Clin Endosc.
2024 May;57(3):335-341. 10.5946/ce.2023.018.
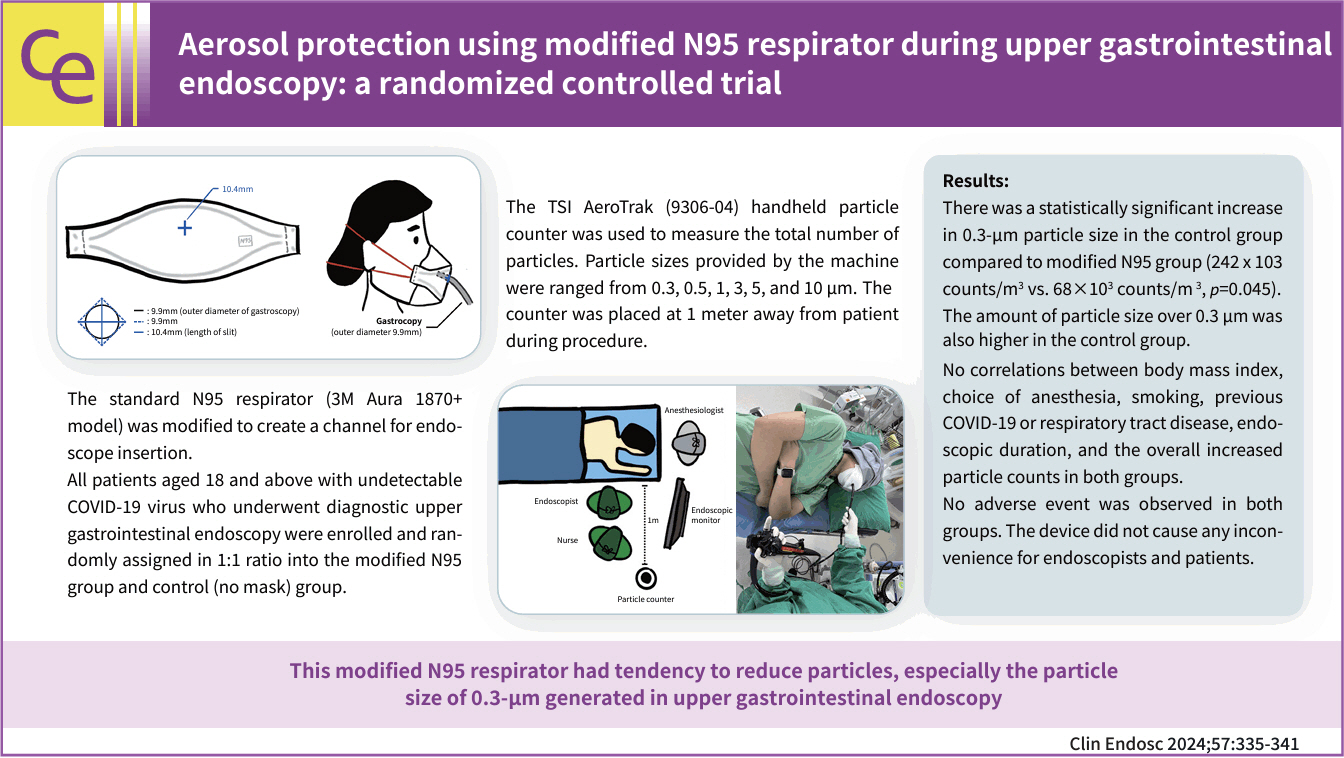
Aerosol protection using modified N95 respirator during upper gastrointestinal endoscopy: a randomized controlled trial
- Affiliations
-
- 1Department of Surgery, Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand
- KMID: 2555895
- DOI: http://doi.org/10.5946/ce.2023.018
Abstract
- Background/Aims
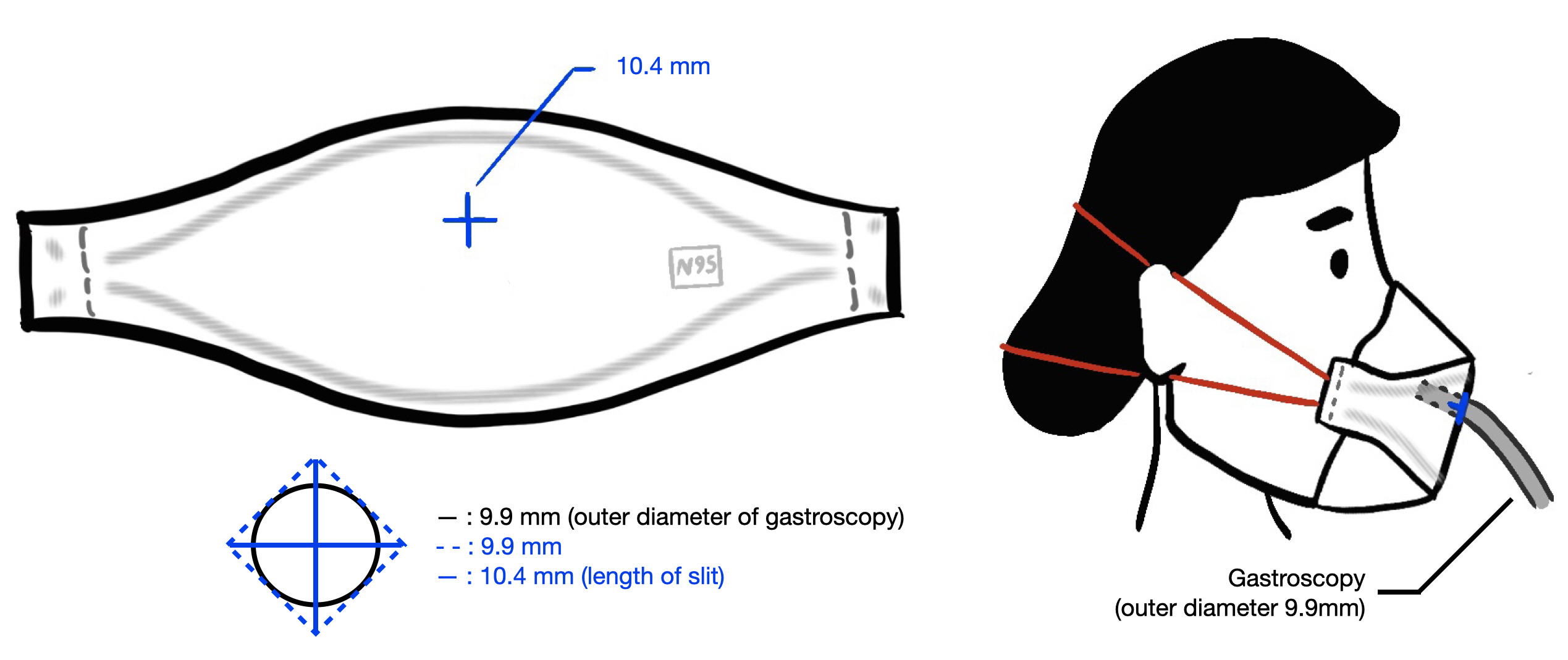
The coronavirus disease 2019 pandemic has affected the worldwide practice of upper gastrointestinal endoscopy. Here we designed a modified N95 respirator with a channel for endoscope insertion and evaluated its efficacy in upper gastrointestinal endoscopy.
Methods
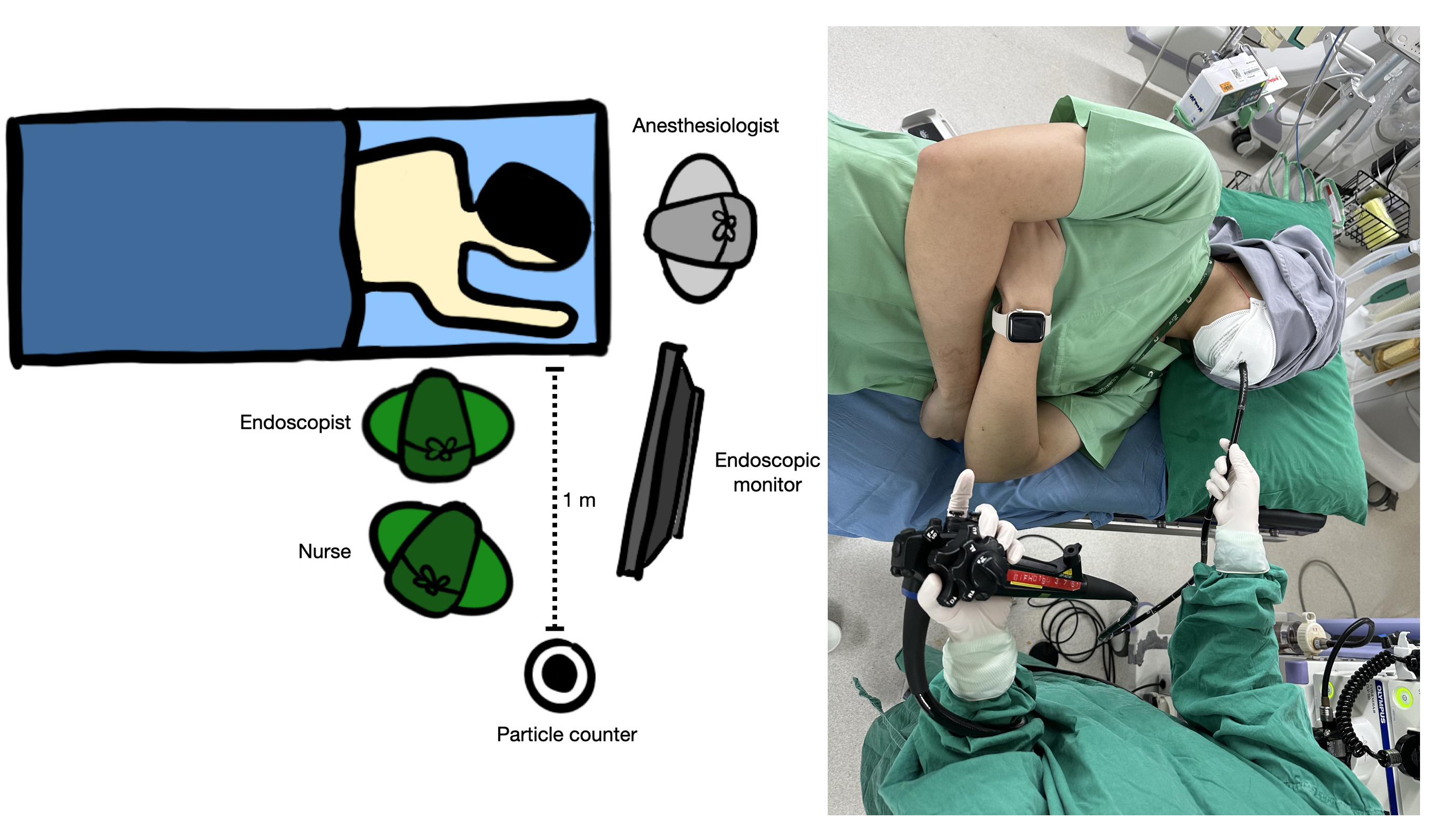
Thirty patients scheduled for upper gastrointestinal endoscopy were randomized into the modified N95 (n=15) or control (n=15) group. The mask was placed on the patient after anesthesia administration and particles were counted every minute