J Korean Assoc Oral Maxillofac Surg.
2024 Apr;50(2):70-79. 10.5125/jkaoms.2024.50.2.70.
A 10-year follow-up study on clinical outcomes of dental implant rehabilitation using surgical guide
- Affiliations
-
- 1Department of Oral and Maxillofacial Surgery, Dental Research Institute, School of Dentistry, Seoul National University, Seoul, Korea
- KMID: 2555736
- DOI: http://doi.org/10.5125/jkaoms.2024.50.2.70
Abstract
Objectives
The surgical guide is a static computer-assisted device used for implant surgery planning and guidance. By taking an impression and referring to the patients’ three-dimensional computed tomography scan of the desired implant site, a surgical guide can be created. During surgery, the surgical guide aids in achieving the designed implant placement position and direction. We examined and evaluated the long-term clinical outcomes of implant surgery using surgical guides.
Materials and Methods
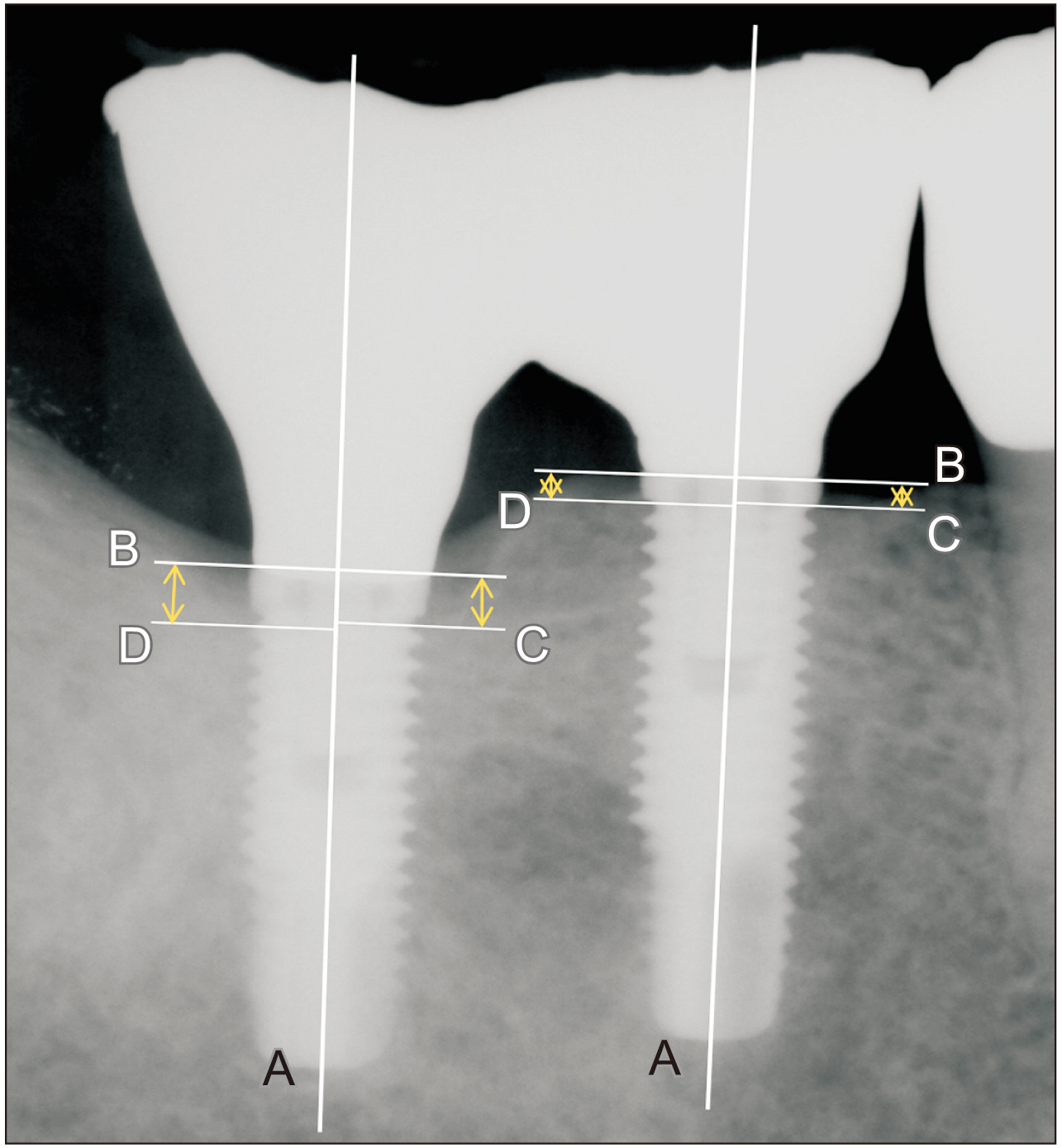
This study investigated a total of 15 patients with 32 implants that were placed using surgical guides from 2009 to 2011 with a mean follow-up period extended beyond 10 years. Patient demographics and implant survival rates were recorded. We analyzed marginal bone loss (MBL) by assessing the radiographs acquired at installation, three months after installation, and one month, one, two, and five years after prosthesis delivery.
Results
The mean patient age was 57.33 years at implant placement. Of the 32 implants, five implants were placed in the anterior region and 27 implants were in the posterior region. Six implants failed and three of them were replaced, resulting in an 81.25% survival rate. The mean follow-up period was 10 years and nine months. Mean MBL compared to post-installation was significantly higher than at three months after installation, and one month, one, two, and five years after prosthesis delivery. Mean MBL at three months after installation, and one month, one year, and two years were significantly higher compared to the previous visit (P<0.05). However, MBL at five years after prosthesis delivery did not differ significantly compared to at two years.
