Clin Transplant Res.
2024 Mar;38(1):52-56. 10.4285/kjt.23.0056.
Overcoming the longest cold ischemia time yet seen in Korea using hypothermic machine perfusion in deceased donor kidney transplantation: a case report
- Affiliations
-
- 1Department of Surgery, Samsung Medical Center, Seoul, Korea
- 2Department of Surgery, Jeju National University Hospital, Jeju National University College of Medicine, Jeju, Korea
- 3Department of Premedicine, Amherst College, Amherst, MA, USA
- 4Department of Nursing, Jeju National University Hospital, Jeju, Korea
- KMID: 2555997
- DOI: http://doi.org/10.4285/kjt.23.0056
Abstract
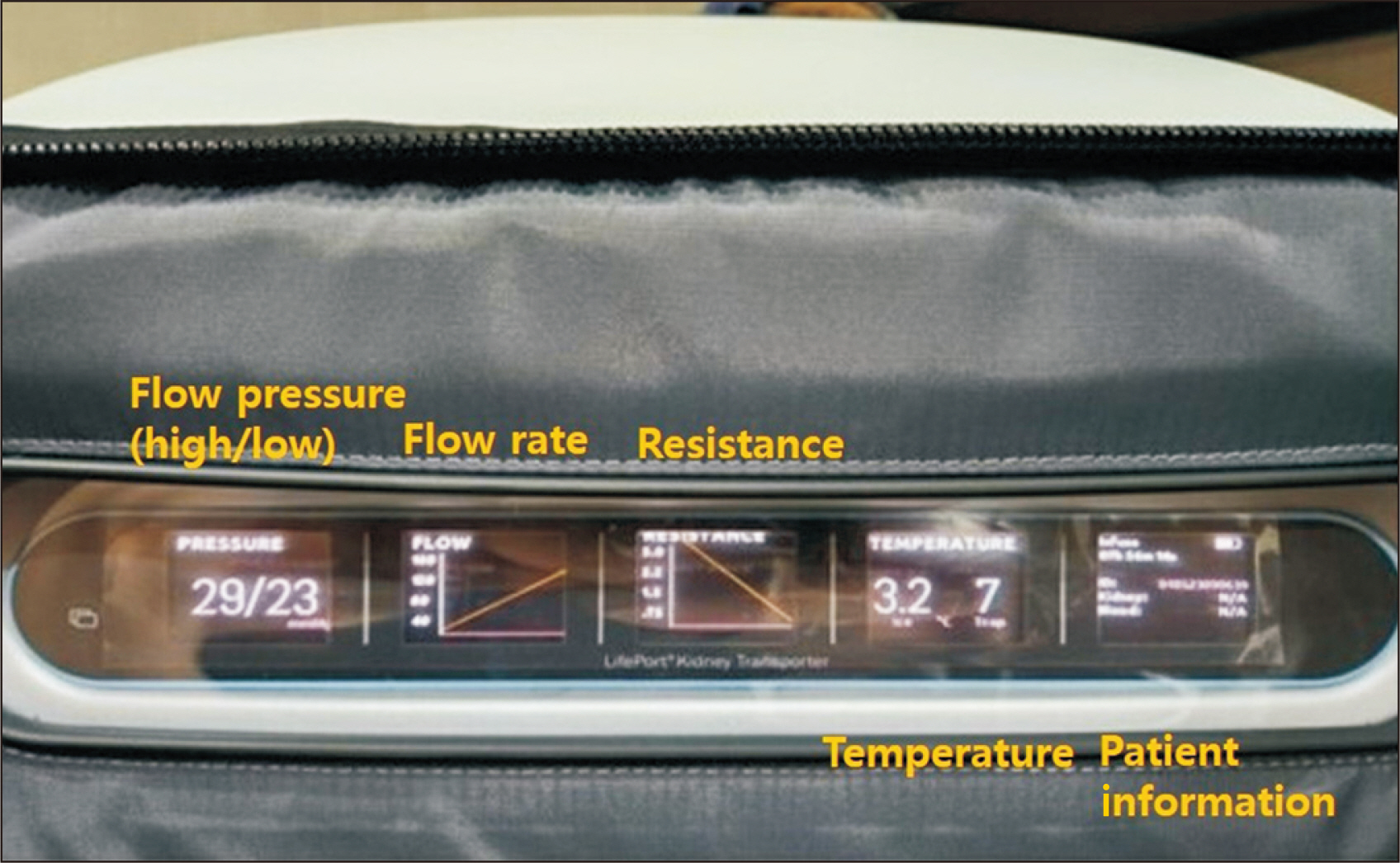
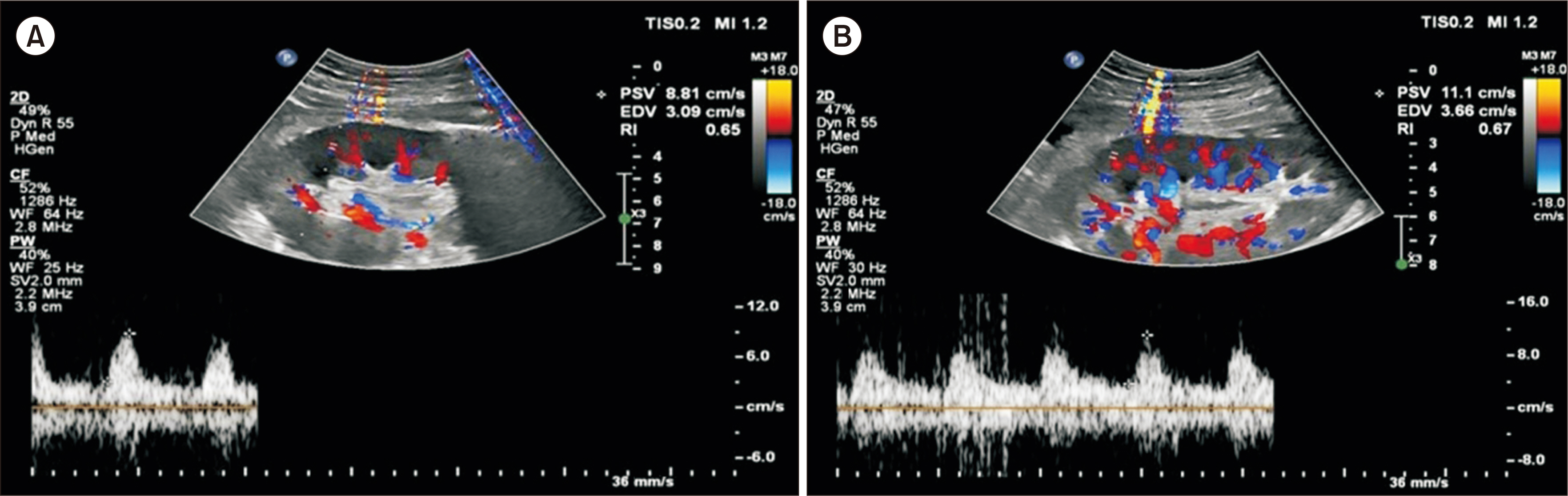
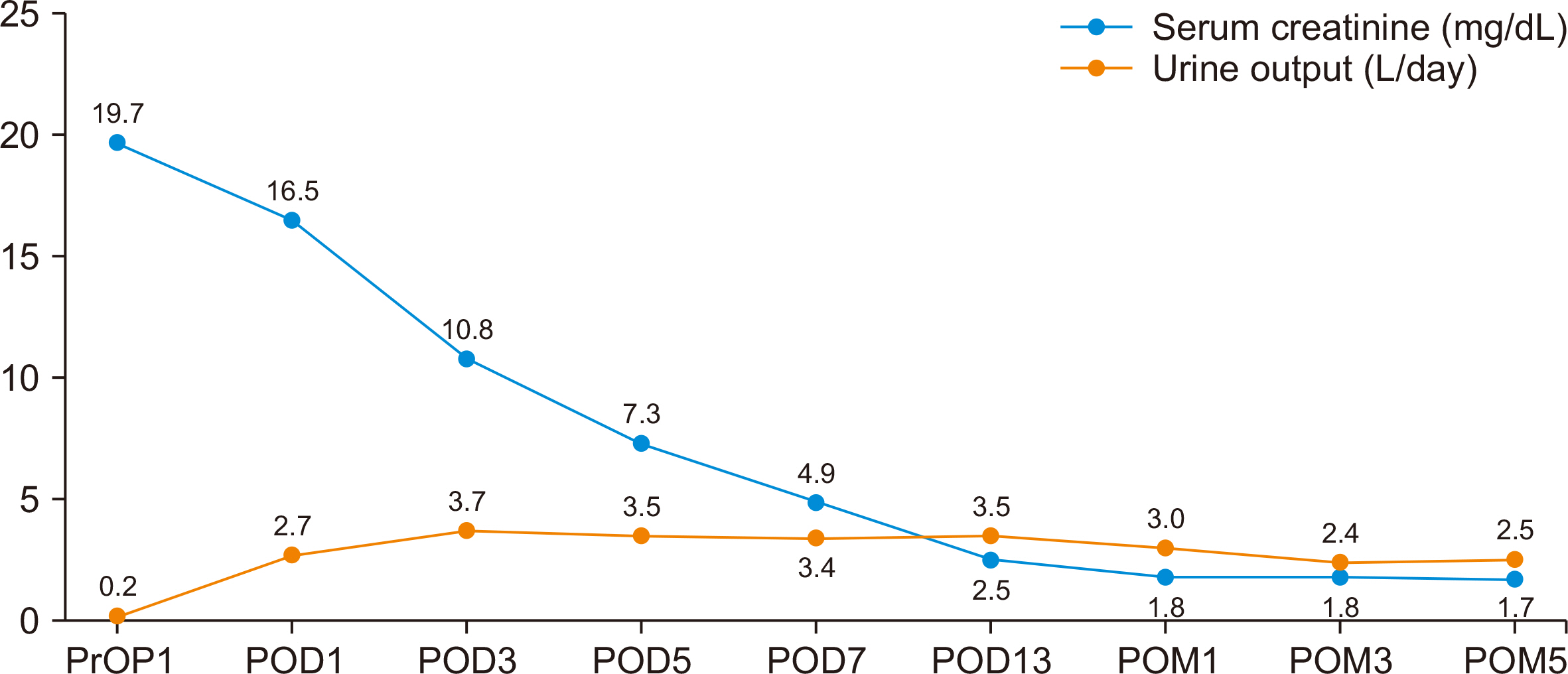
