Korean J Transplant.
2022 Sep;36(3):231-235. 10.4285/kjt.22.0033.
The significance of the first living donor kidney transplantation in Jeju: a case report
- Affiliations
-
- 1Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Surgery, Jeju National University Hospital, Jeju, Korea
- KMID: 2533962
- DOI: http://doi.org/10.4285/kjt.22.0033
Abstract
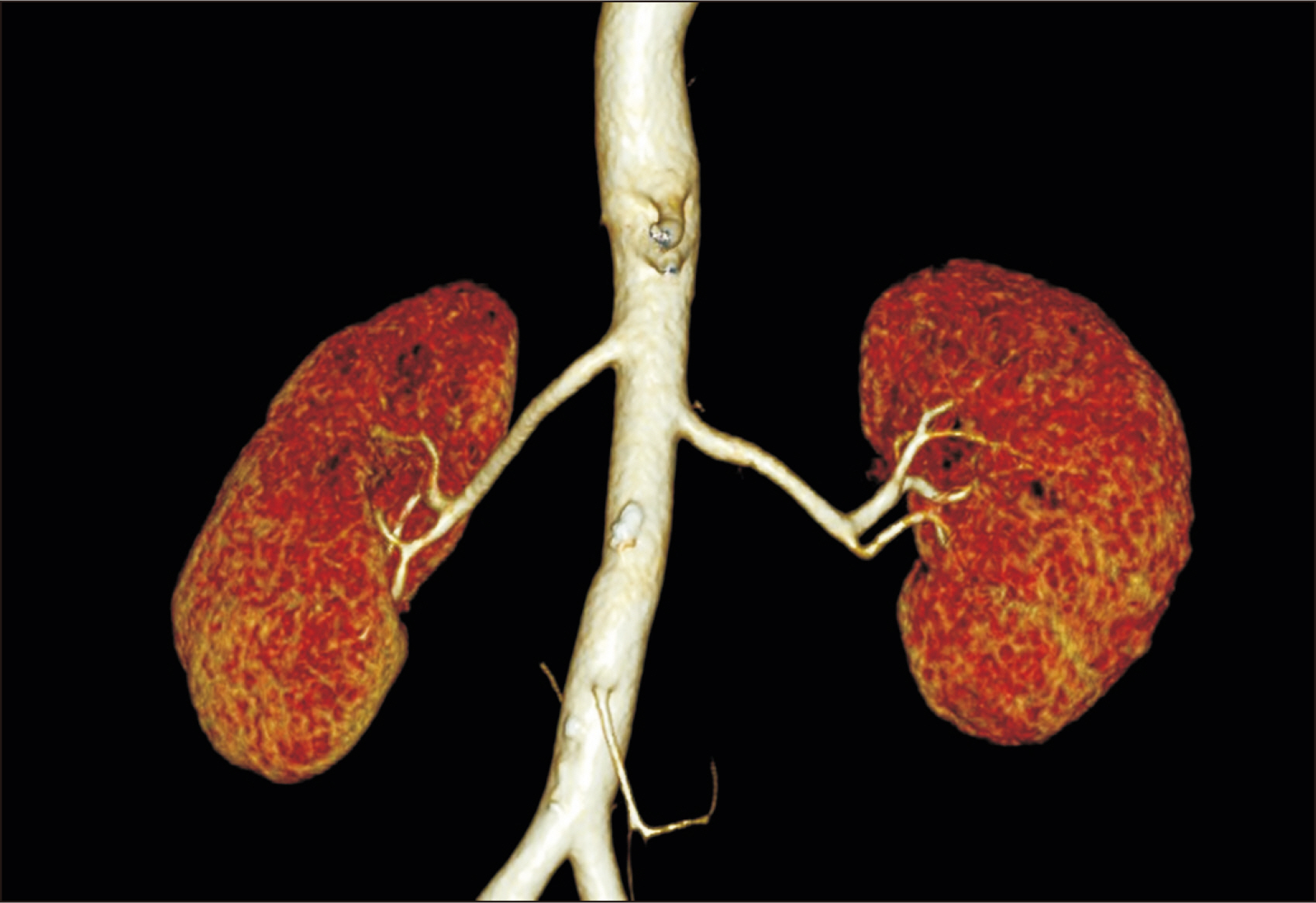
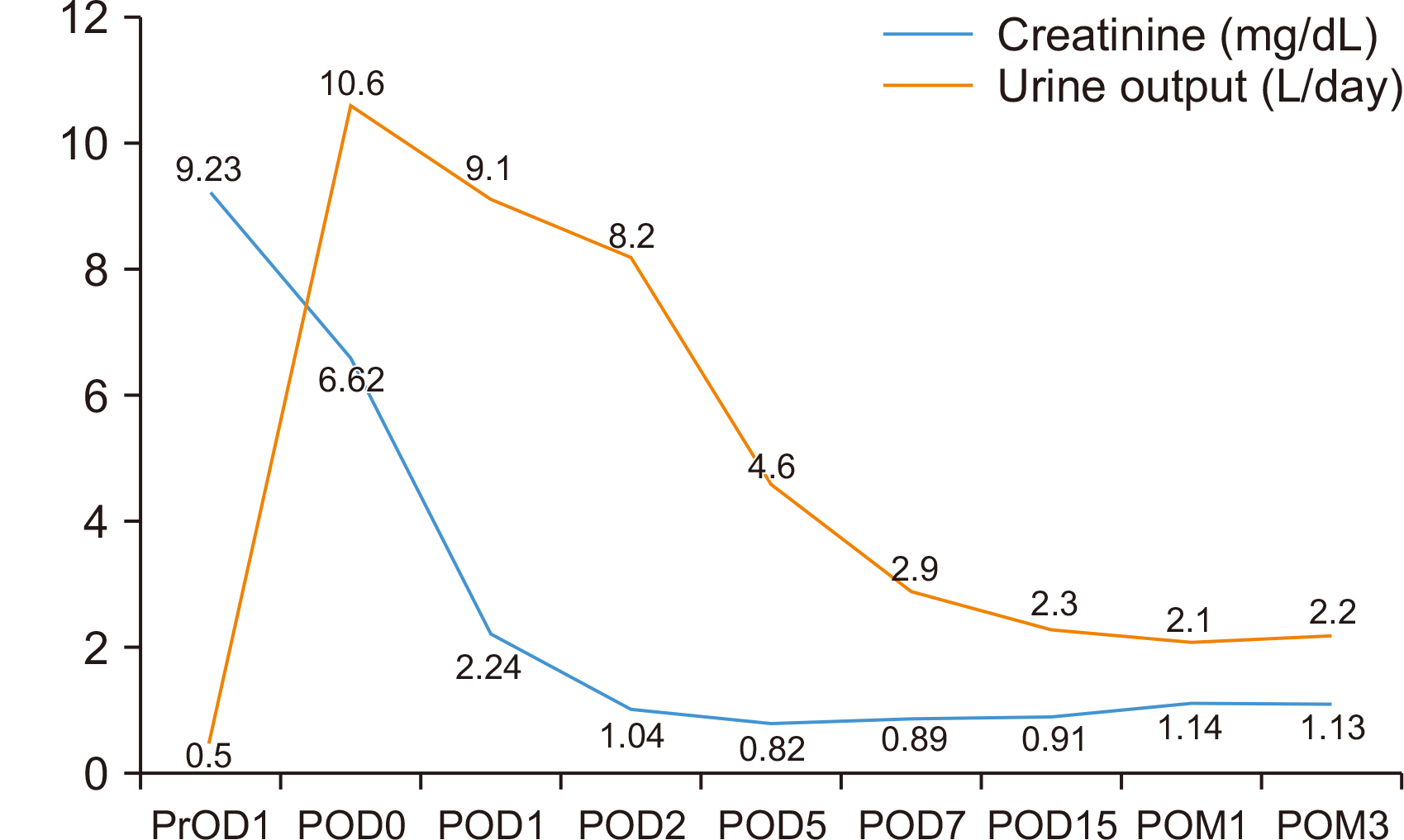
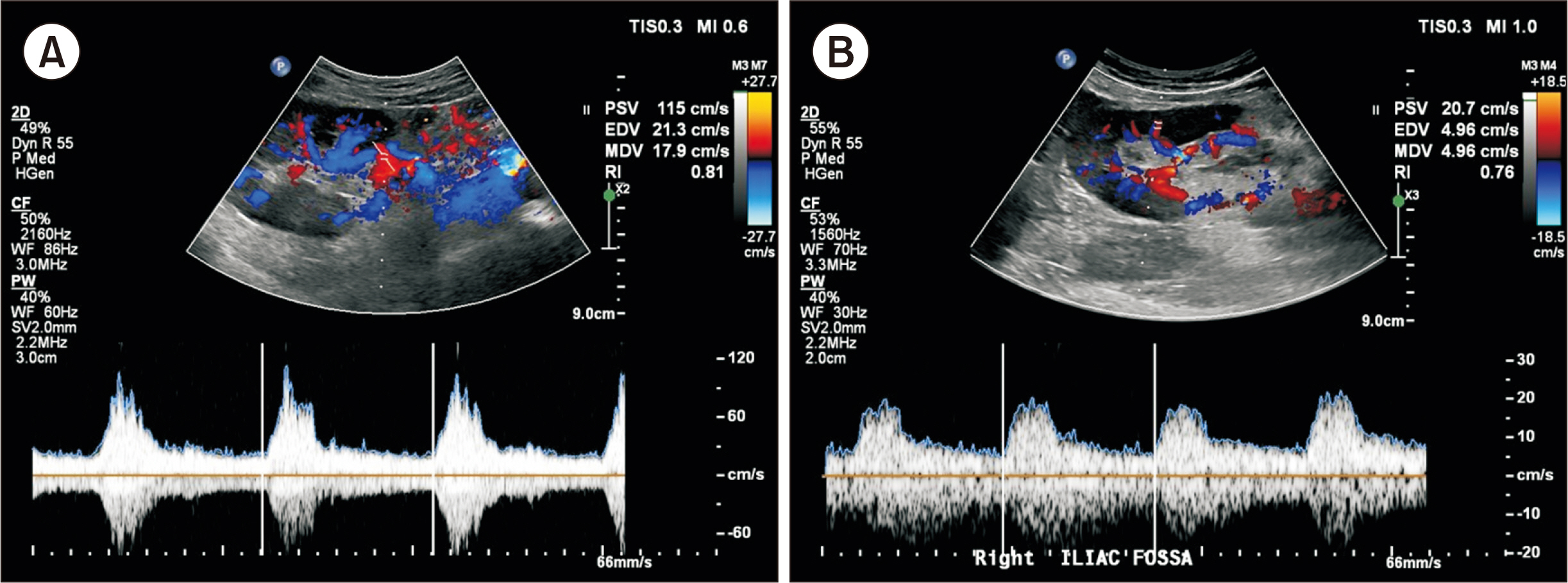
- To overcome the shortage of kidney donors, diverse methods have been utilized, in-cluding living donor kidney transplantation (LDKT) and extended criteria for deceased donor grafts. Currently, LDKT is a major treatment option. However, in Jeju, deceased donor kidney transplantation (DDKT) has