Korean Circ J.
2024 Apr;54(4):203-217. 10.4070/kcj.2023.0312.
The Effects of Radiofrequency Catheter Ablation for Atrial Fibrillation on Right Ventricular Function
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yongin Severance Hospital, Yonsei University College of Medicine, Yongin, Korea
- 2Division of Cardiology, Department of Internal Medicine, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Biostatistics, Department of Biomedical Systems Informatics, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2555533
- DOI: http://doi.org/10.4070/kcj.2023.0312
Abstract
- Background and Objective
The effects of radiofrequency catheter ablation (RFCA) for atrial fibrillation (AF) on right ventricular (RV) function are not well known.
Methods
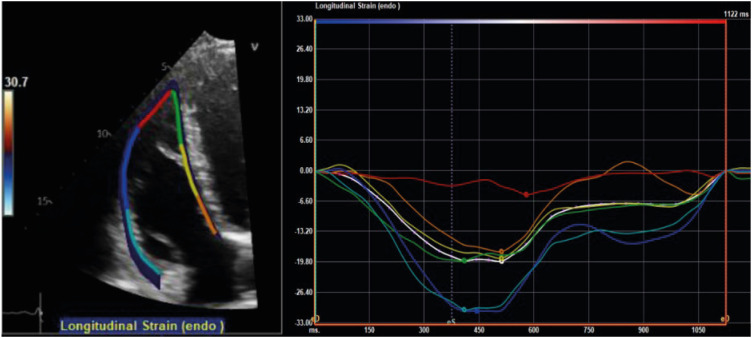
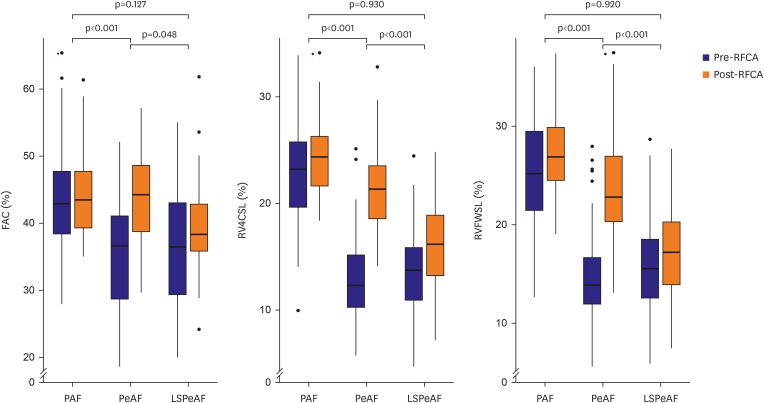
Patients who underwent RFCA for AF and underwent pre- and post-procedural echocardiography were enrolled consecutively. Fractional area change (FAC), RV free-wall longitudinal strain (RVFWSL), and RV 4-chamber strain including the ventricular septum (RV4CSL) were measured. Changes in FAC, RVFWSL, and RV4CSL before and after RFCA were compared among paroxysmal AF (PAF), persistent AF (PeAF), and long-standing persistent AF (LSPeAF) groups.
