Clin Endosc.
2024 May;57(3):402-406. 10.5946/ce.2023.268.
Polyposis of gastrointestinal tract after COVID-19 mRNA vaccination: a report of two cases
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- KMID: 2555902
- DOI: http://doi.org/10.5946/ce.2023.268
Abstract
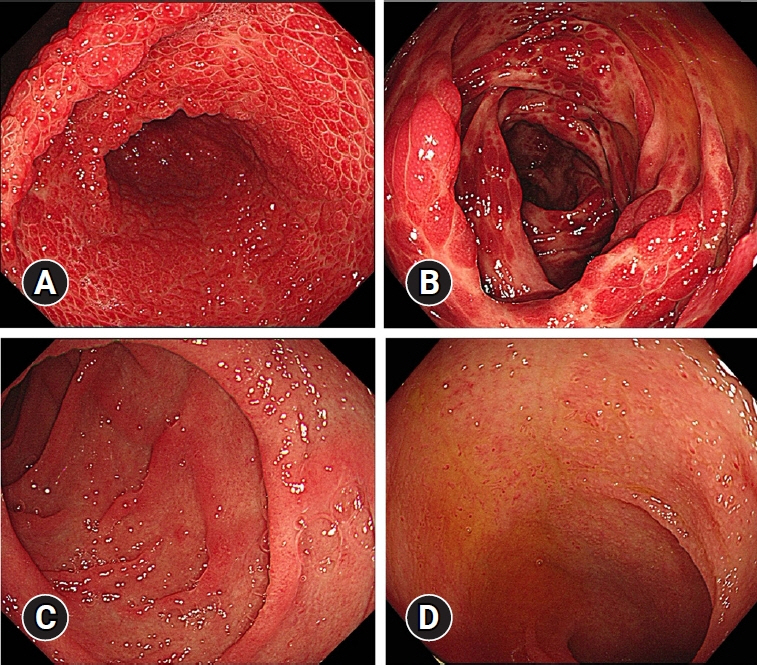
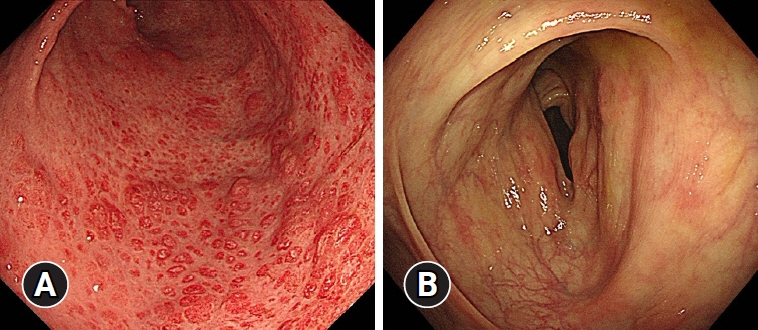
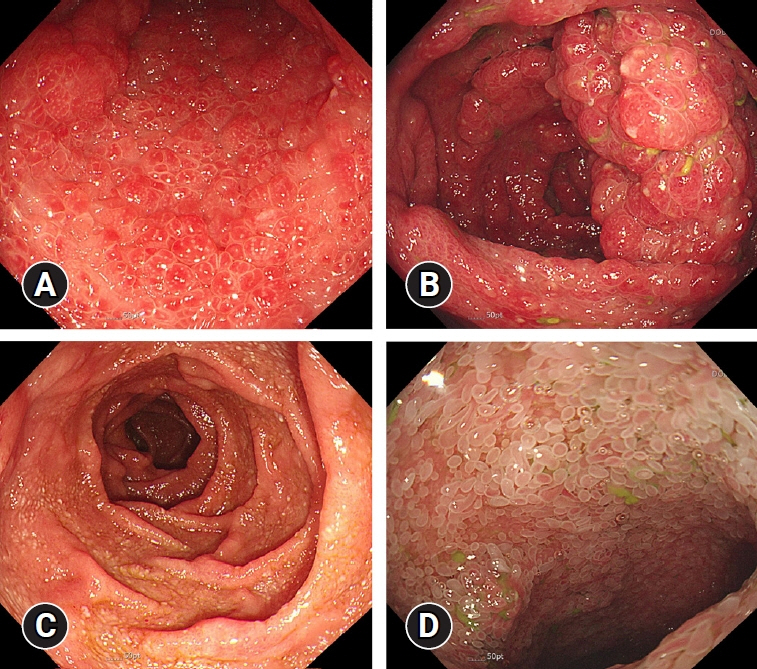
- Cronkhite-Canada syndrome is a rare gastrointestinal polyposis syndrome with distinctive clinical features and endoscopic findings. Diagnosis can be challenging without suspicion, and the disease carries high mortality due to complications such as infection, gastrointestinal bleeding, and malignancies. This paper presents two cases of Cronkhite-Canada syndrome occurring after coronavirus disease 2019 (COVID-19) mRNA vaccination. Both cases exhibited typical clinical findings, including hypogeusia, onychodystrophy, alopecia, and weight loss. Typical polyposis in the gastrointestinal tract was confirmed through endoscopies. As symptomatic treatment did not improve the symptoms, corticosteroids were administered, and symptoms and laboratory test results improved immediately. The patients improved upon corticosteroids tapering. These cases illustrate typical presentations of Cronkhite-Canada syndrome and the course of the disease following corticosteroid treatment. Additionally, they suggest the possibility that Cronkhite-Canada syndrome may be triggered by COVID-19 mRNA vaccination.
