Ann Hepatobiliary Pancreat Surg.
2024 May;28(2):155-160. 10.14701/ahbps.23-138.
Incidence of incisional hernia following liver surgery for colorectal liver metastases. Does the laparoscopic approach reduce the risk? A comparative study
- Affiliations
-
- 1Department of General & HPB Surgery, East Lancashire Hospitals NHS Trust, Royal Blackburn Hospital, Blackburn, UK
- 2Blackburn Research Innovation Development Group in General Surgery (BRIDGES), Royal Blackburn Hospital, Blackburn, UK
- 3University Hospitals of Morecambe Bay NHS Foundation Trust, Royal Lancaster Infirmary, Lancaster, UK
- KMID: 2555928
- DOI: http://doi.org/10.14701/ahbps.23-138
Abstract
- Backgrounds/Aims
No reports to compare incisional hernia (IH) incidence between laparoscopic and open colorectal liver metastases (CRLM) resections have previously been made. This is the first comparative study.
Methods
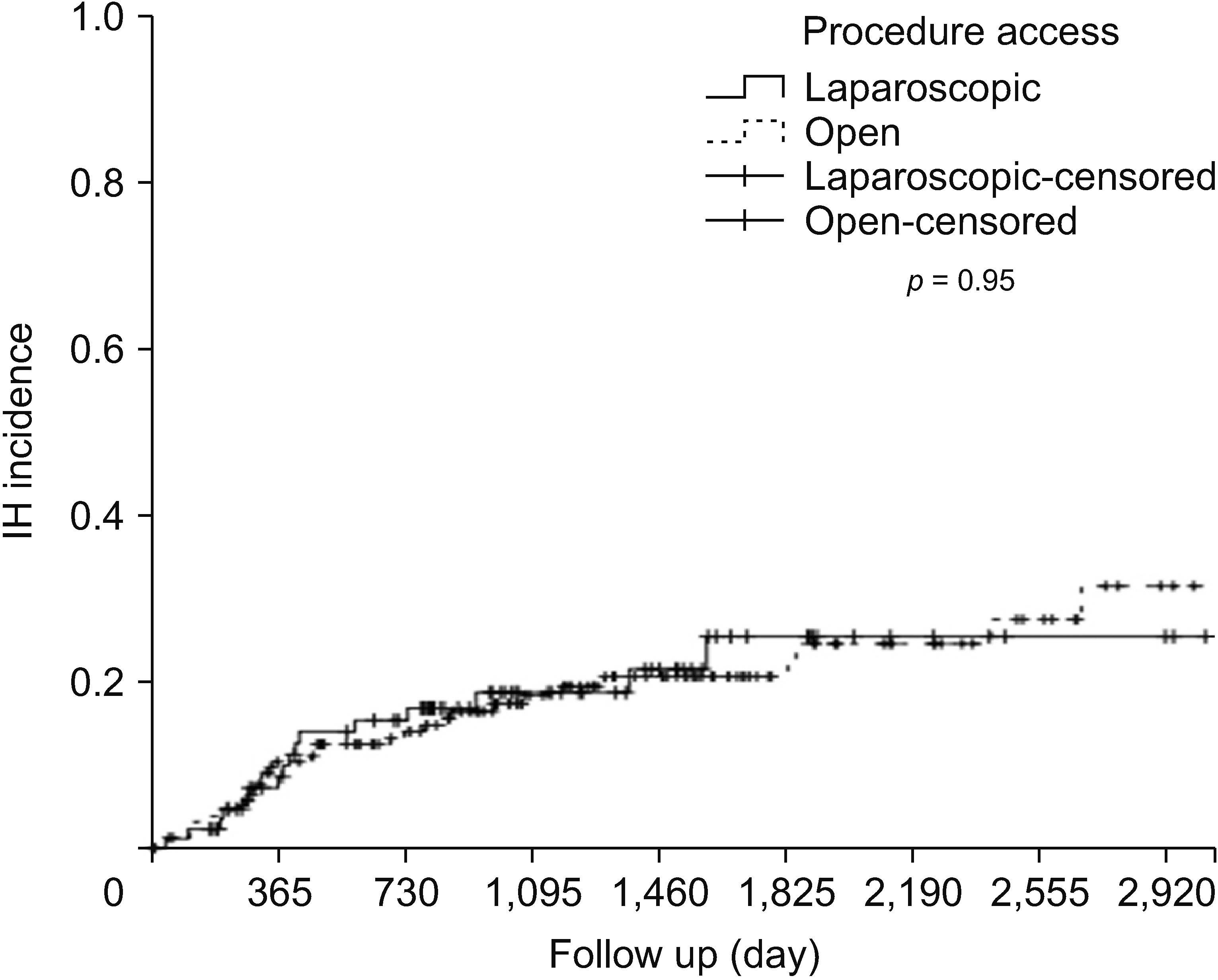
Single-center retrospective review of patients who underwent CRLM surgery between January 2011 and December 2018. IH relating to liver surgery was confirmed by computed tomography. Patients were divided into laparoscopic liver resection (LLR) and open liver resection (OLR) groups. Data collection included age, sex, presence of diabetes mellitus, steroid intake, history of previous hernia or liver resection, subcutaneous and peri-renal fat thickness, preoperative creatinine and albumin, American Society of Anesthesiologists (ASA) score, major liver resection, surgical site infection, synchronous presentation, and preoperative chemotherapy.
