Ann Hepatobiliary Pancreat Surg.
2024 May;28(2):203-213. 10.14701/ahbps.23-112.
Prognostic factors and predictive models in hot gallbladder surgery: A prospective observational study in a high-volume center
- Affiliations
-
- 1Surgical Emergency Unit, John Radcliffe Hospital, Oxford University Hospitals NHS Foundation Trust, Oxford, UK
- 2University of Oxford School of Medicine, Oxford, UK
- 3Digestive and Emergency Surgery Unit, S.Maria Hospital, Terni, Italy
- KMID: 2555930
- DOI: http://doi.org/10.14701/ahbps.23-112
Abstract
- Backgrounds/Aims
The standard treatment for acute cholecystitis, biliary pancreatitis and intractable biliary colics (“hot gallbladder”) is emergency laparoscopic cholecystectomy (LC). This paper aims to identify the prognostic factors and create statistical models to predict the outcomes of emergency LC for “hot gallbladder.”
Methods
A prospective observational cohort study was conducted on 466 patients having an emergency LC in 17 months. Primary endpoint was “suboptimal treatment,” defined as the use of escape strategies due to the impossibility to complete the LC. Secondary endpoints were postoperative morbidity and length of postoperative stay.
Results
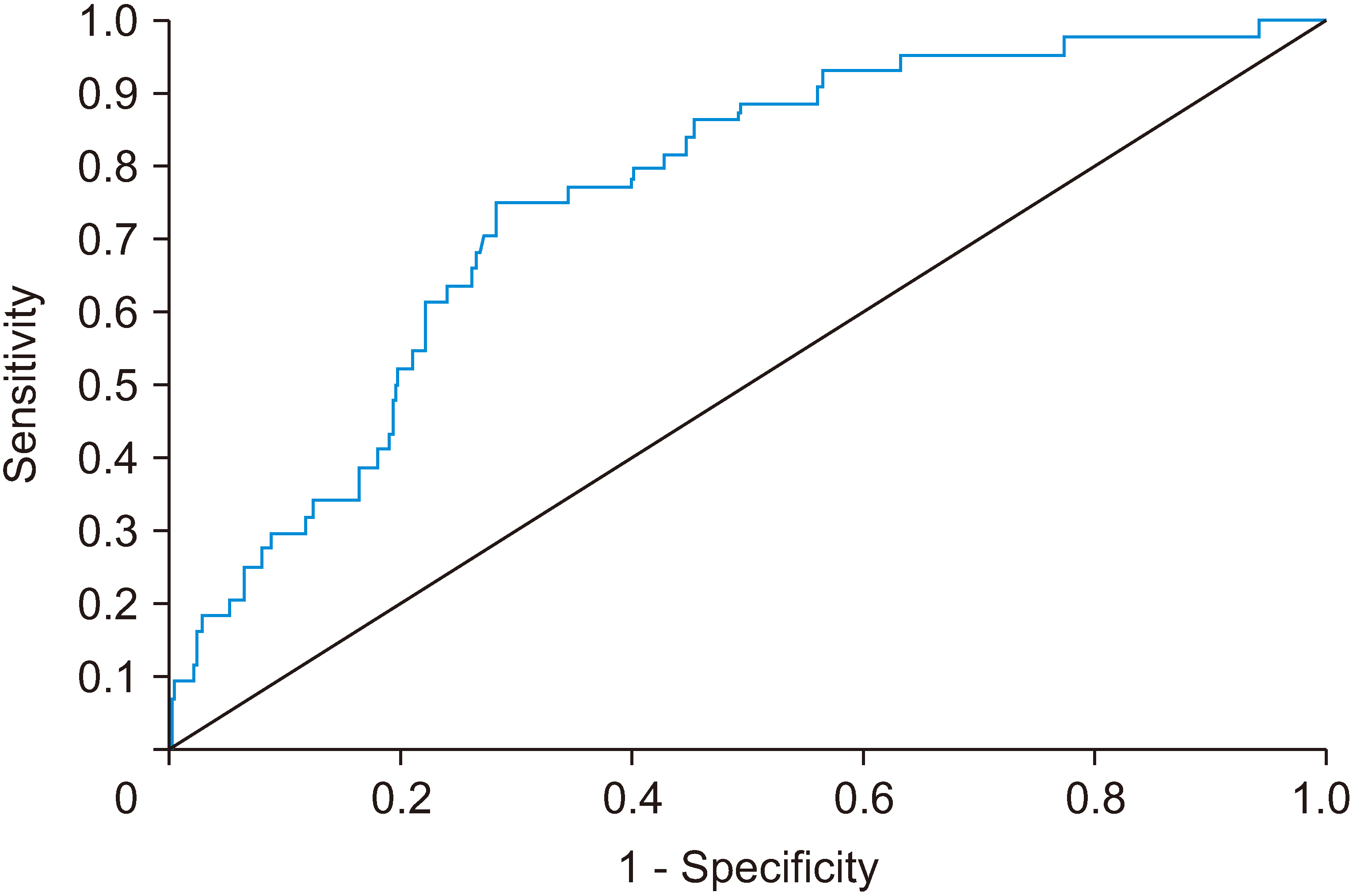
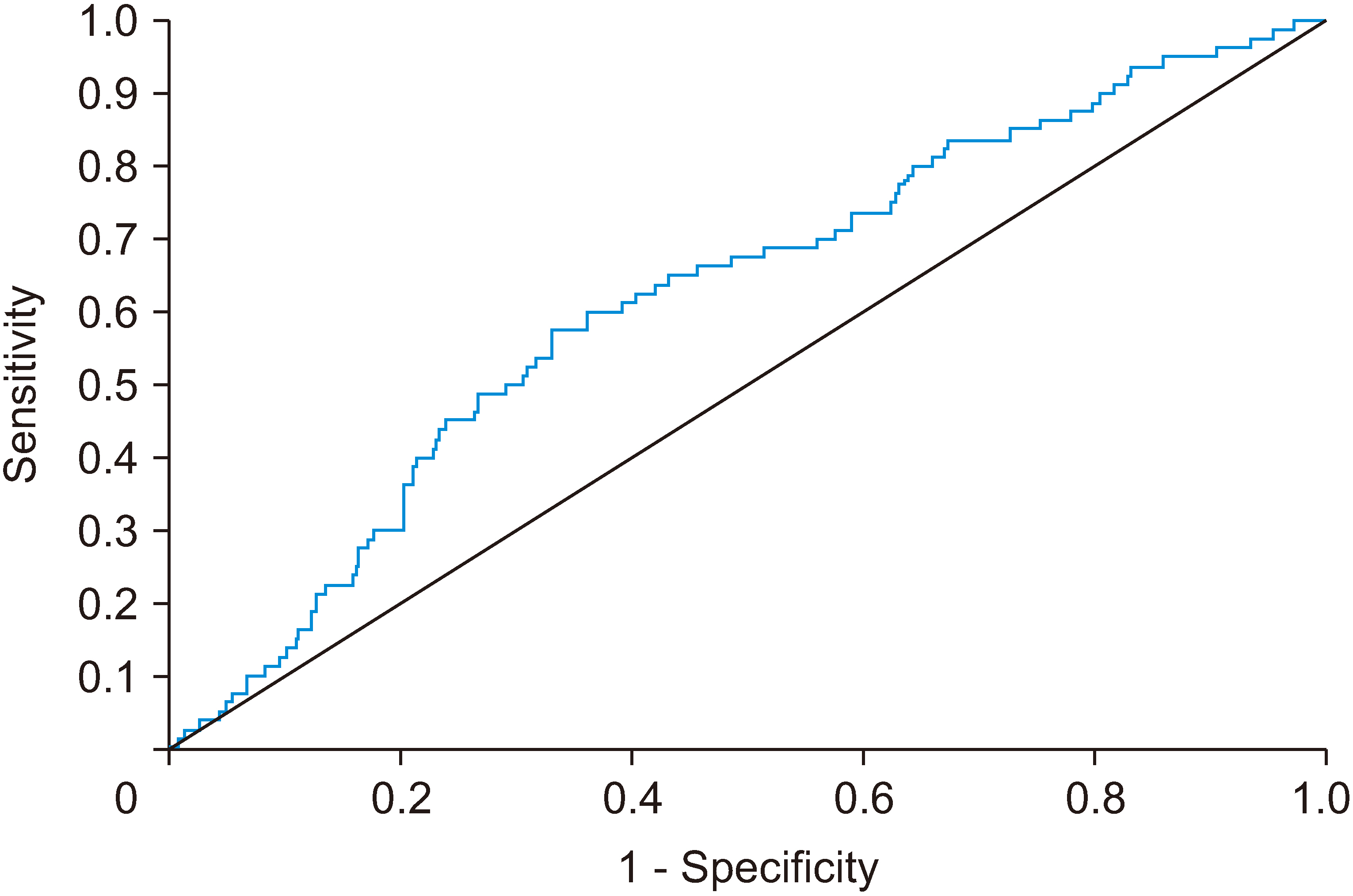
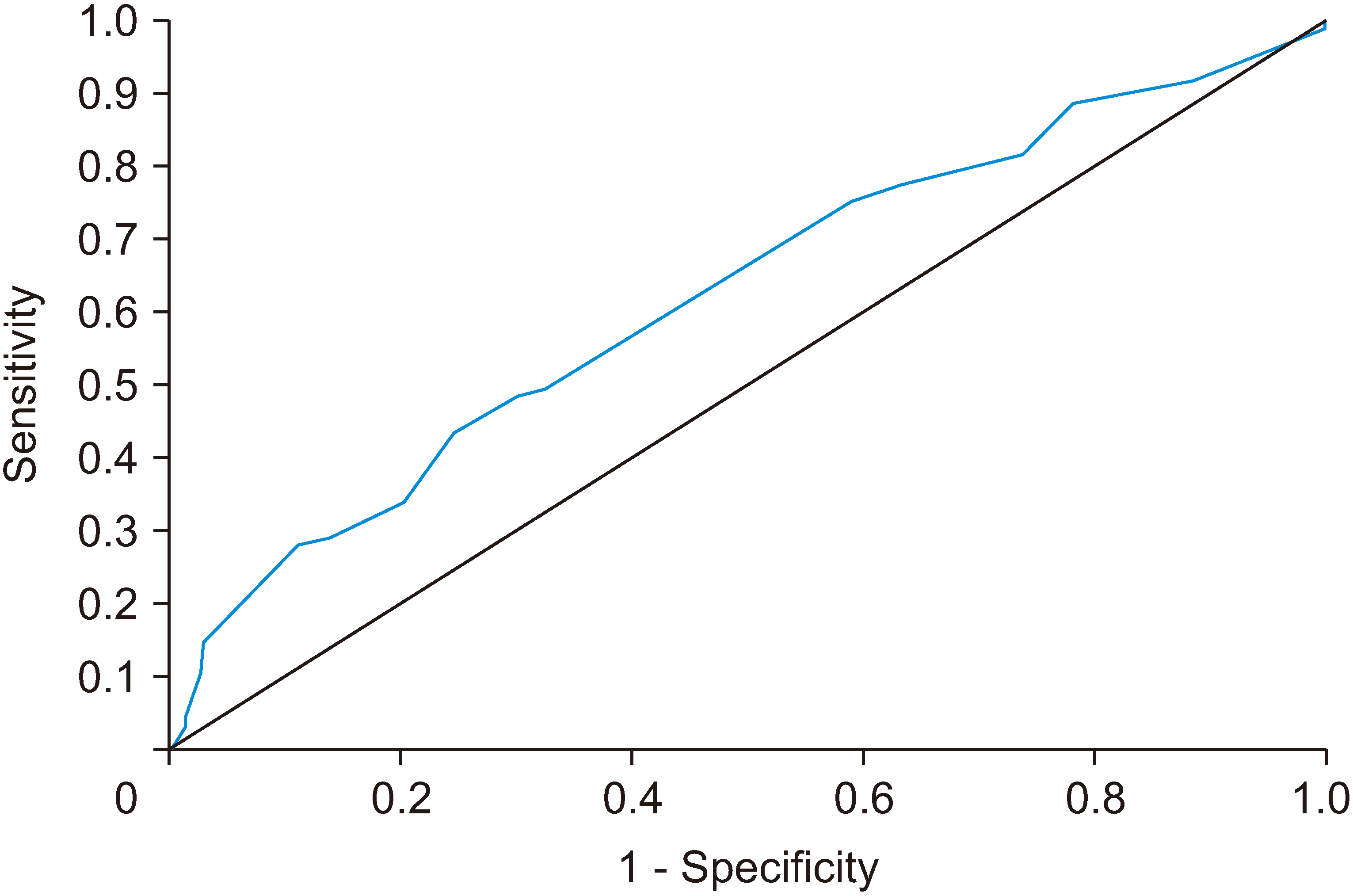
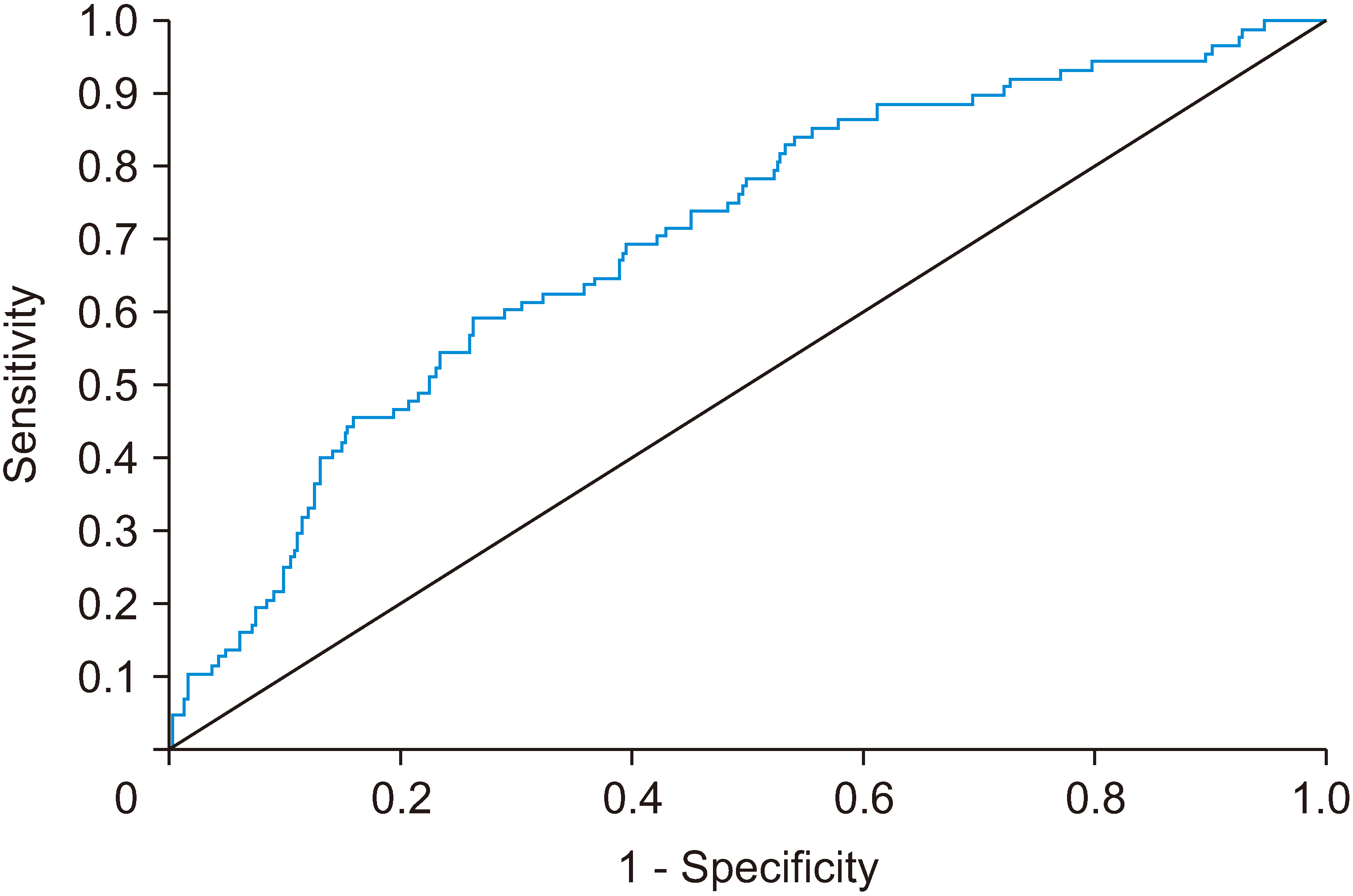