- To address a donor kidney shortage, marginal grafts have been applied in deceased donor kidney transplantation (DDKT). These grafts exhibit comparatively unfavorable outcomes, particularly when cold ischemia time (CIT) is prolonged. Hypothermic machine perfusion (HMP) has been investigated to mitigate the effects of prolonged CIT during graft transport. The present case involved successful management of the longest CIT recorded in Korea by employing HMP in DDKT. The donor was a 54-year-old man (Korean Kidney Donor Profile Index, 82%) with diabetes. The recipient, a 51-year-old man on peritoneal dialysis, had end-stage renal disease secondary to diabetic nephropathy. Following procurement, the left kidney was preserved using HMP. Inclement weather delayed graft transportation; consequently, the total CIT was 28 hours and 6 minutes, with the kidney preserved by HMP for 22 hours and 35 minutes. Postoperative graft function gradually recovered, and urine output was satisfactory. Delayed graft function was not observed, and the patient was discharged on postoperative day 13 without significant complications. Five months after surgery, his serum creatinine level was 1.7 mg/dL. Successful DDKT with a marginal donor graft via HMP, despite the longest CIT yet observed in Korea, underscores the usefulness of HMP in enhancing graft quality and preserving function.
Figure
Reference
-
1. Heilman RL, Smith ML, Kurian SM, Huskey J, Batra RK, Chakkera HA, et al. 2015; Transplanting kidneys from deceased donors with severe acute kidney injury. Am J Transplant. 15:2143–51. DOI: 10.1111/ajt.13260. PMID: 25808278.
