Diabetes Metab J.
2024 May;48(3):373-384. 10.4093/dmj.2023.0190.
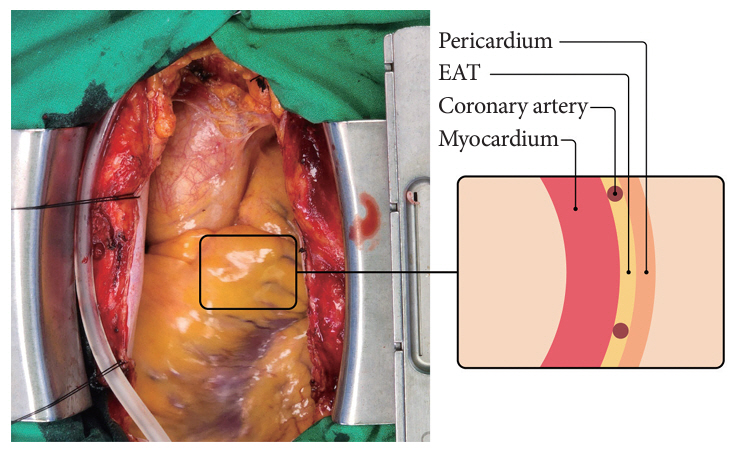
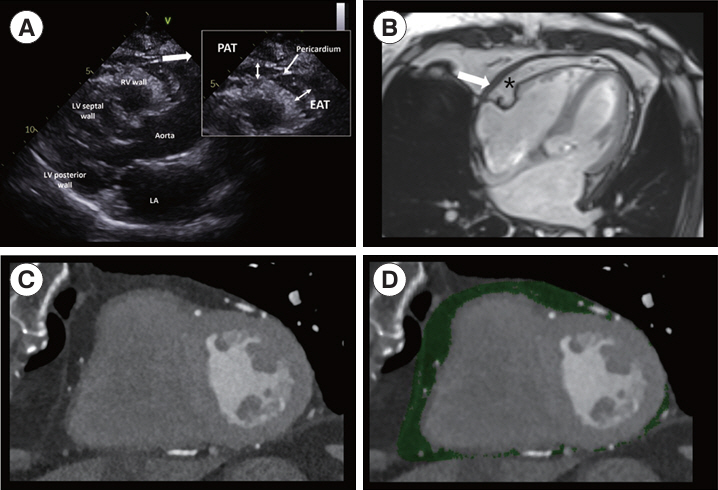
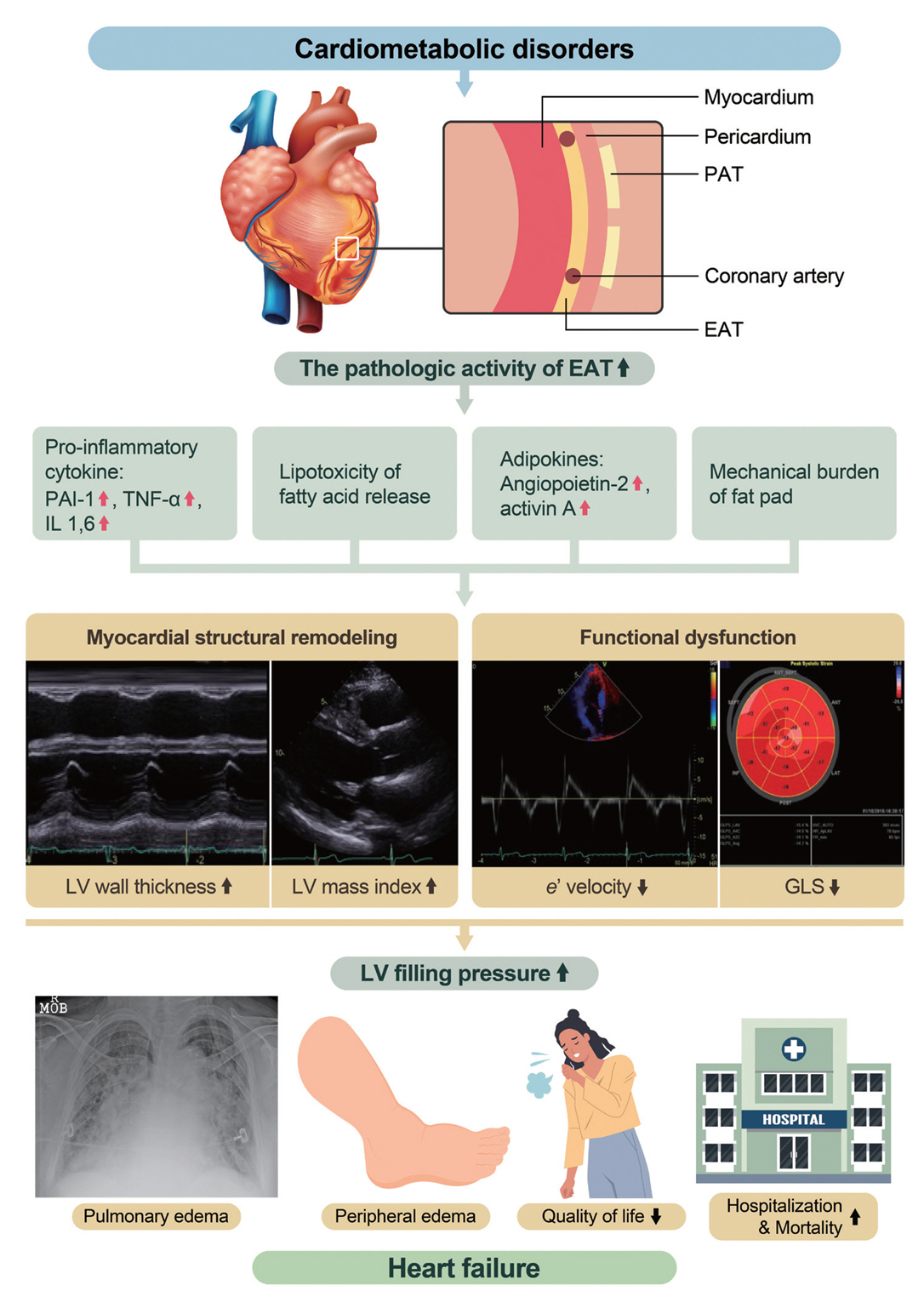
Epicardial Adipose Tissue and Heart Failure, Friend or Foe?
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- KMID: 2555768
- DOI: http://doi.org/10.4093/dmj.2023.0190
Abstract
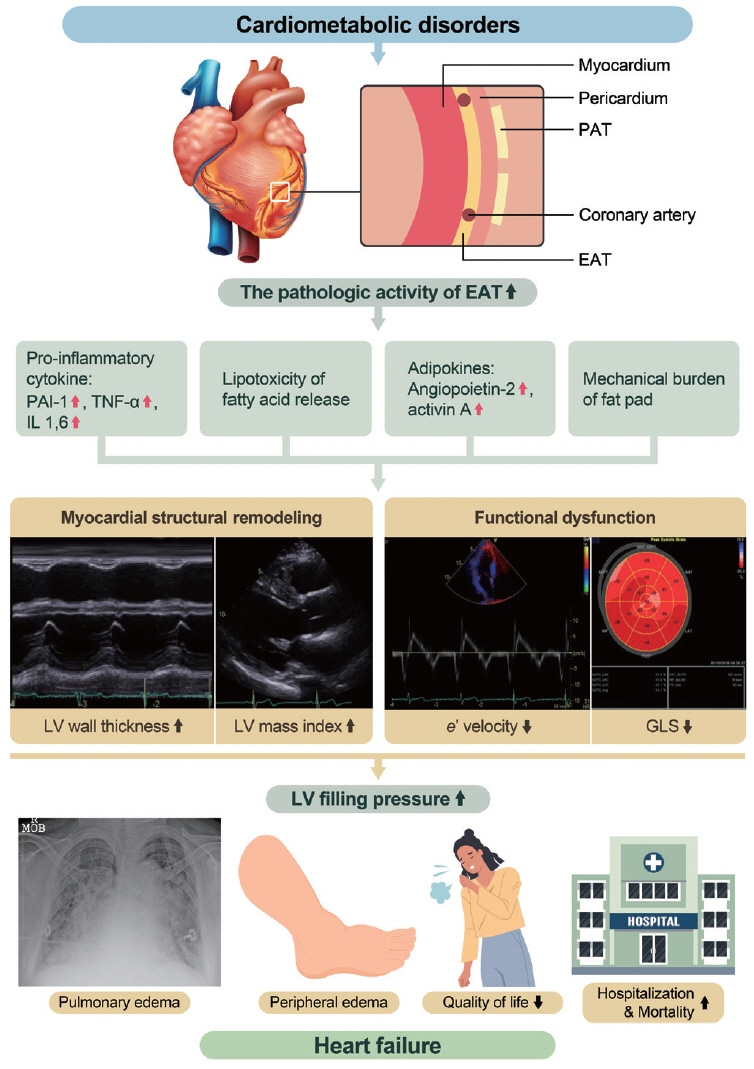
- Heart failure (HF) management guidelines recommend individualized assessments based on HF phenotypes. Adiposity is a known risk factor for HF. Recently, there has been an increased interest in organ-specific adiposity, specifically the role of the epicardial adipose tissue (EAT), in HF risk. EAT is easily assessable through various imaging modalities and is anatomically and functionally connected to the myocardium. In pathological conditions, EAT secretes inflammatory cytokines, releases excessive fatty acids, and increases mechanical load on the myocardium, resulting in myocardial remodeling. EAT plays a pathophysiological role in characterizing both HF with reduced ejection fraction (HFrEF) and HF with preserved ejection fraction (HFpEF). In HFrEF, EAT volume is reduced, reflecting an impaired metabolic reservoir, whereas in HFpEF, the amount of EAT is associated with worse biomarker and hemodynamic profiles, indicating increased EAT activity. Studies have examined the possibility of therapeutically targeting EAT, and recent studies using sodium glucose cotransporter 2 inhibitors have shown potential in reducing EAT volume. However, further research is required to determine the clinical implications of reducing EAT activity in patients with HF.
