J Korean Med Sci.
2024 May;39(19):e171. 10.3346/jkms.2024.39.e171.
Epidemiology of Respiratory Viruses in Korean Children Before and After the COVID-19 Pandemic: A Prospective Study From National Surveillance System
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- 2Boston University Chobanian & Avedisian School of Medicine, Boston, MA, USA
- 3Division of Emerging Infectious Diseases, Bureau of Infectious Diseases Diagnosis Control, Korea Disease Control and Prevention Agency (KDCA), Cheongju, Korea
- 4Department of Pediatrics, Seoul National University Children’s Hospital, Seoul, Korea
- KMID: 2555915
- DOI: http://doi.org/10.3346/jkms.2024.39.e171
Abstract
- Background
The coronavirus disease 2019 (COVID-19) pandemic led to a decrease in the seasonal incidence of many respiratory viruses worldwide due to the impact of nonpharmaceutical interventions (NPIs). However, as NPI measures were relaxed, respiratory viral infections re-emerged. We aimed to characterize the epidemiology of respiratory viruses in Korean children during post-COVID-19 pandemic years compared to that before the pandemic.
Methods
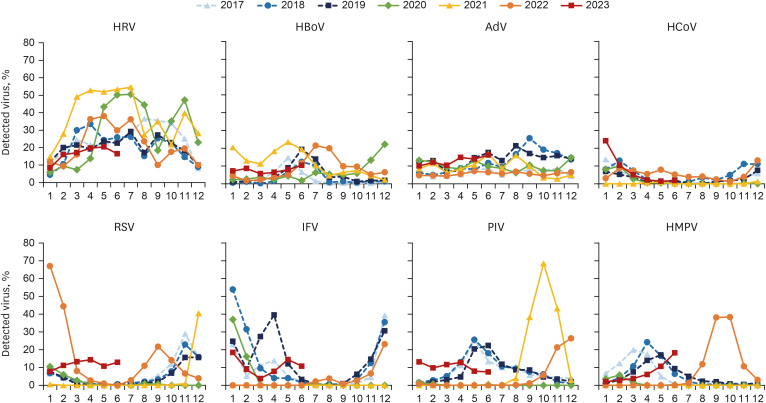
A nationwide prospective ongoing surveillance study has been conducted for detection of respiratory viruses between January 2017 and June 2023. We included data on adenovirus (AdV), human bocavirus (HBoV), human coronavirus (HCoV), human metapneumovirus (HMPV), human rhinovirus (HRV), influenza virus (IFV), parainfluenza virus (PIV), and respiratory syncytial virus (RSV), which were detected in children and adolescents younger than 20 years. We analyzed the weekly detection frequency of individual viruses and the age distribution of the affected children. The study period was divided into prepandemic (2017–2019) and postpandemic (2021–2023) periods.
Results
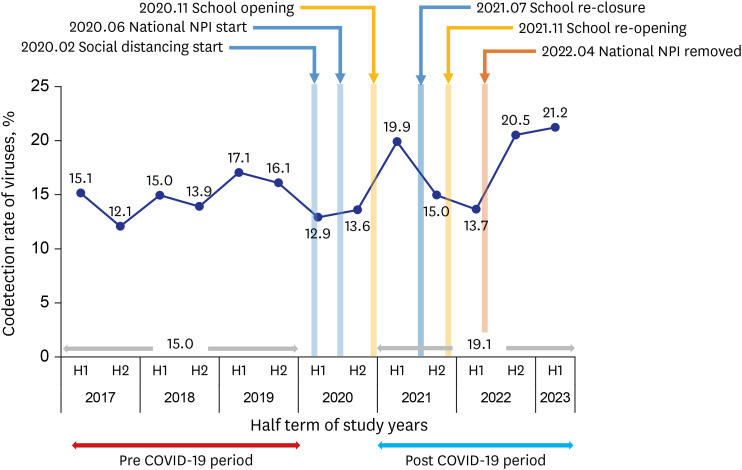
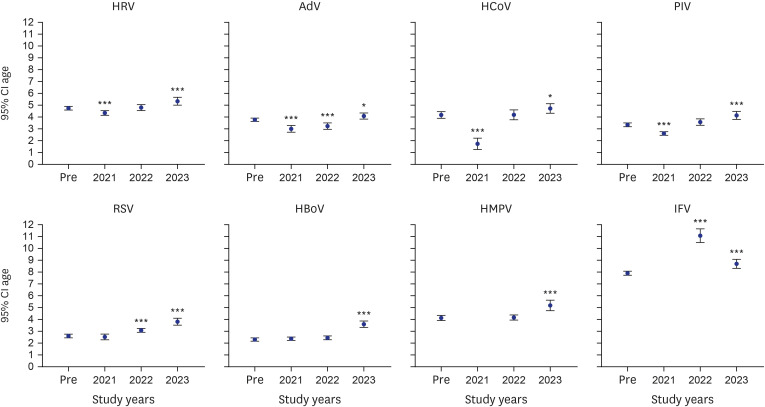
A total of 19,589 and 14,068 samples were collected in the pre- and postpandemic periods, respectively. The overall detection rate of any virus throughout the study period was 63.1%, with the lowest occurring in the 2nd half of 2020 (50.6%) and the highest occurring in the 2nd half of 2021 (72.3%). Enveloped viruses (HCoV, HMPV, IFV, PIV, and RSV) almost disappeared, but nonenveloped viruses (AdV, HBoV, and HRV) were detected even during the peak of the COVID-19 pandemic. The codetection rate increased from 15.0% prepandemic to 19.1% postpandemic (P < 0.001). During the postpandemic period, a large out-of-season PIV and HMPV epidemic occurred, but the usual seasonality began to be restored in 2023. The mean age of children with each virus detected in 2023 was significantly greater than that in prepandemic years (P = 0.003 and 0.007 for AdV and HCoV, respectively; P < 0.001 for others). The mean age of children with IFV increased in 2022 (11.1 ± 5.2 years) from prepandemic years (7.9 ± 4.6 years) but decreased to 8.7 ± 4.1 years in 2023.
