Clin Endosc.
2024 May;57(3):342-349. 10.5946/ce.2023.130.
Clinical outcomes of nonvariceal upper gastrointestinal bleeding in nonagenarians and octogenarians: a comparative nationwide analysis
- Affiliations
-
- 1Department of Internal Medicine, SBH Health System, New York, NY
- 2Department of Medicine, University of Illinois at Chicago, Chicago, IL, USA
- 3Tanta University Faculty of Medicine, Tanta, Egypt
- 4Department of Internal Medicine, University of Missouri-Kansas City School of Medicine, Kansas City, MO
- 5Division of Gastroenterology, SBH Health System, New York, NY
- 6Division of Gastroenterology, Montefiore Medical Center, Albert Einstein College of Medicine, Bronx, NY
- 7Division of Gastroenterology, Department of Medicine, Robert Wood Johnson University Hospital, New Brunswick, NJ, USA
- KMID: 2555896
- DOI: http://doi.org/10.5946/ce.2023.130
Abstract
- Background/Aims
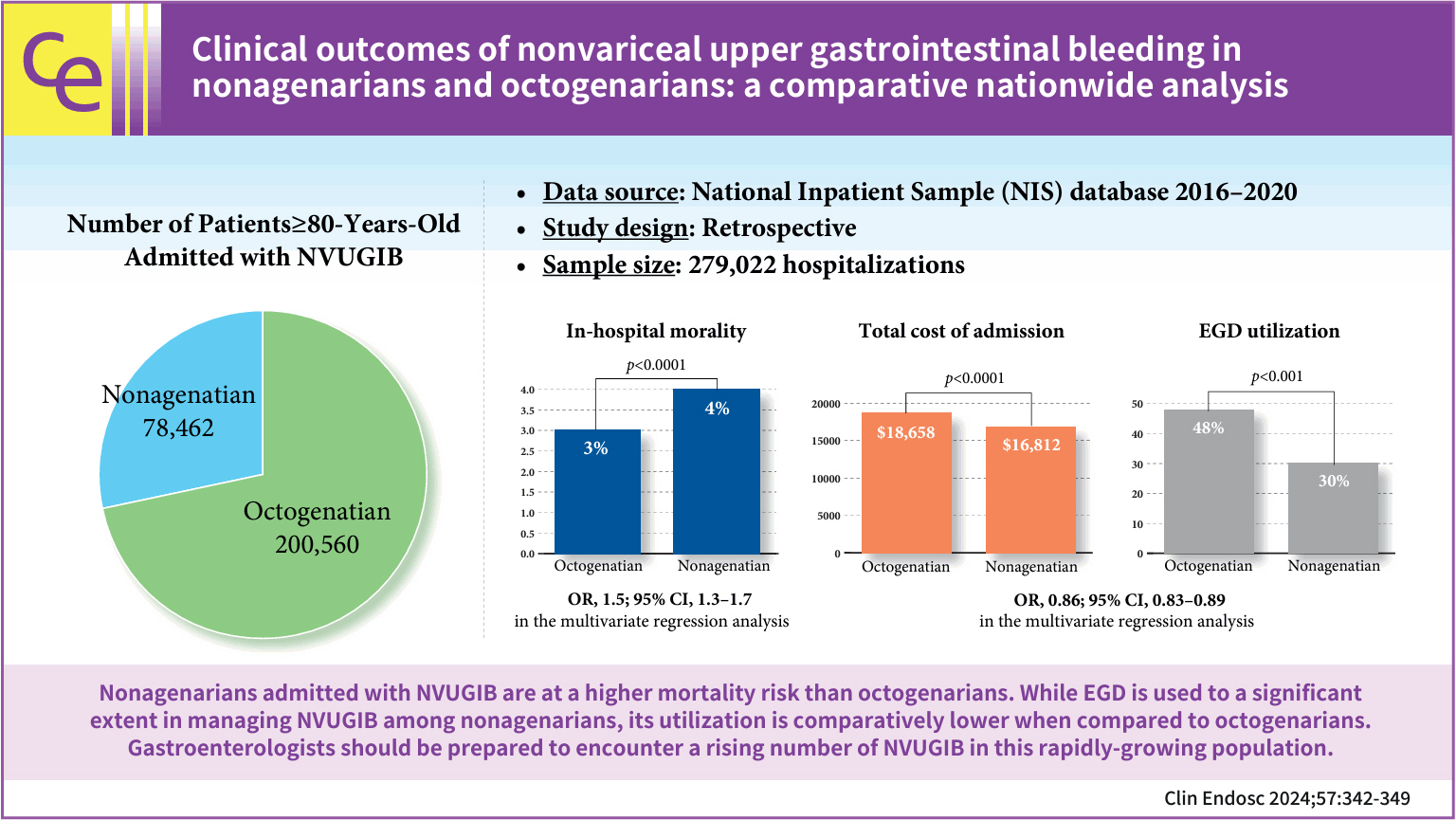
Nonagenarians will purportedly account for 10% of the United States population by 2050. However, no studies have assessed the outcomes of nonvariceal upper gastrointestinal bleeding (NVUGIB) in this age group.