Figure
Cited by 1 articles
-
Targeting Cardiac Fibrosis in Diabetic Heart Failure: The Role of the EZH2, AMPK, and PPAR-γ Pathways (
Diabetes Metab J 2024;48:716-29)
Jooyeop Lee, Joon Ho Moon
Diabetes Metab J. 2024;48(6):1176-1178. doi: 10.4093/dmj.2024.0551.
Reference
-
1. Cho DH, Joo HJ, Kim MN, Lim DS, Shim WJ, Park SM. Association between epicardial adipose tissue, high-sensitivity C-reactive protein and myocardial dysfunction in middle-aged men with suspected metabolic syndrome. Cardiovasc Diabetol. 2018; 17:95.
Article2. Iacobellis G, Corradi D, Sharma AM. Epicardial adipose tissue: anatomic, biomolecular and clinical relationships with the heart. Nat Clin Pract Cardiovasc Med. 2005; 2:536–43.
Article3. Sacks HS, Fain JN. Human epicardial adipose tissue: a review. Am Heart J. 2007; 153:907–17.
Article4. Iacobellis G, Willens HJ. Echocardiographic epicardial fat: a review of research and clinical applications. J Am Soc Echocardiogr. 2009; 22:1311–9.
Article5. Iacobellis G. Epicardial and pericardial fat: close, but very different. Obesity (Silver Spring). 2009; 17:625.
Article6. Fei J, Cook C, Blough E, Santanam N. Age and sex mediated changes in epicardial fat adipokines. Atherosclerosis. 2010; 212:488–94.
Article7. Iacobellis G. Epicardial adipose tissue in contemporary cardiology. Nat Rev Cardiol. 2022; 19:593–606.
Article8. Song Y, Song F, Wu C, Hong YX, Li G. The roles of epicardial adipose tissue in heart failure. Heart Fail Rev. 2022; 27:369–77.
Article9. Park JJ, Lee CJ, Park SJ, Choi JO, Choi S, Park SM, et al. Heart failure statistics in Korea, 2020: a report from the Korean Society of Heart Failure. Int J Heart Fail. 2021; 3:224–36.
Article10. Lee HY, Oh BH. Paradigm shifts of heart failure therapy: do we need another paradigm? Int J Heart Fail. 2020; 2:145–56.
Article11. Lee KS, Noh J, Park SM, Choi KM, Kang SM, Won KC, et al. Evaluation and management of patients with diabetes and heart failure: a Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement. Diabetes Metab J. 2023; 47:10–26.
Article12. Cho DH, Yoo BS. Current prevalence, incidence, and outcomes of heart failure with preserved ejection fraction. Heart Fail Clin. 2021; 17:315–26.
Article13. Cho JY, Cho DH, Youn JC, Kim D, Park SM, Jung MH, et al. Korean Society of Heart Failure guidelines for the management of heart failure: definition and diagnosis. Int J Heart Fail. 2023; 5:51–65.
Article14. Kim KJ, Cho HJ, Kim MS, Kang J, Kim KH, Kim D, et al. Focused update of 2016 Korean Society of Heart Failure guidelines for the management of chronic heart failure. Int J Heart Fail. 2019; 1:4–24.
Article15. McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Bohm M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42:3599–726.
Article16. Youn JC, Kim D, Cho JY, Cho DH, Park SM, Jung MH, et al. Korean Society of Heart Failure guidelines for the management of heart failure: treatment. Int J Heart Fail. 2023; 5:66–81.