Conclusion
With the relaxation of NPI measures, several seasonal respiratory viruses cocirculated with unusual seasonal epidemic patterns and were associated with increasing age of infected children.
Keyword
Figure
Reference
-
1. Miyah Y, Benjelloun M, Lairini S, Lahrichi A. COVID-19 impact on public health, environment, human psychology, global socioeconomy, and education. Sci World J. 2022; 2022:5578284.2. Huh K, Jung J, Hong J, Kim M, Ahn JG, Kim JH, et al. Impact of nonpharmaceutical interventions on the incidence of respiratory infections during the coronavirus disease 2019 (COVID-19) outbreak in Korea: a nationwide surveillance study. Clin Infect Dis. 2021; 72(7):e184–e191. PMID: 33150393.3. Ljubin-Sternak S, Meštrović T, Lukšić I, Mijač M, Vraneš J. Seasonal coronaviruses and other neglected respiratory viruses: a global perspective and a local snapshot. Front Public Health. 2021; 9:691163. PMID: 34291031.4. Shi HJ, Kim NY, Eom SA, Kim-Jeon MD, Oh SS, Moon BS, et al. Effects of non-pharmacological interventions on respiratory viruses other than SARS-CoV-2: analysis of laboratory surveillance and literature review from 2018 to 2021. J Korean Med Sci. 2022; 37(21):e172. PMID: 35638198.5. Engels G, Sack J, Weissbrich B, Hartmann K, Knies K, Härtel C, et al. Very low incidence of SARS-CoV-2, influenza and RSV but high incidence of rhino-, adeno- and endemic coronaviruses in children with acute respiratory infection in primary care pediatric practices during the second and third wave of the SARS-CoV-2 pandemic. Pediatr Infect Dis J. 2022; 41(4):e146–e148. PMID: 35175993.6. Rao S, Armistead I, Messacar K, Alden NB, Schmoll E, Austin E, et al. Shifting epidemiology and severity of respiratory syncytial virus in children during the COVID-19 pandemic. JAMA Pediatr. 2023; 177(7):730–732. PMID: 37184852.7. Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. 2023; 21(3):195–210. PMID: 36253478.8. Izu A, Nunes MC, Solomon F, Baillie V, Serafin N, Verwey C, et al. All-cause and pathogen-specific lower respiratory tract infection hospital admissions in children younger than 5 years during the COVID-19 pandemic (2020-22) compared with the pre-pandemic period (2015-19) in South Africa: an observational study. Lancet Infect Dis. 2023; 23(9):1031–1041. PMID: 37141913.9. Bardsley M, Morbey RA, Hughes HE, Beck CR, Watson CH, Zhao H, et al. Epidemiology of respiratory syncytial virus in children younger than 5 years in England during the COVID-19 pandemic, measured by laboratory, clinical, and syndromic surveillance: a retrospective observational study. Lancet Infect Dis. 2023; 23(1):56–66. PMID: 36063828.10. Kim YK, Song SH, Ahn B, Lee JK, Choi JH, Choi SH, et al. Shift in clinical epidemiology of human parainfluenza virus type 3 and respiratory syncytial virus B infections in Korean children before and during the COVID-19 pandemic: a multicenter retrospective study. J Korean Med Sci. 2022; 37(28):e215. PMID: 35851860.11. Ehrenzeller S, Chen T, Vaidya V, Rhee C, Baker MA, Klompas M. Impact of SARS-CoV-2 prevention measures on non-SARS-CoV-2 hospital-onset respiratory viral infections: an incidence trend analysis from 2015-2023. Clin Infect Dis. 2023; 77(12):1696–1699. PMID: 37531616.12. Uhteg K, Amadi A, Forman M, Mostafa HH. Circulation of non-SARS-CoV-2 respiratory pathogens and coinfection with SARS-CoV-2 amid the COVID-19 pandemic. Open Forum Infect Dis. 2021; 9(3):ofab618. PMID: 35211632.13. Kang HM, Song SH, Ahn B, Park JY, Kang H, Kwak BO, et al. Etiology and risk factors of community-acquired pneumonia in hospitalized children during the COVID-19 pandemic in South Korea. Pediatr Infect Vaccine. 