasospasm. Following the infusion of intra-arterial papaverine, urokinase, and intravenous nicorandil, there was an improvement in blood flow. The patient responded well and was discharged on postoperative day 23 with normal liver enzymes.
Keyword
Figure
Reference
-
1. Grodzicki M, Anysz-Grodzicka A, Remiszewski P, Cieślak B, Kotulski M, Kalinowski P, et al. 2011; Treatment of early hepatic artery thrombosis after liver transplantation. Transplant Proc. 43:3039–42. DOI: 10.1016/j.transproceed.2011.08.028. PMID: 21996219.
Article2. Heaton ND. 2013; Hepatic artery thrombosis: conservative management or retransplantation? Liver Transpl. 19 Suppl 2:S14–6. DOI: 10.1002/lt.23739. PMID: 24019107.
Article3. Chen W, Facciuto ME, Rocca JP, Marvin MR, Sheiner PA, Rachlin S, et al. 2006; Doppler ultrasonographic findings on hepatic arterial vasospasm early after liver transplantation. J Ultrasound Med. 25:631–8. DOI: 10.7863/jum.2006.25.5.631. PMID: 16632787.
Article4. Behera A, Kaman L, Dahiya D, Tandup C, Kalra N. 2022; Hepatic artery vasospasm masquerading as hepatic artery thrombosis in a case of deceased donor liver transplant. J Clin Exp Hepatol. 12:654–7. DOI: 10.1016/j.jceh.2021.09.004. PMID: 35535101. PMCID: PMC9077215.
Article5. Carter SA. Zwiebel WJ, editor. Hemodynamic considerations in peripheral and cerebrovascular disease. Introduction to vascular ultrasonography. 4th ed. WB Saunders;2000. p. 3–17.6. Richards RR, Seaber AV, Urbaniak JR. 1985; Chemically induced vasospasm: the effect of ischemia, vessel occlusion, and adrenergic blockade. Plast Reconstr Surg. 75:238–44. DOI: 10.1097/00006534-198502000-00016. PMID: 3969410.
Article7. Hellstrom HR. 1979; Evidence in favor of the vasospastic cause of coronary artery thrombosis. Am Heart J. 97:449–52. DOI: 10.1016/0002-8703(79)90391-0. PMID: 425878.
Article8. García-Criado A, Gilabert R, Salmerón JM, Nicolau C, Vilana R, Bianchi L, et al. 2003; Significance of and contributing factors for a high resistive index on Doppler sonography of the hepatic artery immediately after surgery: prognostic implications for liver transplant recipients. AJR Am J Roentgenol. 181:831–8. DOI: 10.2214/ajr.181.3.1810831. PMID: 12933490.9. Jeng LB, Lin PJ, Yao PC, Chen MF, Tsai KT, Chang CH. 1997; Impaired endothelium-dependent relaxation of human hepatic arteries after preservation with the University of Wisconsin solution. Arch Surg. 132:7–12. DOI: 10.1001/archsurg.1997.01430250009001. PMID: 9006546.
Article10. Acosta F, Diaz J, Sansano T, Palenciano CG, Reche M, Beltran R, et al. 2000; Evolution of the plasma concentration of norepinephrine in cirrhotic patients during liver transplantation. Transplant Proc. 32:2659–60. DOI: 10.1016/S0041-1345(00)01829-7. PMID: 11134749.
Article11. Pareja E, Cortes M, Navarro R, Sanjuan F, López R, Mir J. 2010; Vascular complications after orthotopic liver transplantation: hepatic artery thrombosis. Transplant Proc. 42:2970–2. DOI: 10.1016/j.transproceed.2010.07.063. PMID: 20970585.
Article12. Sakamoto Y, Harihara Y, Nakatsuka T, Kawarasaki H, Takayama T, Kubota K, et al. 1999; Rescue of liver grafts from hepatic artery occlusion in living-related liver transplantation. Br J Surg. 86:886–9. DOI: 10.1046/j.1365-2168.1999.01166.x. PMID: 10417559.
Article13. Hillier C, Watt PA, Spyt TJ, Thurston H. 1992; Contraction and relaxation of human internal mammary artery after intraluminal administration of papaverine. Ann Thorac Surg. 53:1033–7. DOI: 10.1016/0003-4975(92)90382-E. PMID: 1596124.
Article14. Lablanche JM, Bauters C, Leroy F, Bertrand ME. 1992; Prevention of coronary spasm by nicorandil: comparison with nifedipine. J Cardiovasc Pharmacol. 20 Suppl 3:S82–5. DOI: 10.1097/00005344-199206203-00014. PMID: 1282182.15. Hidalgo EG, Abad J, Cantarero JM, Fernández R, Parga G, Jover JM, et al. 1989; High-dose intra-arterial urokinase for the treatment of hepatic artery thrombosis in liver transplantation. Hepatogastroenterology. 36:529–32.16. Semba CP, Bakal CW, Calis KA, Grubbs GE, Hunter DW, Matalon TA, et al. 2000; Alteplase as an alternative to urokinase. J Vasc Interv Radiol. 11:279–87. DOI: 10.1016/S1051-0443(07)61418-3. PMID: 10735420.
Article17. Stange BJ, Glanemann M, Nuessler NC, Settmacher U, Steinmüller T, Neuhaus P. 2003; Hepatic artery thrombosis after adult liver transplantation. Liver Transpl. 9:612–20. DOI: 10.1053/jlts.2003.50098. PMID: 12783404.
Article18. Breguet R, Dondero F, Pupulim L, Goossens N, Sepulveda A, Francoz C, et al. 2019; Endovascular treatment of arterial complications after liver transplantation: long-term follow-up evaluated on Doppler ultrasound and magnetic resonance cholangiopancreatography. Cardiovasc Intervent Radiol. 42:381–8. DOI: 10.1007/s00270-018-2108-8. PMID: 30411152.
Article19. Singhal A, Stokes K, Sebastian A, Wright HI, Kohli V. 2010; Endovascular treatment of hepatic artery thrombosis following liver transplantation. Transpl Int. 23:245–56. DOI: 10.1111/j.1432-2277.2009.01037.x. PMID: 20030796.
Article20. Decrinis M, Pilger E, Stark G, Lafer M, Obernosterer A, Lammer J. 1993; A simplified procedure for intra-arterial thrombolysis with tissue-type plasminogen activator in peripheral arterial occlusive disease: primary and long-term results. Eur Heart J. 14:297–305. DOI: 10.1093/eurheartj/14.3.297. PMID: 8458348.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Presentation of Progressive Familial Intrahepatic Cholestasis Type 3 Mimicking Wilson Disease: Molecular Genetic Diagnosis and Response to Treatment
- Normal variation of hepatic artery
- Intra-arterial thrombolysis for early hepatic artery thrombosis following liver transplantation: a case report
- A Case of Successful Hepatic Retransplantation
- Variations in the origin of middle hepatic artery: a cadaveric study and implications for living donor liver transplantation