Article17. Cho DH, Kim MN, Joo HJ, Shim WJ, Lim DS, Park SM. Visceral obesity, but not central obesity, is associated with cardiac remodeling in subjects with suspected metabolic syndrome. Nutr Metab Cardiovasc Dis. 2019; 29:360–6.
Article18. Iacobellis G, Ribaudo MC, Assael F, Vecci E, Tiberti C, Zappaterreno A, et al. Echocardiographic epicardial adipose tissue is related to anthropometric and clinical parameters of metabolic syndrome: a new indicator of cardiovascular risk. J Clin Endocrinol Metab. 2003; 88:5163–8.
Article19. Iacobellis G, Barbaro G, Gerstein HC. Relationship of epicardial fat thickness and fasting glucose. Int J Cardiol. 2008; 128:424–6.
Article20. Malavazos AE, Ermetici F, Cereda E, Coman C, Locati M, Morricone L, et al. Epicardial fat thickness: relationship with plasma visfatin and plasminogen activator inhibitor-1 levels in visceral obesity. Nutr Metab Cardiovasc Dis. 2008; 18:523–30.
Article21. Pierdomenico SD, Pierdomenico AM, Cuccurullo F, Iacobellis G. Meta-analysis of the relation of echocardiographic epicardial adipose tissue thickness and the metabolic syndrome. Am J Cardiol. 2013; 111:73–8.
Article22. Fernandes-Cardoso A, Santos-Furtado M, Grindler J, Ferreira LA, Andrade JL, Santo MA. Epicardial fat thickness correlates with P-wave duration, left atrial size and decreased left ventricular systolic function in morbid obesity. Nutr Metab Cardiovasc Dis. 2017; 27:731–8.
Article23. Cetin M, Kocaman SA, Durakoglugil ME, Erdogan T, Ergul E, Dogan S, et al. Effect of epicardial adipose tissue on diastolic functions and left atrial dimension in untreated hypertensive patients with normal systolic function. J Cardiol. 2013; 61:359–64.
Article24. Yerramasu A, Dey D, Venuraju S, Anand DV, Atwal S, Corder R, et al. Increased volume of epicardial fat is an independent risk factor for accelerated progression of sub-clinical coronary atherosclerosis. Atherosclerosis. 2012; 220:223–30.
Article25. Shin SY, Yong HS, Lim HE, Na JO, Choi CU, Choi JI, et al. Total and interatrial epicardial adipose tissues are independently associated with left atrial remodeling in patients with atrial fibrillation. J Cardiovasc Electrophysiol. 2011; 22:647–55.
Article26. McNeill AM, Rosamond WD, Girman CJ, Golden SH, Schmidt MI, East HE, et al. The metabolic syndrome and 11-year risk of incident cardiovascular disease in the atherosclerosis risk in communities study. Diabetes Care. 2005; 28:385–90.
Article27. Hwang IC, Choi HM, Yoon YE, Park JJ, Park JB, Park JH, et al. Body mass index, muscle mass, and all-cause mortality in patients with acute heart failure: the obesity paradox revisited. Int J Heart Fail. 2022; 4:95–109.
Article28. Kim SE, Lee CJ. The paradox in defining obesity in patients with heart failure. Int J Heart Fail. 2022; 4:91–4.
Article29. Ho JE, McCabe EL, Wang TJ, Larson MG, Levy D, Tsao C, et al. Cardiometabolic traits and systolic mechanics in the community. Circ Heart Fail. 2017; 10:e003536.
Article30. Shen Q, Hiebert JB, Rahman FK, Krueger KJ, Gupta B, Pierce JD. Understanding obesity-related high output heart failure and its implications. Int J Heart Fail. 2021; 3:160–71.
Article31. Lemieux I, Pascot A, Prud’homme D, Almeras N, Bogaty P, Nadeau A, et al. Elevated C-reactive protein: another component of the atherothrombotic profile of abdominal obesity. Arterioscler Thromb Vasc Biol. 2001; 21:961–7.32. Park M, Sweeney G. Direct effects of adipokines on the heart: focus on adiponectin. Heart Fail Rev. 2013; 18:631–44.
Article33. Lopaschuk GD. Metabolic modulators in heart disease: past, present, and future. Can J Cardiol. 2017; 33:838–49.
Article34. Iacobellis G. Local and systemic effects of the multifaceted epicardial adipose tissue depot. Nat Rev Endocrinol. 2015; 11:363–71.
Article35. Prati F, Arbustini E, Labellarte A, Sommariva L, Pawlowski T, Manzoli A, et al. Eccentric atherosclerotic plaques with positive remodelling have a pericardial distribution: a permissive role of epicardial fat?: a three-dimensional intravascular ultrasound study of left anterior descending artery lesions. Eur Heart J. 2003; 24:329–36.