2023; 30(1):20–32.14. Park S, Michelow IC, Choe YJ. Shifting patterns of respiratory virus activity following social distancing measures for coronavirus disease 2019 in South Korea. J Infect Dis. 2021; 224(11):1900–1906. PMID: 34009376.15. Kim HM, Lee EJ, Lee NJ, Woo SH, Kim JM, Rhee JE, et al. Impact of coronavirus disease 2019 on respiratory surveillance and explanation of high detection rate of human rhinovirus during the pandemic in the Republic of Korea. Influenza Other Respi Viruses. 2021; 15(6):721–731.16. Yoo KJ, Lee Y, Lee S, Friebel R, Shin SA, Lee T, et al. The road to recovery: impact of COVID-19 on healthcare utilization in South Korea in 2016-2022 using an interrupted time-series analysis. Lancet Reg Health West Pac. 2023; 41:100904. PMID: 37780633.17. Leung NH. Transmissibility and transmission of respiratory viruses. Nat Rev Microbiol. 2021; 19(8):528–545. PMID: 33753932.18. Foley DA, Yeoh DK, Minney-Smith CA, Martin AC, Mace AO, Sikazwe CT, et al. The interseasonal resurgence of respiratory syncytial virus in Australian children following the reduction of coronavirus disease 2019-related public health measures. Clin Infect Dis. 2021; 73(9):e2829–e2830. PMID: 33594407.19. Billard MN, van de Ven PM, Baraldi B, Kragten-Tabatabaie L, Bont LJ, Wildenbeest JG. International changes in respiratory syncytial virus (RSV) epidemiology during the COVID-19 pandemic: association with school closures. Influenza Other Respi Viruses. 2022; 16(5):926–936.20. Li Y, Wang X, Cong B, Deng S, Feikin DR, Nair H. Understanding the potential drivers for respiratory syncytial virus rebound during the coronavirus disease 2019 pandemic. J Infect Dis. 2022; 225(6):957–964. PMID: 35030633.21. Cohen R, Ashman M, Taha MK, Varon E, Angoulvant F, Levy C, et al. Pediatric Infectious Disease Group (GPIP) position paper on the immune debt of the COVID-19 pandemic in childhood, how can we fill the immunity gap? Infect Dis Now. 2021; 51(5):418–423. PMID: 33991720.22. Lim FJ, Wake ZV, Levy A, Tempone S, Moore HC, Richmond PC, et al. Viral etiology and the impact of codetection in young children presenting with influenza-like illness. J Pediatric Infect Dis Soc. 2017; 6(3):260–266. PMID: 27440506.23. Li Y, Pillai P, Miyake F, Nair H. The role of viral co-infections in the severity of acute respiratory infections among children infected with respiratory syncytial virus (RSV): a systematic review and meta-analysis. J Glob Health. 2020; 10(1):010426. PMID: 32566164.24. Saravanos GL, Hu N, Homaira N, Muscatello DJ, Jaffe A, Bartlett AW, et al. RSV epidemiology in Australia before and during COVID-19. Pediatrics. 2022; 149(2):e2021053537. PMID: 35083489.25. Rice E, Oakes DB, Holland C, Moore HC, Blyth CC. Respiratory syncytial virus in children: epidemiology and clinical impact post-COVID-19. Curr Opin Infect Dis. 2023; 36(6):522–528. PMID: 37830952.26. McNab S, Ha Do LA, Clifford V, Crawford NW, Daley A, Mulholland K, et al. Changing epidemiology of respiratory syncytial virus in Australia-delayed re-emergence in Victoria compared to Western Australia/New South Wales (WA/NSW) after prolonged lock-down for coronavirus disease 2019 (COVID-19). Clin Infect Dis. 2021; 73(12):2365–2366. PMID: 33735388.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Increased Trend of Adenovirus Activity After the COVID-19 Pandemic in South Korea: Analysis of National Surveillance Data
- Neglecting the neglected during the COVID-19 pandemic: the case of leptospirosis in Sri Lanka
- Changes in the pattern and disease burden of acute respiratory viral infections before and during the COVID-19 pandemic
- Age-Related Morbidity and Mortality among Patients with COVID-19
- The coronavirus disease 2019 pandemic and chronic diseases