About 10% of patients had a “suboptimal treatment” predicted by age and low albumin. Postop morbidity was 17.2%, predicted by age, admission day, and male sex. Postoperative length of stay was correlated to age, low albumin, and delayed surgery.
Conclusions
Several predictive prognostic factors were found to be related to poor emergency LC outcomes. These can be useful in the decision-making process and to inform patients of risks and benefits of an emergency vs. delayed LC for hot gallbladder.
Figure
Reference
-
References
1. Everhart JE, Rulh CE. 2009; Burden of digestive diseases in the United States part I: overall and upper gastrointestinal diseases. Gastroenterology. 136:376–386. DOI: 10.1053/j.gastro.2008.12.015. PMID: 19124023.
Article2. Gurusamy KS, Davidson BR. 2014; Gallstones. BMJ. 348:g2669. DOI: 10.1136/bmj.g2669. PMID: 24755732.
Article3. Tebala GD, Milani MS, Bignell M, Bond-Smith G, Lewis C, Cirocchi R, et al. 2022; Emergency surgery admissions and the COVID-19 pandemic: did the first wave really change our practice? Results of an ACOI/WSES international audit on 6263 patients. World J Emerg Surg. 17:8. DOI: 10.1186/s13017-022-00407-1. PMID: 35090519. PMCID: PMC8795350.
Article4. Takada T. Tokyo Guidelines 2018: updated Tokyo Guidelines for the management of acute cholangitis/acute cholecystitis. J Hepatobiliary Pancreat Sci. 2018; 25:1–2. DOI: 10.1002/jhbp.526. PMID: 29334699.
Article5. STROBE Guidelines [Internet]. Available from: https://www.strobe-statement.org/index.php?id=strobe-home. STROBE;cited 2021 Feb 14.6. Maldjian PD, Ghesani N, Ahmed S, Liu Y. 2007; Adenomyomatosis of the gallbladder: another cause for a "hot" gallbladder on 18F-FDG PET. AJR Am J Roentgenol. 189:W36–W38. DOI: 10.2214/AJR.05.1284. PMID: 17579133.7. Imtiaz M, Prakash S, Iqbal S, Fernandes R, Shah A, Shrestha AK, et al. 2022; ‘Hot gallbladder service’ by emergency general surgeons: is this safe and feasible? J Min Access Surg. 18:45–50. DOI: 10.4103/jmas.JMAS_271_20. PMID: 33885031. PMCID: PMC8830581.
Article8. Bundgaard NS, Bohm A, Hansted AK, Skovsen AP. 2021; Early laparoscopic cholecystectomy for acute cholecystitis is safe regardless of timing. Langenbecks Arch Surg. 406:2367–2373. DOI: 10.1007/s00423-021-02229-2. PMID: 34109473.