Methods
The National Inpatient Sample database between 2016 and 2020 was used to compare the clinical outcomes of NVUGIB in nonagenarians and octogenarians and evaluate predictors of mortality and the use of esophagogastroduodenoscopy (EGD).
Results
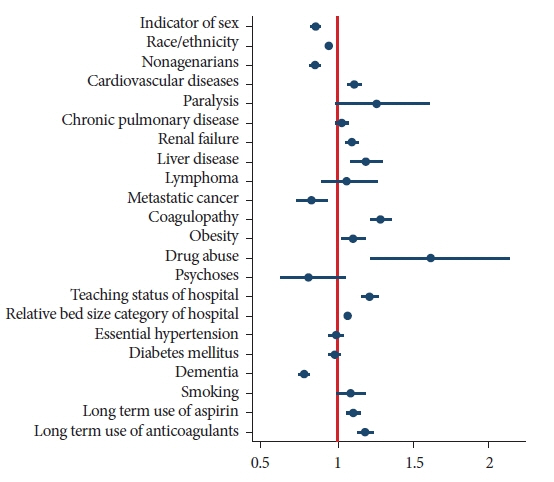
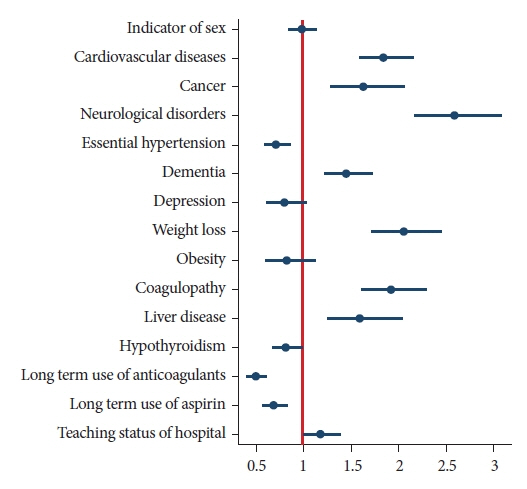
Nonagenarians had higher in-hospital mortality than that of octogenarians (4% vs. 3%, p<0.001). EGD utilization (30% vs. 48%, p<0.001) and blood transfusion (27% vs. 40%, p<0.001) was significantly lower in nonagenarians. Multivariate logistic regression analysis revealed that nonagenarians with NVUGIB had higher odds of mortality (odds ratio [OR], 1.5; 95% confidence interval [CI], 1.3–1.7) and lower odds of EGD utilization (OR, 0.86; 95% CI, 0.83–0.89) than those of octogenarians.
Conclusions
Nonagenarians admitted with NVUGIB have a higher mortality risk than that of octogenarians. EGD is used significantly in managing NVUGIB among nonagenarians; however, its utilization is comparatively lower than in octogenarians. More studies are needed to assess predictors of poor outcomes and the indications of EGD in this growing population.