before (baseline) and during the procedure by a TSI AeroTrak particle counter (9306-04; TSI Inc.) and categorized by size (0.3, 0.5, 1, 3, 5, and 10 µm). Differences in particle counts between time points were recorded.
Results
During the procedure, the modified N95 group displayed significantly smaller overall particle sizes than the control group (median [interquartile range], 231 [54–385] vs. 579 [213–1,379]×103/m3; p=0.056). However, the intervention group had a significant decrease in 0.3-µm particles (68 [–25–185] vs. 242 [72–588]×103/m3; p=0.045). No adverse events occurred in either group. The device did not cause any inconvenience to the endoscopists or patients.
Conclusions
This modified N95 respirator reduced the number of particles, especially 0.3-µm particles, generated during upper gastrointestinal endoscopy.
Keyword
Figure
Reference
-
1. Tran K, Cimon K, Severn M, et al. Aerosol generating procedures and risk of transmission of acute respiratory infections to healthcare workers: a systematic review. PLoS One. 2012; 7:e35797.2. Klompas M, Baker M, Rhee C. What is an aerosol-generating procedure? JAMA Surg. 2021; 156:113–114.3. Rana SS. Risk of COVID-19 transmission during gastrointestinal endoscopy. J Dig Endosc. 2020; 11:27–30.
Article4. Kutti-Sridharan G, Vegunta R, Vegunta R, et al. SARS-CoV2 in different body fluids, risks of transmission, and preventing COVID-19: a comprehensive evidence-based review. Int J Prev Med. 2020; 11:97.
Article5. Peng L, Liu J, Xu W, et al. SARS-CoV-2 can be detected in urine, blood, anal swabs, and oropharyngeal swabs specimens. J Med Virol. 2020; 92:1676–1680.6. Sagami R, Nishikiori H, Sato T, et al. Aerosols produced by upper gastrointestinal endoscopy: a quantitative evaluation. Am J Gastroenterol. 2021; 116:202–205.
Article7. Gralnek IM, Hassan C, Beilenhoff U, et al. ESGE and ESGENA position statement on gastrointestinal endoscopy and the COVID-19 pandemic. Endoscopy. 2020; 52:483–490.