Conclusion
In this study, implant rehabilitation assisted by surgical guides exhibited favorable survival rates. With the limitation of the sample amount in this study, further research and more samples are required to evaluate the long-term clinical effectiveness of surgical guides.
Keyword
Figure
Reference
-
References
1. Chen X, Xu L, Wang W, Li X, Sun Y, Politis C. 2016; Computer-aided design and manufacturing of surgical templates and their clinical applications: a review. Expert Rev Med Devices. 13:853–64. https://doi.org/10.1080/17434440.2016.1218758. DOI: 10.1080/17434440.2016.1218758. PMID: 27479020.
Article2. D'haese J, Ackhurst J, Wismeijer D, De Bruyn H, Tahmaseb A. 2017; Current state of the art of computer-guided implant surgery. Periodontol 2000. 73:121–33. https://doi.org/10.1111/prd.12175. DOI: 10.1111/prd.12175. PMID: 28000275.3. Vercruyssen M, Hultin M, Van Assche N, Svensson K, Naert I, Quirynen M. 2014; Guided surgery: accuracy and efficacy. Periodontol 2000. 66:228–46. https://doi.org/10.1111/prd.12046. DOI: 10.1111/prd.12046. PMID: 25123771.
Article4. Kernen F, Kramer J, Wanner L, Wismeijer D, Nelson K, Flügge T. 2020; A review of virtual planning software for guided implant surgery - data import and visualization, drill guide design and manufacturing. BMC Oral Health. 20:251. https://doi.org/10.1186/s12903-020-01208-1. DOI: 10.1186/s12903-020-01208-1. PMID: 32912273. PMCID: PMC7488021.
Article5. Camargos GV, Rangel EF, Rangel KF, Machado AR, Damis LFT, Gonçalves LC, et al. 2022; Guided implant surgery workflow in edentulous patients: a precise and rapid technique. J Prosthet Dent. 128:239–44. https://doi.org/10.1016/j.prosdent.2020.12.047. DOI: 10.1016/j.prosdent.2020.12.047. PMID: 33632531.