Article36. Sacks HS, Fain JN, Holman B, Cheema P, Chary A, Parks F, et al. Uncoupling protein-1 and related messenger ribonucleic acids in human epicardial and other adipose tissues: epicardial fat functioning as brown fat. J Clin Endocrinol Metab. 2009; 94:3611–5.37. Hirata Y, Kurobe H, Akaike M, Chikugo F, Hori T, Bando Y, et al. Enhanced inflammation in epicardial fat in patients with coronary artery disease. Int Heart J. 2011; 52:139–42.
Article38. Zhao L, Guo Z, Wang P, Zheng M, Yang X, Liu Y, et al. Proteomics of epicardial adipose tissue in patients with heart failure. J Cell Mol Med. 2020; 24:511–20.
Article39. Agra RM, Teijeira-Fernandez E, Pascual-Figal D, Sanchez-Mas J, Fernandez-Trasancos A, Gonzalez-Juanatey JR, et al. Adiponectin and p53 mRNA in epicardial and subcutaneous fat from heart failure patients. Eur J Clin Invest. 2014; 44:29–37.
Article40. Lai YH, Yun CH, Yang FS, Liu CC, Wu YJ, Kuo JY, et al. Epicardial adipose tissue relating to anthropometrics, metabolic derangements and fatty liver disease independently contributes to serum high-sensitivity C-reactive protein beyond body fat composition: a study validated with computed tomography. J Am Soc Echocardiogr. 2012; 25:234–41.
Article41. Cho DH, Joo HJ, Kim MN, Kim HD, Lim DS, Park SM. Longitudinal change in myocardial function and clinical parameters in middle-aged subjects: a 3-year follow-up study. Diabetes Metab J. 2021; 45:719–29.
Article42. Patel VB, Shah S, Verma S, Oudit GY. Epicardial adipose tissue as a metabolic transducer: role in heart failure and coronary artery disease. Heart Fail Rev. 2017; 22:889–902.
Article43. Kankaanpaa M, Lehto HR, Parkka JP, Komu M, Viljanen A, Ferrannini E, et al. Myocardial triglyceride content and epicardial fat mass in human obesity: relationship to left ventricular function and serum free fatty acid levels. J Clin Endocrinol Metab. 2006; 91:4689–95.
Article44. Malavazos AE, Di Leo G, Secchi F, Lupo EN, Dogliotti G, Coman C, et al. Relation of echocardiographic epicardial fat thickness and myocardial fat. Am J Cardiol. 2010; 105:1831–5.
Article45. Ng AC, Strudwick M, van der Geest RJ, Ng AC, Gillinder L, Goo SY, et al. Impact of epicardial adipose tissue, left ventricular myocardial fat content, and interstitial fibrosis on myocardial contractile function. Circ Cardiovasc Imaging. 2018; 11:e007372.
Article46. Wu CK, Lee JK, Hsu JC, Su MM, Wu YF, Lin TT, et al. Myocardial adipose deposition and the development of heart failure with preserved ejection fraction. Eur J Heart Fail. 2020; 22:445–54.
Article47. Greulich S, de Wiza DH, Preilowski S, Ding Z, Mueller H, Langin D, et al. Secretory products of guinea pig epicardial fat induce insulin resistance and impair primary adult rat cardiomyocyte function. J Cell Mol Med. 2011; 15:2399–410.
Article48. Kim SA, Kim MN, Shim WJ, Park SM. Epicardial adipose tissue is related to cardiac function in elderly women, but not in men. Nutr Metab Cardiovasc Dis. 2017; 27:41–7.
Article49. Iacobellis G, Pistilli D, Gucciardo M, Leonetti F, Miraldi F, Brancaccio G, et al. Adiponectin expression in human epicardial adipose tissue in vivo is lower in patients with coronary artery disease. Cytokine. 2005; 29:251–5.
Article50. Kim MN, Kim HL, Park SM, Shin MS, Yu CW, Kim MA, et al. Association of epicardial adipose tissue with coronary spasm and coronary atherosclerosis in patients with chest pain: analysis of data collated by the KoRean wOmen’S chest pain rEgistry (koROSE). Heart Vessels. 2018; 33:17–24.
Article51. Alexopoulos N, McLean DS, Janik M, Arepalli CD, Stillman AE, Raggi P. Epicardial adipose tissue and coronary artery plaque characteristics. Atherosclerosis. 2010; 210:150–4.
Article52. Kim SR, Cho DH, Kim MN, Park SM. Rationale and study design of differences in cardiopulmonary exercise capacity according to coronary microvascular dysfunction and body composition in patients with suspected heart failure with preserved ejection fraction. Int J Heart Fail. 2021; 3:237–43.
