Ann Surg Treat Res.
2024 May;106(5):248-254. 10.4174/astr.2024.106.5.248.
Outcomes of carotid endarterectomy in octogenarians compared to their younger counterparts: a retrospective observational study
- Affiliations
-
- 1Division of Vascular Surgery, Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Vascular Surgery, Department of Surgery, Incheon Sejong Hospital, Incheon, Korea
- KMID: 2555721
- DOI: http://doi.org/10.4174/astr.2024.106.5.248
Abstract
- Purpose
This study was performed to analyze the association between age and outcomes of carotid endarterectomy (CEA) by comparing postoperative outcomes between octogenarians and younger patients.
Methods
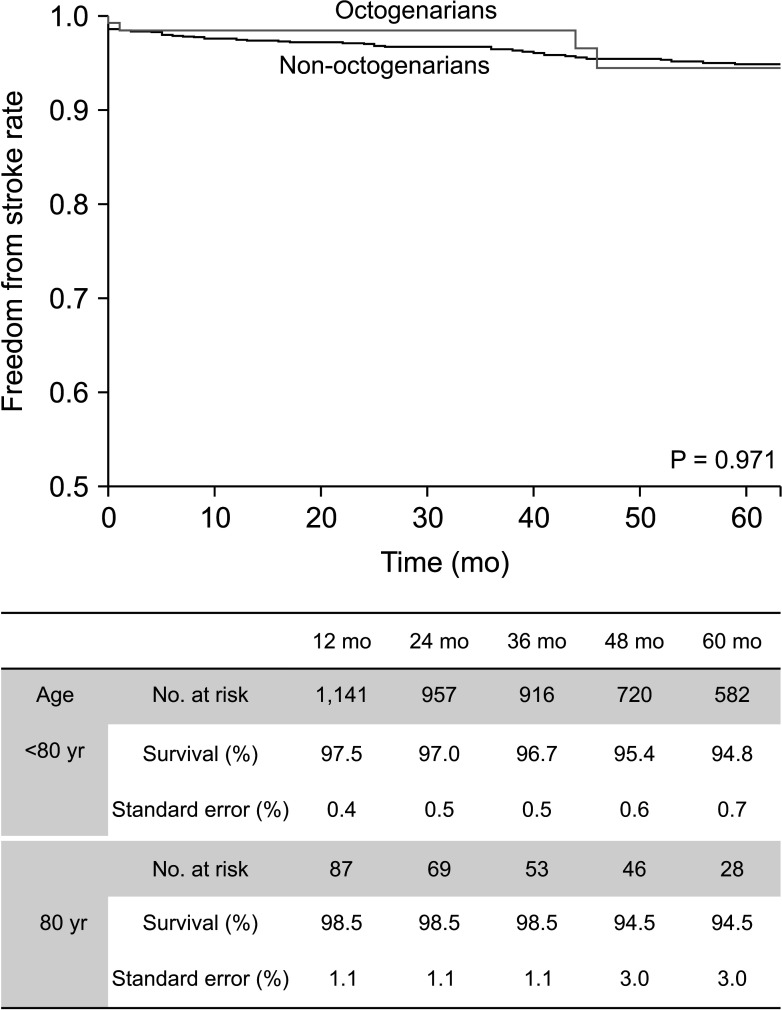
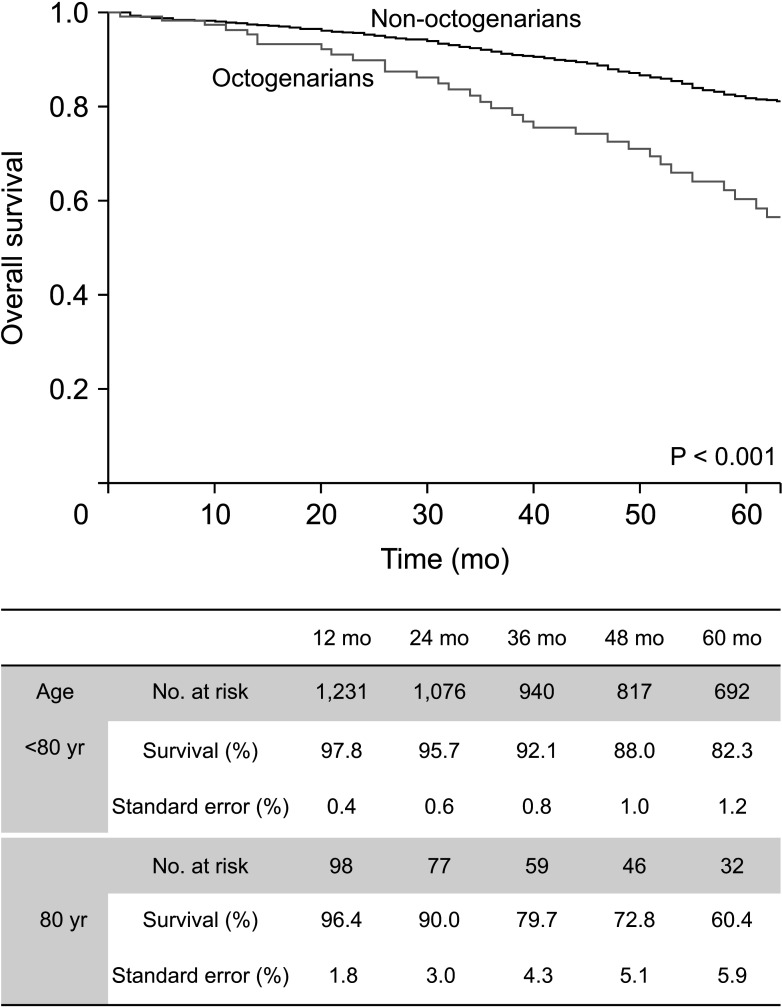
From November 1994 to December 2022, 1,585 internal carotid arteries of 1,434 patients were enrolled. Patients were stratified into 2 groups: octogenarians (≥80 years old) and non-octogenarians (<80 years old). Primary endpoints were early (≤30 days) outcomes of ipsilateral stroke, any stroke, myocardial infarction, death, and major adverse cardiovascular events (MACE). We also compared overall any stroke and death between the 2 groups.
Results
One of 132 octogenarians (0.8%) and 17 of 1,453 non-octogenarians (1.1%) experienced ipsilateral stroke within 30 days. Thirty-day MACE occurred in 4 of 132 octogenarians (3%) and 44 of 1,453 non-octogenarians (3%). There were no significant differences in any early (≤30 days) outcomes. Symptomatic status was associated with increased 30-day MACE (odds ratio [OR], 2.610; 95% confidence interval [CI], 1.450–4.696; P = 0.003) and 30-day any stroke (OR, 3.999; 95% CI, 1.627–9.828; P = 0.003). Symptomatic status was also associated with overall any stroke (hazard ratio [HR], 2.885; 95% CI, 1.865–4.463; P < 0.001), but age of ≥80 years was not associated with 30-day MACE, 30-day any stroke, or overall stroke. Age of ≥80 years was only associated with overall survival (HR, 2.644; 95% CI, 1.967–3.555; P < 0.001).
Conclusion
CEA would be a safe and effective treatment for octogenarians with low 30-day complications and long-term stroke rates, comparable with that of younger counterparts. Advanced age is not a contraindication for CEA.
Figure
Reference
-
1. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012; 380:2095–2128. PMID: 23245604.2. Krawisz AK, Carroll BJ, Secemsky EA. Risk stratification and management of extracranial carotid artery disease. Cardiol Clin. 2021; 39:539–549. PMID: 34686266.3. AbuRahma AF, Avgerinos ED, Chang RW, Darling RC 3rd, Duncan AA, Forbes TL, et al. Society for Vascular Surgery clinical practice guidelines for management of extracranial cerebrovascular disease. J Vasc Surg. 2022; 75(1S):4S–22S. PMID: 34153348.4. Yadav JS, Wholey MH, Kuntz RE, Fayad P, Katzen BT, Mishkel GJ, et al. Protected carotid-artery stenting versus endarterectomy in high-risk patients. N Engl J Med. 2004; 351:1493–1501. PMID: 15470212.5. Schneider JR, Jackson CR, Helenowski IB, Verta MJ, Wilkinson JB, Kim S, et al. A comparison of results of carotid endarterectomy in octogenarians and nonagenarians to younger patients from the Mid-America Vascular Study Group and the Society for Vascular Surgery Vascular Quality Initiative. J Vasc Surg. 2017; 65:1643–1652. PMID: 28259574.6. Nantakool S, Chuatrakoon B, Orrapin S, Leung R, Howard DP, Rerkasem A, et al. Influences of age and gender on operative risks following carotid endarterectomy: a systematic review and meta-analysis. PLoS One. 2023; 18:e0285540. PMID: 37163559.7. Glousman BN, Sebastian R, Macsata R, Kuang X, Yang A, Patel D, et al. Carotid endarterectomy for asymptomatic carotid stenosis is safe in octogenarians. J Vasc Surg. 2020; 71:518–524. PMID: 31471235.8. Ricotta JJ, Aburahma A, Ascher E, Eskandari M, Faries P, Lal BK, et al. Updated Society for Vascular Surgery guidelines for management of extracranial carotid disease: executive summary. J Vasc Surg. 2011; 54:832–836. PMID: 21889705.9. Fahad S, Shirsath S, Metcalfe M, Elmallah A. Carotid endarterectomy in the very elderly: short-, medium-, and long-term outcomes. Vasc Specialist Int. 2023; 39:28. PMID: 37748930.10. Jeong MJ, Kwon SU, Kim MJ, Han Y, Kwon TW, Cho YP. Effects of patient age on outcomes after carotid endarterectomy: a retrospective, single-center study in Korea. Medicine (Baltimore). 2019; 98:e16781. PMID: 31393403.11. Ball S, Ball A, Antoniou GA. Editor’s choice: prognostic role of pre-operative symptom status in carotid endarterectomy: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2020; 59:516–524. PMID: 32081531.12. Jeong MJ, Kwon H, Kim MJ, Han Y, Kwon TW, Cho YP. Effect of severe contralateral carotid stenosis or occlusion on early and late outcomes after carotid endarterectomy. Ann Surg Treat Res. 2019; 97:202–209. PMID: 31620394.13. Reiff T, Eckstein HH, Mansmann U, Jansen O, Fraedrich G, Mudra H, et al. Carotid endarterectomy or stenting or best medical treatment alone for moderate-to-severe asymptomatic carotid artery stenosis: 5-year results of a multicentre, randomised controlled trial. Lancet Neurol. 