Article9. Acar N, Acar T, Sür Y, Bağ H, Kar H, Bozok Y, et al. 2021; Is subtotal cholecystectomy safe and feasible? Short- and long-term results. J Hepatobiliary Pancreat Sci. 28:263–271. DOI: 10.1002/jhbp.847. PMID: 33058478.
Article10. Tang A, Cohan CM, Beattie G, Mooney CM, Chiang A, Keeley JA. 2021; Factors that predict the need for subtotal cholecystectomy. Am Surg. 87:1245–1251. DOI: 10.1177/0003134820979783. PMID: 33339461.
Article11. Terho PM, Leppäniemi AK, Mentula PJ. 2016; Laparoscopic cholecystectomy for acute calculous cholecystitis: a retrospective study assessing risk factors for conversion and complications. World J Emerg Surg. 11:54. DOI: 10.1186/s13017-016-0111-4. PMID: 27891173. PMCID: PMC5112701.
Article12. Wevers KP, van Westreenen HL, Patijin GA. 2013; Laparoscopic cholecystectomy in acute cholecystitis: C-reactive protein level combined with age predicts conversion. Surg Laparosc Endosc Percutan Tech. 23:163–166. DOI: 10.1097/SLE.0b013e31826d7fb0. PMID: 23579511.13. Stanisic V, Milicevic M, Kocev N, Stojanovic M, Vlaovic D, Babic I, et al. 2014; Prediction of difficulties in laparoscopic cholecystectomy on the base of routinely available parameters in a smaller regional hospital. Eur Rev Med Pharmacol Sci. 18:1204–1211.14. Inoue K, Ueno T, Douchi D, Shima K, Goto S, Takahashi M, et al. 2017; Risk factors for difficulty of laparoscopic cholecystectomy in grade II acute cholecystitis according to the Tokyo guidelines 2013. BMC Surg. 17:114. DOI: 10.1186/s12893-017-0319-6. PMID: 29183352. PMCID: PMC5706415.
Article15. Yol S, Kartal A, Vatansev C, Aksoy F, Toy H. 2006; Sex as a factor in conversion from laparoscopic cholecystectomy to open surgery. JSLS. 10:359–363.16. Ishizuka M, Shibuya N, Shimoda M, Kato M, Aoki T, Kubota K. 2016; Preoperative hypoalbuminemia is an independent risk factor for conversion from laparoscopic to open cholecystectomy in patients with cholecystolithiasis. Asian J Endosc Surg. 9:275–280. DOI: 10.1111/ases.12301. PMID: 27283337.
Article17. Eckart A, Struja T, Kutz A, Baumgartner A, Baumgartner T, Zurfluh S, et al. 2020; Relationship of nutritional status, inflammation, and serum albumin levels during acute illness: a prospective study. Am J Med. 133:713–722.e7. DOI: 10.1016/j.amjmed.2019.10.031. PMID: 31751531.
Article18. Ishida S, Hashimoto I, Seike T, Abe Y, Nakaya Y, Nakanishi H. 2014; Serum albumin levels correlate with inflammation rather than nutrition supply in burns patients: a retrospective study. J Med Invest. 61:361–368. DOI: 10.2152/jmi.61.361. PMID: 25264055.
Article19. Ambe PC, Köhler L. 2015; Is the male gender an independent risk factor for complications in patients undergoing laparoscopic cholecystectomy for acute cholecystitis? Int Surg. 100:854–859. DOI: 10.9738/INTSURG-D-14-00151.1. PMID: 26011206. PMCID: PMC4452974.