Article53. Alam MS, Green R, de Kemp R, Beanlands RS, Chow BJ. Epicardial adipose tissue thickness as a predictor of impaired microvascular function in patients with non-obstructive coronary artery disease. J Nucl Cardiol. 2013; 20:804–12.
Article54. Fontes-Carvalho R, Fontes-Oliveira M, Sampaio F, Mancio J, Bettencourt N, Teixeira M, et al. Influence of epicardial and visceral fat on left ventricular diastolic and systolic functions in patients after myocardial infarction. Am J Cardiol. 2014; 114:1663–9.
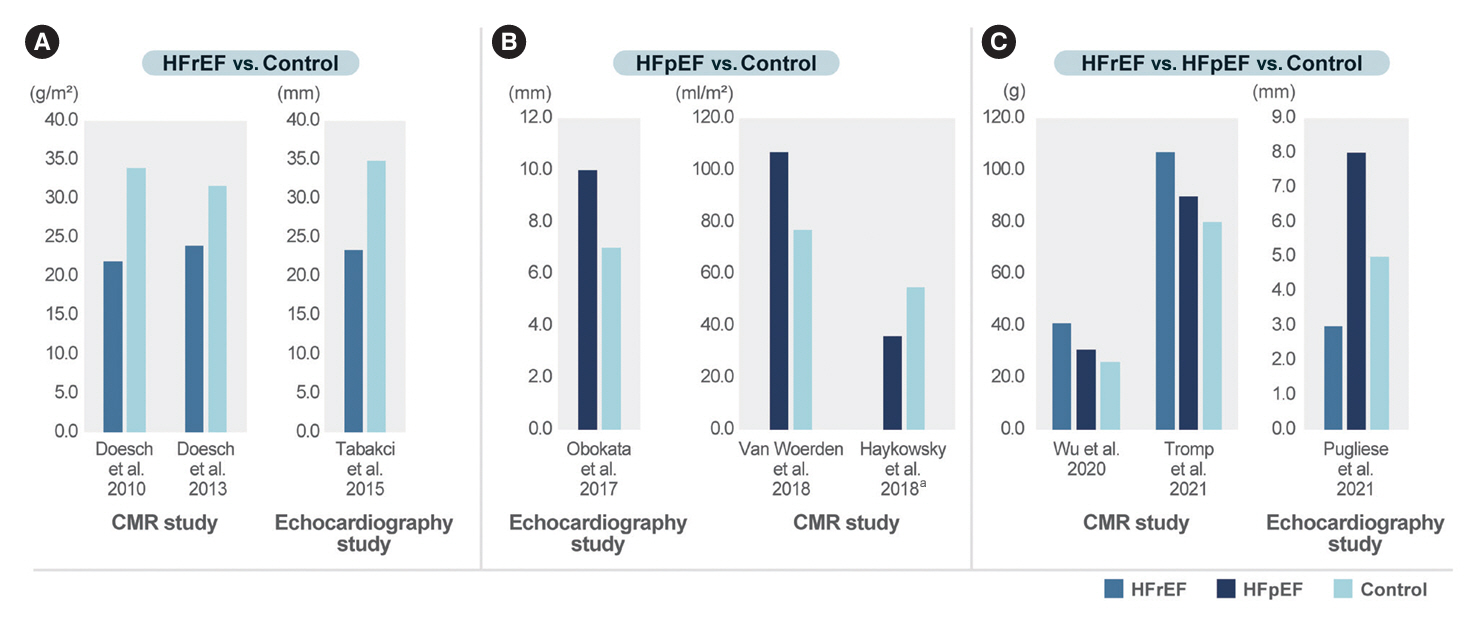
Article55. Doesch C, Haghi D, Fluchter S, Suselbeck T, Schoenberg SO, Michaely H, et al. Epicardial adipose tissue in patients with heart failure. J Cardiovasc Magn Reson. 2010; 12:40.
Article56. Doesch C, Streitner F, Bellm S, Suselbeck T, Haghi D, Heggemann F, et al. Epicardial adipose tissue assessed by cardiac magnetic resonance imaging in patients with heart failure due to dilated cardiomyopathy. Obesity (Silver Spring). 2013; 21:E253–61.
Article57. Tabakci MM, Durmus HI, Avci A, Toprak C, Demir S, Arslantas U, et al. Relation of epicardial fat thickness to the severity of heart failure in patients with nonischemic dilated cardiomyopathy. Echocardiography. 2015; 32:740–8.