Keyword
Figure
Reference
-
1. Abougergi MS, Travis AC, Saltzman JR. The in-hospital mortality rate for upper GI hemorrhage has decreased over 2 decades in the United States: a nationwide analysis. Gastrointest Endosc. 2015; 81:882–888.
Article2. Antunes C, Copelin II EL. Upper gastrointestinal bleeding. StatPearls [Internet]. StatPearls Publishing;2023. [updated 2023 Apr 7; cited 2023 Apr 27]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470300/.3. Jairath V, Martel M, Logan RF, et al. Why do mortality rates for nonvariceal upper gastrointestinal bleeding differ around the world?: a systematic review of cohort studies. Can J Gastroenterol. 2012; 26:537–543.
Article4. Chason R, Singal A, Rockey D. Mortality in acute upper gastrointestinal bleeding is uncommonly due to persistent hemorrhage: 1634. Am J Gastroenterol. 2013; 108:S490–S491.5. Biecker E. Diagnosis and therapy of non-variceal upper gastrointestinal bleeding. World J Gastrointest Pharmacol Ther. 2015; 6:172–182.
Article6. Alkhatib AA, Elkhatib FA, Alkhatib AA, et al. Acute upper gastrointestinal bleeding in elderly people: presentations, endoscopic findings, and outcomes. J Am Geriatr Soc. 2010; 58:182–185.
Article7. Theocharis GJ, Arvaniti V, Assimakopoulos SF, et al. Acute upper gastrointestinal bleeding in octogenarians: clinical outcome and factors related to mortality. World J Gastroenterol. 2008; 14:4047–4053.
Article8. Rural Health Information Hub (RHIhub). Rural aging in place toolkit: demographic changes and aging population [Internet]. RHIhub;2015 [cited 2023 Apr 27]. Available from: https://www.ruralhealthinfo.org/toolkits/aging/1/demographics.9. Odden MC, Koh WJ, Arnold AM, et al. Trajectories of nonagenarian health: sex, age, and period effects. Am J Epidemiol. 2019; 188:382–388.
Article10. Healthcare Cost and Utilization Project (HCUP). Elixhauser comorbidity software refined for ICD-10-CM [Internet]. HCUP;2022 [cited 2023 Jul 1]. Available from: https://hcup-us.ahrq.gov/toolssoftware/comorbidityicd10/comorbidity_icd10.jsp.11. Glasheen WP, Cordier T, Gumpina R, et al. Charlson Comorbidity Index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits. 2019; 12:188–197.12. Di Fiore F, Lecleire S, Merle V, et al. Changes in characteristics and outcome of acute upper gastrointestinal haemorrhage: a comparison of epidemiology and practices between 1996 and 2000 in a multicentre French study. Eur J Gastroenterol Hepatol. 2005; 17:641–647.
Article13. van Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003; 98:1494–1499.14. Diener HC. Preventing major gastrointestinal bleeding in elderly patients. Lancet. 2017; 390:435–437.
Article15. Yamaguchi Y, Yamato T, Katsumi N, et al. Endoscopic hemostasis: safe treatment for peptic ulcer patients aged 80 years or older? J Gastroenterol Hepatol. 2003; 18:521–525.
Article16. Choudari CP, Elton RA, Palmer KR. Age-related mortality in patients treated endoscopically for bleeding peptic ulcer. Gastrointest Endosc. 1995; 41:557–560.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Safe and feasible outcomes of cholecystectomy in extremely elderly patients (octogenarians vs. nonagenarians)
- Endoscopic Management of Nonvariceal Upper Gastrointestinal Bleeding
- Endoscopy Timing in Patients with Acute Upper Gastrointestinal Bleeding
- Recent Update of Embolization of Upper Gastrointestinal Tract Bleeding
- Transcatheter Arterial Embolization of Nonvariceal Upper Gastrointestinal Bleeding with N-Butyl Cyanoacrylate