been restricted due to the prolonged cold ischemia time (CIT) caused by the island’s geographic disadvantages and transportation limitations. We report the first LDKT in Jeju, which demonstrates a means of over-coming prolonged CIT. A 67-year-old male patient with diabetic nephropathy underwent a preemptive ABO compatible LDKT (ABO type O+) from his 62-year-old wife. The op-eration was uneventful, using anti-thymocyte globulin based on the recipient’s medical and immunologic risks. The patient recovered without significant complications and was discharged on postoperative day 15. Follow-up Doppler ultrasonography showed good blood flow to the kidney, and his serum creatinine levels steadily decreased and remained stable. The first successful LDKT in Jeju was significant in that kidney transplantation was implemented by compensating for its geographic limitations. In addition, we review machine perfusion as another method of avoiding prolonged CIT.
Figure
Cited by 2 articles
-
The first use of hypothermic machine perfusion in Korea to recover a procured kidney graft and prevent prolonged cold ischemic time: a case report
Young-Heun Shin, Taerim Ko, John Hee Park, Won-Bae Chang
Korean J Transplant. 2023;37(2):129-134. doi: 10.4285/kjt.23.0017.Overcoming the longest cold ischemia time yet seen in Korea using hypothermic machine perfusion in deceased donor kidney transplantation: a case report
Min-Ji Kim, Young-Heun Shin, Jason Kang, Taerim Ko, Won-Bae Chang
Clin Transplant Res. 2024;38(1):52-56. doi: 10.4285/kjt.23.0056.