Article58. Obokata M, Reddy YN, Pislaru SV, Melenovsky V, Borlaug BA. Evidence supporting the existence of a distinct obese phenotype of heart failure with preserved ejection fraction. Circulation. 2017; 136:6–19.
Article59. Haykowsky MJ, Nicklas BJ, Brubaker PH, Hundley WG, Brinkley TE, Upadhya B, et al. Regional adipose distribution and its relationship to exercise intolerance in older obese patients who have heart failure with preserved ejection fraction. JACC Heart Fail. 2018; 6:640–9.
Article60. van Woerden G, Gorter TM, Westenbrink BD, Willems TP, van Veldhuisen DJ, Rienstra M. Epicardial fat in heart failure patients with mid-range and preserved ejection fraction. Eur J Heart Fail. 2018; 20:1559–66.
Article61. Tromp J, Bryant JA, Jin X, van Woerden G, Asali S, Yiying H, et al. Epicardial fat in heart failure with reduced versus preserved ejection fraction. Eur J Heart Fail. 2021; 23:835–8.
Article62. Valentova M, von Haehling S, Krause C, Ebner N, Steinbeck L, Cramer L, et al. Cardiac cachexia is associated with right ventricular failure and liver dysfunction. Int J Cardiol. 2013; 169:219–24.
Article63. Pugliese NR, Paneni F, Mazzola M, De Biase N, Del Punta L, Gargani L, et al. Impact of epicardial adipose tissue on cardiovascular haemodynamics, metabolic profile, and prognosis in heart failure. Eur J Heart Fail. 2021; 23:1858–71.
Article64. van Woerden G, van Veldhuisen DJ, Manintveld OC, van Empel VP, Willems TP, de Boer RA, et al. Epicardial adipose tissue and outcome in heart failure with mid-range and preserved ejection fraction. Circ Heart Fail. 2022; 15:e009238.
Article65. Kenchaiah S, Ding J, Carr JJ, Allison MA, Budoff MJ, Tracy RP, et al. Pericardial fat and the risk of heart failure. J Am Coll Cardiol. 2021; 77:2638–52.66. Iacobellis G, Bianco AC. Epicardial adipose tissue: emerging physiological, pathophysiological and clinical features. Trends Endocrinol Metab. 2011; 22:450–7.
Article67. Alexopoulos N, Melek BH, Arepalli CD, Hartlage GR, Chen Z, Kim S, et al. Effect of intensive versus moderate lipid-lowering therapy on epicardial adipose tissue in hyperlipidemic postmenopausal women: a substudy of the BELLES trial (Beyond Endorsed Lipid Lowering with EBT Scanning). J Am Coll Cardiol. 2013; 61:1956–61.68. Parisi V, Petraglia L, D’Esposito V, Cabaro S, Rengo G, Caruso A, et al. Statin therapy modulates thickness and inflammatory profile of human epicardial adipose tissue. Int J Cardiol. 2019; 274:326–30.
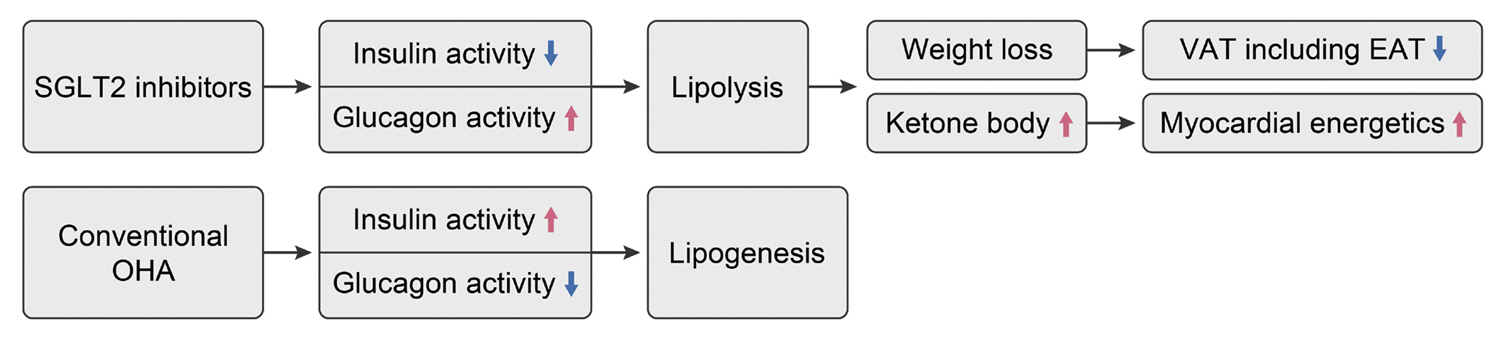
Article69. Park JH, Park YS, Kim YJ, Lee IS, Kim JH, Lee JH, et al. Effects of statins on the epicardial fat thickness in patients with coronary artery stenosis underwent percutaneous coronary intervention: comparison of atorvastatin with simvastatin/ezetimibe. J Cardiovasc Ultrasound. 2010; 18:121–6.70. Braunwald E. SGLT2 inhibitors: the statins of the 21st century. Eur Heart J. 2022; 43:1029–30.71. Kato ET, Kimura T. Sodium-glucose co-transporters-2 inhibitors and heart failure: state of the art review and future potentials. Int J Heart Fail. 2020; 2:12–22.72. Iacobellis G, Baroni MG. Cardiovascular risk reduction throughout GLP-1 receptor agonist and SGLT2 inhibitor modulation of epicardial fat. J Endocrinol Invest. 2022; 45:489–95.73. Cho DH. SGLT2 inhibitors: emerging drugs in heart failure. Korean J Med. 2023; 98:59–63.