Results
Two hundred and forty-seven patients were included with a mean follow-up period of 41 ± 29 months (mean ± standard deviation). Eighty seven (35%) patients had LLR and 160 patients had OLR. No significant difference in the incidence of IH between LLR and OLR was found at 1 and 3 years, respectively ([10%, 19%] vs. [10%, 19%], p = 0.95). On multivariate analysis, previous hernia history (hazard ratio [HR], 2.22; 95% confidence interval [CI], 1.56–4.86) and subcutaneous fat thickness (HR, 2.22; 95% CI, 1.19–4.13) were independent risk factors. Length of hospital stay was shorter in LLR (6 ± 4 days vs. 10 ± 8 days, p < 0.001), in comparison to OLR.
Conclusions
In CRLM, no difference in the incidence of IH between LLR and OLR was found. Previous hernia and subcutaneous fat thickness were risk factors. Further studies are needed to assess modifiable risk factors to develop IH in LLR.
Keyword
Figure
Reference
-
References
1. Itatsu K, Yokoyama Y, Sugawara G, Kubota H, Tojima Y, Kurumiya Y, et al. 2014; Incidence of and risk factors for incisional hernia after abdominal surgery. Br J Surg. 101:1439–1447. DOI: 10.1002/bjs.9600. PMID: 25123379.
Article2. Chen-Xu J, Bessa-Melo R, Graça L, Costa-Maia J. 2018; Incisional hernia in hepatobiliary and pancreatic surgery: incidence and risk factors. Hernia. 23:67–79. DOI: 10.1007/s10029-018-1847-4. PMID: 30392165.
Article3. Le Huu Nho R, Mege D, Ouaïssi M, Sielezneff I, Sastre B. 2012; Incidence and prevention of ventral incisional hernia. J Visc Surg. 149:e3–14. DOI: 10.1016/j.jviscsurg.2012.05.004. PMID: 23142402.
Article4. Nilsson JH, Strandberg Holka P, Sturesson C. 2016; Incisional hernia after open resections for colorectal liver metastases - incidence and risk factors. HPB. 18:436–441. DOI: 10.1016/j.hpb.2016.02.001. PMID: 27154807. PMCID: PMC4857068.
Article5. Togo S, Nagano Y, Masumoto C, Takakura H, Matsuo K, Takeda K, et al. 2008; Outcome of and risk factors for incisional hernia after partial hepatectomy. J Gastrointest Surg. 12:1115–1120. DOI: 10.1007/s11605-008-0469-z. PMID: 18213504.
Article6. D'Angelica M, Maddineni S, Fong Y, Martin RCG, Cohen MS, Ben-Porat L, et al. 2006; Optimal abdominal incision for partial hepatectomy: increased late complications with Mercedes-type incisions compared to extended right subcostal incisions. World J Surg. 30:410–418. DOI: 10.1007/s00268-005-0183-x. PMID: 16467983.7. Cos H, Ahmed O, Garcia-Aroz S, Vachharajani N, Shenoy S, Wellen JR, et al. 2020; Incisional hernia after liver transplantation: risk factors, management strategies and long-term outcomes of a cohort study. Int J Surg. 78:149–153. DOI: 10.1016/j.ijsu.2020.04.048. PMID: 32335240.
Article8. Arslan MK, Aydin C, Topaloglu S, Calik A, Tomas K, Karabulut E. 2017; Incidence of and risk factors for incisional hernia after liver surgery performed with a J-Shaped right subcostal incision. Am Surg. 83:e49–53. DOI: 10.1177/000313481708300204. PMID: 28228191.
Article9. Bismuth H, Chiche L. 1993; Surgery of hepatic tumors. Prog Liver Dis. 11:269–285. PMID: 8272515.10. Fretland ÅA, Dagenborg VJ, Bjørnelv GMW, Kazaryan AM, Kristiansen R, Fagerland MW, et al. 2018; Laparoscopic versus open resection for colorectal liver metastases: the OSLO-COMET randomized controlled trial. Ann Surg. 267:199–207. DOI: 10.1097/SLA.0000000000002353. PMID: 28657937.11. Kuemmerli C, Fichtinger RS, Moekotte A, Aldrighetti LA, Aroori S, Besselink MGH, et al. 2022; Laparoscopic versus open resections in the posterosuperior liver segments within an enhanced recovery programme (ORANGE Segments): study protocol for a multicentre randomised controlled trial. Trials. 23:206. DOI: 10.1186/s13063-022-06112-3. PMID: 35264216. PMCID: PMC8908665.