2022; 21:877–888. PMID: 36115360.14. Kernan WN, Ovbiagele B, Black HR, Bravata DM, Chimowitz MI, Ezekowitz MD, et al. Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160–2236. PMID: 24788967.15. Kang J, Woo SY, Yang SS, Park YJ, Kim DI, Jeon P, et al. Treatment results of carotid endarterectomy and carotid artery stenting for patients with radiation-induced carotid stenosis. Ann Surg Treat Res. 2022; 103:112–118. PMID: 36017138.16. Mendez-Sosa MA, Contreras-Jimenez E, Anaya-Ayala JE, Miranda-Ramirez MW, Lopez-Pena G, Arzola LH, et al. Surgical management of a type II extracranial internal carotid aneurysm near to the skull base. Vasc Specialist Int. 2021; 37:27. PMID: 34349047.17. Howard G, Roubin GS, Jansen O, Hendrikse J, Halliday A, Fraedrich G, et al. Association between age and risk of stroke or death from carotid endarterectomy and carotid stenting: a meta-analysis of pooled patient data from four randomised trials. Lancet. 2016; 387:1305–1311. PMID: 26880122.18. Kleindorfer DO, Towfighi A, Chaturvedi S, Cockroft KM, Gutierrez J, Lombardi-Hill D, et al. 2021 Guideline for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline from the American Heart Association/American Stroke Association. Stroke. 2021; 52:e364–e467. PMID: 34024117.19. Park JK, Woo SY, Park YJ, Kim DI, Kim GM, Seo WK, et al. The Impact of age and outcomes of high-risk patients on carotid revascularization. Vascular. 2023; 17085381231155035. PMID: 36794829.20. Seo KD, Lee KY, Suh SH. Comparison of long term prognosis between carotid endarterectomy versus stenting; a Korean population-based study using national insurance data. Neurointervention. 2019; 14:82–90. PMID: 31450880.21. Lichtman JH, Jones MR, Leifheit EC, Sheffet AJ, Howard G, Lal BK, et al. Carotid endarterectomy and carotid artery stenting in the US medicare population, 1999-2014. JAMA. 2017; 318:1035–1046. PMID: 28975306.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Safety after Percutaneous Coronary Intervention Between Octogenarians and Counterparts with Coronary Artery Disease
- Is Carotid Stenting a Reasonable Alternative to Carotid Endarterectomy?
- Microsurgical Endarterectomy for Symptomatic Carotid Artery Stenosis
- Complication of Carotid Endarterectomy
- Carotid Angioplasty: Is it Safe as Carotid Endarterectomy?