Article6. El Kholy K, Lazarin R, Janner SFM, Faerber K, Buser R, Buser D. 2019; Influence of surgical guide support and implant site location on accuracy of static computer-assisted implant surgery. Clin Oral Implants Res. 30:1067–75. https://doi.org/10.1111/clr.13520. DOI: 10.1111/clr.13520. PMID: 31381178.
Article7. Tahmaseb A, Wu V, Wismeijer D, Coucke W, Evans C. 2018; The accuracy of static computer-aided implant surgery: a systematic review and meta-analysis. Clin Oral Implants Res. 29 Suppl 16:416–35. https://doi.org/10.1111/clr.13346. DOI: 10.1111/clr.13346. PMID: 30328191.
Article8. D'haese J, Van De Velde T, Komiyama A, Hultin M, De Bruyn H. 2012; Accuracy and complications using computer-designed stereolithographic surgical guides for oral rehabilitation by means of dental implants: a review of the literature. Clin Implant Dent Relat Res. 14:321–35. https://doi.org/10.1111/j.1708-8208.2010.00275.x. DOI: 10.1111/j.1708-8208.2010.00275.x. PMID: 20491822.9. Shen P, Zhao J, Fan L, Qiu H, Xu W, Wang Y, et al. 2015; Accuracy evaluation of computer-designed surgical guide template in oral implantology. J Craniomaxillofac Surg. 43:2189–94. https://doi.org/10.1016/j.jcms.2015.10.022. DOI: 10.1016/j.jcms.2015.10.022. PMID: 26776292.
Article10. Lee JH, Park JM, Kim SM, Kim MJ, Lee JH, Kim MJ. 2013; An assessment of template-guided implant surgery in terms of accuracy and related factors. J Adv Prosthodont. 5:440–7. https://doi.org/10.4047/jap.2013.5.4.440. DOI: 10.4047/jap.2013.5.4.440. PMID: 24353883. PMCID: PMC3865200.
Article11. Scherer U, Stoetzer M, Ruecker M, Gellrich NC, von See C. 2015; Template-guided vs. non-guided drilling in site preparation of dental implants. Clin Oral Investig. 19:1339–46. https://doi.org/10.1007/s00784-014-1346-7. DOI: 10.1007/s00784-014-1346-7. PMID: 25354488.
Article12. Esposito M, Grusovin MG, Worthington HV. 2012; Interventions for replacing missing teeth: treatment of peri-implantitis. Cochrane Database Syst Rev. 1(1):CD004970. https://doi.org/10.1002/14651858.cd004970.pub5. DOI: 10.1002/14651858.CD004970.pub5.
Article13. Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, Trisi P, et al. 2008; Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent. 17:5–15. https://doi.org/10.1097/id.0b013e3181676059. DOI: 10.1097/ID.0b013e3181676059. PMID: 18332753.
Article14. Sodnom-Ish B, Eo MY, Kim MJ, Kim SM. 2023; A 10-year survival rate of tapered self-tapping bone-level implants from medically compromised Korean patients at a maxillofacial surgical unit. Maxillofac Plast Reconstr Surg. 45:35. https://doi.org/10.1186/s40902-023-00401-w. DOI: 10.1186/s40902-023-00401-w. PMID: 37801094. PMCID: PMC10558417.
Article15. Turbush SK, Turkyilmaz I. 2012; Accuracy of three different types of stereolithographic surgical guide in implant placement: an in vitro study. J Prosthet Dent. 108:181–8. https://doi.org/10.1016/s0022-3913(12)60145-0. DOI: 10.1016/S0022-3913(12)60145-0. PMID: 22944314.
Article16. Ozan O, Turkyilmaz I, Ersoy AE, McGlumphy EA, Rosenstiel SF. 2009; Clinical accuracy of 3 different types of computed tomography-derived stereolithographic surgical guides in implant placement. J Oral Maxillofac Surg. 67:394–401. https://doi.org/10.1016/j.joms.2008.09.033. DOI: 10.1016/j.joms.2008.09.033. PMID: 19138616.