Article12. Maurette RJ, Ejarque MG, Mihura M, Bregante M, Bogetti D, Pirchi D. 2017; Laparoscopic liver resection in metastatic colorectal cancer treatment: comparison with long-term results using the conventional approach. Ecancermedicalscience. 11:775. DOI: 10.3332/ecancer.2017.775. PMID: 29104612. PMCID: PMC5659829.13. Chiang MH, Tsai KY, Chen HA, Wang WY, Huang MT. 2021; Comparison of surgical outcomes for laparoscopic liver resection of large hepatocellular carcinomas: a retrospective observation from single-center experience. Asian J Surg. 44:1376–1382. DOI: 10.1016/j.asjsur.2021.03.027. PMID: 33888363.
Article14. Tian F, Leng S, Chen J, Cao Y, Cao L, Wang X, et al. 2023; Long-term outcomes of laparoscopic liver resection versus open liver resection for hepatocellular carcinoma: a single-center 10-year experience. Front Oncol. 13:1112380. DOI: 10.3389/fonc.2023.1112380. PMID: 36761978. PMCID: PMC9905741.
Article15. Darnis B, Mohkam K, Golse N, Vibert E, Cherqui D, Cauchy F, et al. 2021; Long-term abdominal wall benefits of the laparoscopic approach in liver left lateral sectionectomy: a multicenter comparative study. Surg Endosc. 35:5034–5042. DOI: 10.1007/s00464-020-07985-8. PMID: 32989540.
Article16. Mishra A, Keeler BD, Maxwell-Armstrong C, Simpson JA, Acheson AG. 2014; The influence of laparoscopy on incisional hernia rates: a retrospective analysis of 1057 colorectal cancer resections. Colorectal Dis. 16:815–821. DOI: 10.1111/codi.12687. PMID: 24944003.
Article17. Guilbaud T, Feretti C, Holowko W, Garbarino GM, Marchese U, Sarran A, et al. 2020; Laparoscopic major hepatectomy: do not underestimate the impact of specimen extraction site. World J Surg. 44:1223–1230. DOI: 10.1007/s00268-019-05285-4. PMID: 31748884.
Article18. Wabitsch S, Schulz P, Fröschle F, Kästner A, Fehrenbach U, Benzing C, et al. 2021; Incidence of incisional hernia after laparoscopic liver resection. Surg Endosc. 35:1108–1115. DOI: 10.1007/s00464-020-07475-x. PMID: 32124059.
Article19. Maki H, Kim BJ, Kawaguchi Y, Fernandez-Placencia R, Haddad A, Panettieri E, et al. 2023; Incidence of and risk factors for incisional hernia after hepatectomy for colorectal liver metastases. J Gastrointest Surg. 27:2388–2395. DOI: 10.1007/s11605-023-05777-8. PMID: 37537494.
Article20. Haueter R, Schütz T, Raptis DA, Clavien PA, Zuber M. 2017; Meta-analysis of single-port versus conventional laparoscopic cholecystectomy comparing body image and cosmesis. Br J Surg. 104:1141–1159. DOI: 10.1002/bjs.10574. PMID: 28569406.
Article21. Milas M, Deveđija S, Trkulja V. 2014; Single incision versus standard multiport laparoscopic cholecystectomy: up-dated systematic review and meta-analysis of randomized trials. Surgeon. 12:271–289. DOI: 10.1016/j.surge.2014.01.009. PMID: 24529791.
Article22. Sangster W, Kulaylat AN, Stewart DB, Schubart JR, Koltun WA, Messaris E. 2015; Hernia incidence following single-site vs standard laparoscopic colorectal surgery. Colorectal Dis. 17:250–256. DOI: 10.1111/codi.12797. PMID: 25307082.
Article23. Benlice C, Stocchi L, Costedio MM, Gorgun E, Kessler H. 2016; Impact of the specific extraction-site location on the risk of incisional hernia after laparoscopic colorectal resection. Dis Colon Rectum. 59:743–750. DOI: 10.1097/DCR.0000000000000632. PMID: 27384092.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Risk of incisional hernia after laparoscopic colorectal surgery: surgeon’s worries and challenges
- Risk factors of incisional hernia after laparoscopic colorectal surgery with periumbilical minilaparotomy incision: a propensity score matching analysis
- Liver Metastases in Colorectal Cancer
- Risk Factors for Incisional Hernia and Parastomal Hernia after Colorectal Surgery
- Risk factors of incisional hernia after single-incision cholecystectomy and safety of barbed suture material for wound closure