Article2. Pascual J, Zamora J, Pirsch JD. 2008; A systematic review of kidney transplantation from expanded criteria donors. Am J Kidney Dis. 52:553–86. DOI: 10.1053/j.ajkd.2008.06.005. PMID: 18725015.
Article3. Hernández D, Estupiñán S, Pérez G, Rufino M, González-Posada JM, Luis D, et al. 2008; Impact of cold ischemia time on renal allograft outcome using kidneys from young donors. Transpl Int. 21:955–62. DOI: 10.1111/j.1432-2277.2008.00708.x. PMID: 18564990.
Article4. Kruszyna T, Richter P. 2021; Hypothermic machine perfusion of kidneys compensates for extended storage time: a single intervention with a significant impact. Transplant Proc. 53:1085–90. DOI: 10.1016/j.transproceed.2021.01.022. PMID: 33579549.
Article5. Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, Napieralski BP, et al. 2009; Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 360:7–19. DOI: 10.1056/NEJMoa0802289. PMID: 19118301.
Article6. Brat A, de Vries KM, van Heurn EW, Huurman VA, de Jongh W, Leuvenink HG, et al. 2022; Hypothermic machine perfusion as a national standard preservation method for deceased donor kidneys. Transplantation. 106:1043–50. DOI: 10.1097/TP.0000000000003845. PMID: 34172648. PMCID: PMC9038234.
Article7. Lo Faro ML, Akhtar MZ, Boffa C, Ploeg R. 2015; Should pulsatile preservation be the gold standard in kidney transplantation? Curr Transpl Rep. 2:105–12. DOI: 10.1007/s40472-015-0063-8.
Article8. Henry SD, Guarrera JV. 2012; Protective effects of hypothermic ex vivo perfusion on ischemia/reperfusion injury and transplant outcomes. Transplant Rev (Orlando). 26:163–75. DOI: 10.1016/j.trre.2011.09.001. PMID: 22074785.
Article9. Yuan X, Theruvath AJ, Ge X, Floerchinger B, Jurisch A, García-Cardeña G, et al. 2010; Machine perfusion or cold storage in organ transplantation: indication, mechanisms, and future perspectives. Transpl Int. 23:561–70. DOI: 10.1111/j.1432-2277.2009.01047.x. PMID: 20074082.
Article10. Shin YH, Lee T, Chang WB. 2022; The significance of the first living donor kidney transplantation in Jeju: a case report. Korean J Transplant. 36:231–5. DOI: 10.4285/kjt.22.0033. PMID: 36275993. PMCID: PMC9574429.
Article11. Kayler LK, Srinivas TR, Schold JD. 2011; Influence of CIT-induced DGF on kidney transplant outcomes. Am J Transplant. 11:2657–64. DOI: 10.1111/j.1600-6143.2011.03817.x. PMID: 22051325.
Article12. Lum EL, Homkrailas P, Abdalla B, Danovitch GM, Bunnapradist S. 2022; Cold ischemia time, kidney donor profile index, and kidney transplant outcomes: a cohort study. Kidney Med. 5:100570. DOI: 10.1016/j.xkme.2022.100570. PMID: 36632197. PMCID: PMC9827060.
Article13. Adani GL, Pravisani R, Tulissi P, Isola M, Calini G, Terrosu G, et al. 2021; Hypothermic machine perfusion can safely prolong cold ischemia time in deceased donor kidney transplantation: a retrospective analysis on postoperative morbidity and graft function. Artif Organs. 45:516–23. DOI: 10.1111/aor.13858. PMID: 33210745.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Overcoming the most prolonged cold ischemia time in Korea using hypothermic machine perfusion in deceased donor kidney transplantation
- The first use of hypothermic machine perfusion in Korea to recover a procured kidney graft and prevent prolonged cold ischemic time: a case report
- The significance of the first living donor kidney transplantation in Jeju: a case report
- Cold but not too cold: advances in hypothermic and normothermic organ perfusion
- Back on track: outcomes of deceased donor kidney recipients at national kidney and transplant institute during the COVID-19 pandemic