Article20. Braunwarth E, Rumpf B, Primavesi F, Pereyra D, Hochleitner M, Göbel G, et al. 2020; Sex differences in disease presentation, surgical and oncological outcome of liver resection for primary and metastatic liver tumours-a retrospective multicenter study. PLoS One. 15:e0243539. DOI: 10.1371/journal.pone.0243539. PMID: 33315924. PMCID: PMC7735568.21. Al-Taki M, Sukkarieh HG, Hoballah JJ, Jamali SF, Habbal M, Masrouha KZ, et al. 2018; Effect of gender on postoperative morbidity and mortality outcomes: a retrospective cohort study. Am Surg. 84:377–386. DOI: 10.1177/000313481808400321. PMID: 29559052.
Article22. Zapf MA, Kothari AN, Markossian T, Gupta GN, Blackwell RH, Wai PY, et al. 2015; The "weekend effect" in urgent general operative procedures. Surgery. 158:508–514. DOI: 10.1016/j.surg.2015.02.024. PMID: 26013983. PMCID: PMC5226376.
Article23. Tebala GD, Milani MS, Cirocchi R, Bignell M, Bond-Smith G, Lewis C, et al. 2022; The weekend effect on the provision of emergency surgery before and during the COVID-19 pandemic: case-control analysis of a retrospective multicentre database. World J Emerg Surg. 17:22. DOI: 10.1186/s13017-022-00425-z. PMID: 35488247. PMCID: PMC9051756.24. Hoehn RS, Go DE, Dhar VK, Kim Y, Hanseman DJ, Wima K, et al. 2018; Understanding the "weekend effect" for emergency general surgery. J Gastrointest Surg. 22:321–328. DOI: 10.1007/s11605-017-3592-x. PMID: 28963604.
Article25. Sathiyakumar V, Molina CS, Thakore RV, Obremskey WT, Sethi MK. 2015; ASA score as a predictor of 30-day perioperative readmission in patients with orthopaedic trauma injuries. J Orthop Trauma. 29:e127–e132. DOI: 10.1097/BOT.0000000000000200. PMID: 25072291.
Article26. Evans LA, Goeteyn J, Carter B, Greig M, Tay HS, McCormack C, et al. 2017; Preoperative kidney function linked to mortality and readmission outcomes at Day 90 and 30 in older emergency surgical patients. Eur Geriatr Med. 8:216–220. DOI: 10.1016/j.eurger.2017.03.001.
Article27. Sawalha K, Al-Akchar M, Ibrahim A, Buhnerkempe M, Koester C, Salih M, et al. 2021; Impact of chronic kidney disease on in-hospital outcomes and readmission rate after edge-to-edge transcatheter mitral valve repair. Catheter Cardiovasc Interv. 97:E569–E579. DOI: 10.1002/ccd.29188. PMID: 32969155.
Article28. Chong JU, Lee JH, Yoon YC, Kwon KH, Cho JY, Kim SJ, et al. 2016; Influencing factors on postoperative hospital stay after laparoscopic cholecystectomy. Korean J Hepatobiliary Pancreat Surg. 20:12–16. DOI: 10.14701/kjhbps.2016.20.1.12. PMID: 26925145. PMCID: PMC4767266.
Article29. Mitton J, Daliya P, Singh P, Parsons SL, Lobo DN, Lilford R, et al. 2021; Outcomes following an index emergency admission with cholecystitis: a national cohort study. Ann Surg. 274:367–374. DOI: 10.1097/SLA.0000000000003599. PMID: 31567508.30. Di Martino M, Mora-Guzmán I, Vaello Jodra V, Sanjuanbenito Dehesa A, Morales-García D, Caiña Ruiz A, et al. 2021; Laparoscopic cholecystectomy for acute cholecystitis: is the surgery still safe beyond the 7-day barrier? A multicentric observational study. Updates Surg. 73:261–272. DOI: 10.1007/s13304-020-00924-1. PMID: 33211289.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sonographic measurement of the gallbladder
- Analysis of Prognostic Factors after Curative Resection for Gallbladder Carcinoma
- Surgical outcome and prognostic factors in patients with gallbladder carcinoma
- Analysis of Prognostic Factors after Surgery for Gallbladder Cancer
- Predictive factors for gangrene complication in acute calculous cholecystitis