Article74. Kim SR, Lee SG, Kim SH, Kim JH, Choi E, Cho W, et al. SGLT2 inhibition modulates NLRP3 inflammasome activity via ketones and insulin in diabetes with cardiovascular disease. Nat Commun. 2020; 11:2127.
Article75. McMurray JJ, Solomon SD, Inzucchi SE, Kober L, Kosiborod MN, Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019; 381:1995–2008.76. Fukuda T, Bouchi R, Terashima M, Sasahara Y, Asakawa M, Takeuchi T, et al. Ipragliflozin reduces epicardial fat accumulation in non-obese type 2 diabetic patients with visceral obesity: a pilot study. Diabetes Ther. 2017; 8:851–61.
Article77. Gaborit B, Ancel P, Abdullah AE, Maurice F, Abdesselam I, Calen A, et al. Effect of empagliflozin on ectopic fat stores and myocardial energetics in type 2 diabetes: the EMPACEF study. Cardiovasc Diabetol. 2021; 20:57.
Article78. Hiruma S, Shigiyama F, Hisatake S, Mizumura S, Shiraga N, Hori M, et al. A prospective randomized study comparing effects of empagliflozin to sitagliptin on cardiac fat accumulation, cardiac function, and cardiac metabolism in patients with early-stage type 2 diabetes: the ASSET study. Cardiovasc Diabetol. 2021; 20:32.
Article79. Iacobellis G, Gra-Menendez S. Effects of dapagliflozin on epicardial fat thickness in patients with type 2 diabetes and obesity. Obesity (Silver Spring). 2020; 28:1068–74.
Article80. Masson W, Lavalle-Cobo A, Nogueira JP. Effect of SGLT2-inhibitors on epicardial adipose tissue: a meta-analysis. Cells. 2021; 10:2150.
Article81. Requena-Ibanez JA, Santos-Gallego CG, Rodriguez-Cordero A, Vargas-Delgado AP, Mancini D, Sartori S, et al. Mechanistic insights of empagliflozin in nondiabetic patients with HFrEF: from the EMPA-TROPISM study. JACC Heart Fail. 2021; 9:578–89.82. Kosiborod MN, Abildstrom SZ, Borlaug BA, Butler J, Rasmussen S, Davies M, et al. Semaglutide in patients with heart failure with preserved ejection fraction and obesity. N Engl J Med. 2023; 389:1069–84.83. Romanelli MM, Vianello E, Malavazos AE, Tacchini L, Schmitz G, Iacobellis G, et al. GLP‐1 receptor is associated with genes involved in fatty acids oxidation and white‐to‐brown fat differentiation in epicardial adipose tissue (EAT). FASEB J. 2019; 33(S1):662.
Article84. Iacobellis G, Mohseni M, Bianco SD, Banga PK. Liraglutide causes large and rapid epicardial fat reduction. Obesity (Silver Spring). 2017; 25:311–6.
Article85. Iacobellis G, Villasante Fricke AC. Effects of semaglutide versus dulaglutide on epicardial fat thickness in subjects with type 2 diabetes and obesity. J Endocr Soc. 2020; 4:bvz042.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Non-calcified Coronary Plaque Burden is Related to Epicardial Adipose Tissue and Peri-coronary Adipose Tissue Attenuation in Heart Failure With Preserved Ejection Fraction
- Is Shank3 a ‘Friend or Foe’ of the Heart? Its Role in Cardiac Calcium Homeostasis
- A case of prominent epicardial fat mimicking a tumor on echocardiography
- Metabolically healthy obesity: a friend or foe?
- Anti-tumor Necrosis Factor Therapy for Crohn Disease: Friend or Foe to the Surgeon?