Article17. Verhamme LM, Meijer GJ, Boumans T, de Haan AF, Bergé SJ, Maal TJ. 2015; A clinically relevant accuracy study of computer-planned implant placement in the edentulous maxilla using mucosa-supported surgical templates. Clin Implant Dent Relat Res. 17:343–52. https://doi.org/10.1111/cid.12112. DOI: 10.1111/cid.12112. PMID: 23879524.
Article18. Tang CB, Liul SY, Zhou GX, Yu JH, Zhang GD, Bao YD, et al. 2012; Nonlinear finite element analysis of three implant- abutment interface designs. Int J Oral Sci. 4:101–8. https://doi.org/10.1038/ijos.2012.35. DOI: 10.1038/ijos.2012.35. PMID: 22699263. PMCID: PMC3412669.
Article19. Freitas-Júnior AC, Rocha EP, Bonfante EA, Almeida EO, Anchieta RB, Martini AP, et al. 2012; Biomechanical evaluation of internal and external hexagon platform switched implant-abutment connections: an in vitro laboratory and three-dimensional finite element analysis. Dent Mater. 28:e218–28. https://doi.org/10.1016/j.dental.2012.05.004. DOI: 10.1016/j.dental.2012.05.004. PMID: 22682782.
Article20. Tripodi D, Vantaggiato G, Scarano A, Perrotti V, Piattelli A, Iezzi G, et al. 2012; An in vitro investigation concerning the bacterial leakage at implants with internal hexagon and Morse taper implant-abutment connections. Implant Dent. 21:335–9. https://doi.org/10.1097/id.0b013e31825cd472. DOI: 10.1097/ID.0b013e31825cd472. PMID: 22814560.
Article21. Gracis S, Michalakis K, Vigolo P, Vult von Steyern P, Zwahlen M, Sailer I. 2012; Internal vs. external connections for abutments/reconstructions: a systematic review. Clin Oral Implants Res. 23 Suppl 6:202–16. https://doi.org/10.1111/j.1600-0501.2012.02556.x. DOI: 10.1111/j.1600-0501.2012.02556.x. PMID: 23062143.
Article22. Frösch L, Mukaddam K, Filippi A, Zitzmann NU, Kühl S. 2019; Comparison of heat generation between guided and conventional implant surgery for single and sequential drilling protocols-an in vitro study. Clin Oral Implants Res. 30:121–30. https://doi.org/10.1111/clr.13398. DOI: 10.1111/clr.13398. PMID: 30578579.
Article23. Hinckfuss S, Conrad HJ, Lin L, Lunos S, Seong WJ. 2012; Effect of surgical guide design and surgeon's experience on the accuracy of implant placement. J Oral Implantol. 38:311–23. https://doi.org/10.1563/aaid-joi-d-10-00046. DOI: 10.1563/AAID-JOI-D-10-00046. PMID: 20712446.
Article24. Tatakis DN, Chien HH, Parashis AO. 2019; Guided implant surgery risks and their prevention. Periodontol 2000. 81:194–208. https://doi.org/10.1111/prd.12292. DOI: 10.1111/prd.12292. PMID: 31407433.
Article25. Carbajal Mejía JB, Wakabayashi K, Nakano T, Yatani H. 2016; Marginal bone loss around dental implants inserted with static computer assistance in healed sites: a systematic review and meta-analysis. Int J Oral Maxillofac Implants. 31:761–75. https://doi.org/10.11607/jomi.4727. DOI: 10.11607/jomi.4727. PMID: 27447141.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Precautions for Implant Placement using Computer-guided Implant Surgical Guide: A Systematic Review
- Full Mouth Rehabilitation with Modeless Implant Restoration using a Two-step Surgical Guide System: A Case Report
- An assessment of accuracy of half-guided implant surgery using implant surgical guide: A case report
- An analysis on satisfaction level of clinicians on implant surgical guidance system based on computed tomography
- Flapless implant placement with digital 3D imaging and planning system in fully edentulous patient: A case report and 5-year follow-up