Keyword
Figure
Reference
-
1. Wu ZY, Sang LX, Chang B. Cronkhite-Canada syndrome: from clinical features to treatment. Gastroenterol Rep (Oxf). 2020; 8:333–342.
Article2. Kwon J, Fluxá-Cardenas D, Francis D. Cronkhite-Canada syndrome. Clin Gastroenterol Hepatol. 2022; 20:e1224–e1225.
Article3. Jiang CD, Myint H, Tie A, et al. Sustained clinical response to infliximab in refractory Cronkhite-Canada syndrome. BMJ Case Rep. 2020; 13:e236990.
Article4. Kopáčová M, Urban O, Cyrany J, et al. Cronkhite-Canada syndrome: review of the literature. Gastroenterol Res Pract. 2013; 2013:856873.
Article5. Sweetser S, Ahlquist DA, Osborn NK, et al. Clinicopathologic features and treatment outcomes in Cronkhite-Canada syndrome: support for autoimmunity. Dig Dis Sci. 2012; 57:496–502.
Article6. Fan RY, Wang XW, Xue LJ, et al. Cronkhite-Canada syndrome polyps infiltrated with IgG4-positive plasma cells. World J Clin Cases. 2016; 4:248–252.
Article7. Ehrenfeld M, Tincani A, Andreoli L, et al. Covid-19 and autoimmunity. Autoimmun Rev. 2020; 19:102597.
Article8. Caso F, Costa L, Ruscitti P, et al. Could Sars-coronavirus-2 trigger autoimmune and/or autoinflammatory mechanisms in genetically predisposed subjects? Autoimmun Rev. 2020; 19:102524.
Article9. Zhou Y, Han T, Chen J, et al. Clinical and autoimmune characteristics of severe and critical cases of COVID-19. Clin Transl Sci. 2020; 13:1077–1086.
Article10. Vojdani A, Kharrazian D. Potential antigenic cross-reactivity between SARS-CoV-2 and human tissue with a possible link to an increase in autoimmune diseases. Clin Immunol. 2020; 217:108480.
Article11. Sapkota P, Gurung RB, Shrestha A, et al. Cronkhite-Canada syndrome: a case report. JNMA J Nepal Med Assoc. 2022; 60:473–477.
Article12. Schonberger LB, Bregman DJ, Sullivan-Bolyai JZ, et al. Guillain-Barre syndrome following vaccination in the National Influenza Immunization Program, United States, 1976--1977. Am J Epidemiol. 1979; 110:105–123.
Article13. Miller E, Waight P, Farrington CP, et al. Idiopathic thrombocytopenic purpura and MMR vaccine. Arch Dis Child. 2001; 84:227–229.14. Wraith DC, Goldman M, Lambert PH. Vaccination and autoimmune disease: what is the evidence? Lancet. 2003; 362:1659–1666.
Article15. Segal Y, Shoenfeld Y. Vaccine-induced autoimmunity: the role of molecular mimicry and immune crossreaction. Cell Mol Immunol. 2018; 15:586–594.
Article16. Chen Y, Xu Z, Wang P, et al. New-onset autoimmune phenomena post-COVID-19 vaccination. Immunology. 2022; 165:386–401.
Article17. Miyawaki K, Komori T, Ishida Y, et al. Cronkhite-Canada syndrome mimicking COVID-19-related symptoms. Acta Derm Venereol. 2022; 102:adv00812.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Adult-Onset Type 1 Diabetes Development Following COVID-19 mRNA Vaccination
- Cases of Pernio-Like Lesions after mRNA-1273 Vaccination with Clinical and Pathological Features: A Single-Center Experience
- Ipsilateral Radial Neuropathy after COVID-19 mRNA Vaccination in an Immunocompetent Young Man
- COVID-19 Vaccination in Korea
- Eosinophilic Granulomatosis With Polyangiitis Following COVID-19 Vaccination: A Case Report