Article8. South African Gastroenterology Society (SAGES). SAGES position statement on endoscopy and PPE requirements during COVID-19 pandemic [Internet]. SAGES;2020. [cited 2022 Jul 1]. Available from: https://www.sages.co.za/newsletter_SAGES/PPE_Requirements.pdf.9. Kongkam P, Tiankanon K, Ratanalert S, et al. The practice of endoscopy during the COVID-19 pandemic: recommendations from the Thai Association for Gastrointestinal Endoscopy (TAGE) in collaboration with the Endoscopy Nurse Society (Thailand). Siriraj Med J. 2020; 72:283–286.
Article10. Kitiyakara T, Kamalaporn P, Poolsombat A, et al. Leak-testing of an endoscopic aerosol box for preventing SARS-CoV-2 infection during upper gastrointestinal endoscopy. Siriraj Med J. 2021; 73:702–709.
Article11. Sabbagh L, Huertas M, Preciado J, et al. New protection barrier for endoscopic procedures in the era of pandemic COVID-19. VideoGIE. 2020; 5:614–617.
Article12. Lazaridis N, Skamnelos A, Murino A, et al. "Double-surgical-mask-with-slit" method: reducing exposure to aerosol generation at upper gastrointestinal endoscopy during the COVID-19 pandemic. Endoscopy. 2020; 52:928–929.
Article13. Fujifilm. Fujifilm launches droplet-shielding Mouthpiece “B1” and Endoscope Cover “P1” [Internet]. Fujifilm;2020. [cited 2022 Jan 22]. Available from: https://www.fujifilm.com/jp/en/news/hq/5477.14. Kikuchi D, Ariyoshi D, Suzuki Y, et al. Possibility of new shielding device for upper gastrointestinal endoscopy. Endosc Int Open. 2021; 9:E1536–E1541.
Article15. Gao Y, Xie J, Ye LS, et al. Negative-pressure isolation mask for endoscopic examination during the coronavirus disease 2019 pandemic: a randomized controlled trial. Clin Transl Gastroenterol. 2021; 12:e00314.
Article16. Lai HY. Aerosol box 2020 [Internet]. 2020. [cited 2022 Jun 15]. Available from: https://sites.google.com/view/aerosolbox/home?authuser=0.17. Bar-On YM, Flamholz A, Phillips R, et al. SARS-CoV-2 (COVID-19) by the numbers. Elife. 2020; 9:e57309.
Article18. American Society of Anesthesiologists. Continuum of depth of sedation: definition of general anesthesia and levels of sedation/analgesia [Internet]. American Society of Anesthesiologists;2019. [cited 2021 Dec 25]. Available from: https://www.asahq.org/standards-and-guidelines/continuum-of-depth-of-sedation-definition-of-general-anesthesia-and-levels-of-sedationanalgesia.19. Sagami R, Nishikiori H, Sato T, et al. Endoscopic shield: barrier enclosure during the endoscopy to prevent aerosol droplets during the COVID-19 pandemic. VideoGIE. 2020; 5:445–448.
Article20. Chan SM, Ma TW, Chong MK, et al. A proof of concept study: esophagogastroduodenoscopy is an aerosol-generating procedure and continuous oral suction during the procedure reduces the amount of aerosol generated. Gastroenterology. 2020; 159:1949–1951.e4.
Article21. Nampoolsuksan C, Chinswangwatanakul V, Methasate A, et al. Management of aerosol generation during upper gastrointestinal endoscopy. Clin Endosc. 2022; 55:588–593.
Article22. Phillips F, Crowley J, Warburton S, et al. Aerosol and droplet generation in upper and lower GI endoscopy: whole procedure and event-based analysis. Gastrointest Endosc. 2022; 96:603–611.
Article23. Gregson FK, Shrimpton AJ, Hamilton F, et al. Identification of the source events for aerosol generation during oesophago-gastro-duodenoscopy. Gut. 2022; 71:871–878.
Article24. Taweerutchana V, Suwatthanarak T, Methasate A, et al. Laparoscopic surgery produced less surgical smoke and contamination comparing with open surgery: the pilot study in fresh cadaveric experiment in COVID-19 pandemic. BMC Surg. 2021; 21:422.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Evaluation of a New Workplace Protection Factor–Measuring Method for Filtering Facepiece Respirator
- Fit Test for N95 Filtering Facepiece Respirators and KF94 Masks for Healthcare Workers: a Prospective Single-center Simulation Study
- Water-blocking Asphyxia of N95 Medical Respirator During Hot Environment Work Tasks With Whole-body Enclosed Anti-bioaerosol Suit
- Particle Filtration Efficiency Testing of Sterilization Wrap Masks
- Management of aerosol generation during upper gastrointestinal endoscopy