Reference
-
1. Hernandez D, Alonso-Titos J, Armas-Padron AM, Ruiz-Esteban P, Cabello M, Lopez V, et al. 2018; Mortality in elderly waiting-list patients versus age-matched kidney transplant recipients: where is the risk? Kidney Blood Press Res. 43:256–75. DOI: 10.1159/000487684. PMID: 29490298.2. Ruggenenti P, Silvestre C, Boschiero L, Rota G, Furian L, Perna A, et al. 2017; Long-term outcome of renal transplantation from octogenarian donors: a multicenter controlled study. Am J Transplant. 17:3159–71. DOI: 10.1111/ajt.14459. PMID: 28792681.3. Lee S, Kim J, Shin M, Kim E, Moon J, Jung G, et al. 2010; Comparison of outcomes of living and deceased donor kidney grafts surviving longer than 5 years in Korea. Transplant Proc. 42:775–7. DOI: 10.1016/j.transproceed.2010.02.032. PMID: 20430168.4. Ko HW, Koo K, Shin CS, Park HS, Jeong JC, Kim S, et al. 2020; Clinical outcomes of the first 300 cases of kidney transplantation: a single-center retrospective cohort study. Korean J Transplant. 34:154–66. DOI: 10.4285/kjt.2020.34.3.154. PMID: 35769069. PMCID: PMC9187040.5. Brennan DC, Daller JA, Lake KD, Cibrik D, Del Castillo D. Thymoglobulin Induction Study Group. 2006; Rabbit antithymocyte globulin versus basiliximab in renal transplantation. N Engl J Med. 355:1967–77. DOI: 10.1056/NEJMoa060068. PMID: 17093248.6. Kidney Disease: Improving Global Outcomes (KDIGO) Transplant Work Group. 2009; KDIGO clinical practice guideline for the care of kidney transplant recipients. Am J Transplant. 9 Suppl 3:S1–155. DOI: 10.1111/j.1600-6143.2009.02834.x.7. Gurk-Turner C, Airee R, Philosophe B, Kukuruga D, Drachenberg C, Haririan A. 2008; Thymoglobulin dose optimization for induction therapy in high risk kidney transplant recipients. Transplantation. 85:1425–30. DOI: 10.1097/TP.0b013e31816dd596. PMID: 18497682.8. Opelz G, Döhler B. 2007; Multicenter analysis of kidney preservation. Transplantation. 83:247–53. DOI: 10.1097/01.tp.0000251781.36117.27. PMID: 17297393.9. Irish WD, Ilsley JN, Schnitzler MA, Feng S, Brennan DC. 2010; A risk prediction model for delayed graft function in the current era of deceased donor renal transplantation. Am J Transplant. 10:2279–86. DOI: 10.1111/j.1600-6143.2010.03179.x. PMID: 20883559.10. Darius T, Nath J, Mourad M. 2021; Simply adding oxygen during hypothermic machine perfusion to combat the negative effects of ischemia-reperfusion injury: fundamentals and current evidence for kidneys. Biomedicines. 9:993. DOI: 10.3390/biomedicines9080993. PMID: 34440197. PMCID: PMC8394874.11. Guy A, McGrogan D, Inston N, Ready A. 2015; Hypothermic machine perfusion permits extended cold ischemia times with improved early graft function. Exp Clin Transplant. 13:130–7.12. Kvietkauskas M, Leber B, Strupas K, Stiegler P, Schemmer P. 2020; Machine perfusion of extended criteria donor organs: immunological aspects. Front Immunol. 11:192. DOI: 10.3389/fimmu.2020.00192. PMID: 32180769. PMCID: PMC7057848.13. Taylor MJ, Baicu SC. Current state of hypothermic machine perfusion preservation of organs: The clinical perspective. Cryobiology. 2010; Jul. 60(3 Suppl):S20–35. DOI: 10.1016/j.cryobiol.2009.10.006. PMID: 19857479. PMCID: PMC2891866.14. Moers C, Smits JM, Maathuis MH, Treckmann J, van Gelder F, Napieralski BP, et al. 2009; Machine perfusion or cold storage in deceased-donor kidney transplantation. N Engl J Med. 360:7–19. DOI: 10.1056/NEJMoa0802289. PMID: 19118301.15. Brat A, de Vries KM, van Heurn EW, Huurman VA, de Jongh W, Leuvenink HG, et al. 2022; Hypothermic machine perfusion as a national standard preservation method for deceased donor kidneys. Transplantation. 106:1043–50. DOI: 10.1097/TP.0000000000003845. PMID: 34172648. PMCID: PMC9038234.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Kidney Transplantation after ex vivo Repair of an Aneurysm of the Donor Renal Artery
- The use of polytetrafluoroethylene graft for damaged renal artery in ABO-incompatible living donor kidney transplantation: a case report
- Evaluation of the Recipient and Donor in Living Kidney Transplantation
- Exchange Living-donor Kidney Transplantation: The Present and Future
- Results of living donor renal transplantation using donor kidneys with multiple renal arteries