Results
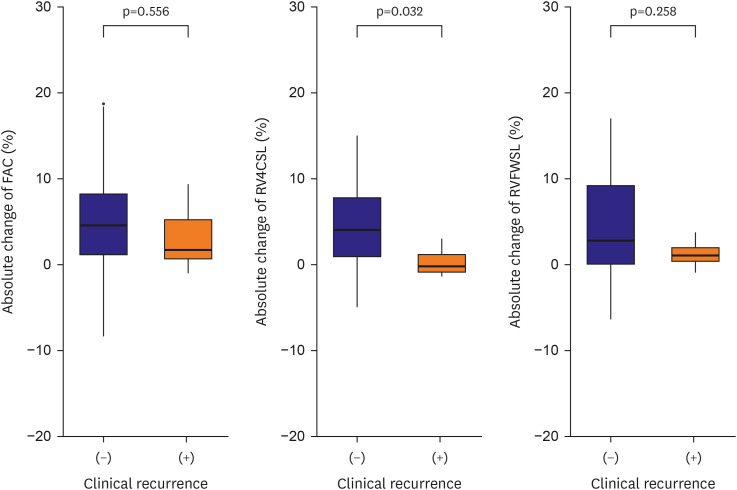
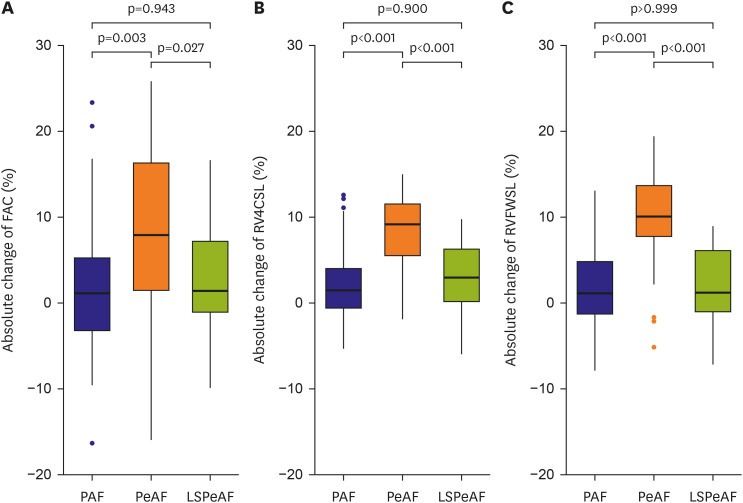
A total of 164 participants (74 PAF, 47 PeAF, and 43 LSPeAF; age, 60.8 ± 9.8 years; men, 74.4%) was enrolled. The patients with PeAF and LSPeAF had worse RV4CSL (p<0.001) and RVFWSL (p<0.001) than those with PAF and reference values. Improvements in RVFWSL and RV4CSL after RFCA were significant in the PeAF group compared with the PAF and LSPeAF groups (ΔRV4CSL, 8.4% [5.1, 11.6] in PeAF vs. 1.0% [−1.0, 4.1] in PAF, 1.9% [−0.2, 4.4] in LSPeAF, p<0.001; ΔRVFWSL, 9.0% [6.9, 11.5] in PeAF vs. 0.9% [−1.4, 4.9] in PAF, 1.0% [−1.0, 3.6] in LSPeAF, p<0.001). In patients without recurrence, improvements in RVFWSL and RV4CSL after RFCA were significant in the PeAF group compared to the LSPeAF group.
Conclusions
RV systolic function is more impaired in patients with PeAF and LSPeAF than in those with PAF. RV systolic function is more improved after RFCA in patients with PeAF than in those with PAF or LSPeAF.
Keyword
Figure
Reference
-
1. Schnabel RB, Yin X, Gona P, et al. 50 Year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: a cohort study. Lancet. 2015; 386:154–162. PMID: 25960110.2. Marrouche NF, Brachmann J, Andresen D, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018; 378:417–427. PMID: 29385358.3. Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018; 20:e1–e160.4. Gorter TM, van Melle JP, Rienstra M, et al. Right heart dysfunction in heart failure with preserved ejection fraction: the impact of atrial fibrillation. J Card Fail. 2018; 24:177–185. PMID: 29197548.5. Fung JW, Sanderson JE, Yip GW, Zhang Q, Yu CM. Impact of atrial fibrillation in heart failure with normal ejection fraction: a clinical and echocardiographic study. J Card Fail. 2007; 13:649–655. PMID: 17923357.6. Itakura K, Hidaka T, Nakano Y, et al. Successful catheter ablation of persistent atrial fibrillation is associated with improvement in functional tricuspid regurgitation and right heart reverse remodeling. Heart Vessels. 2020; 35:842–851. PMID: 31897639.7. Zaidi A, Knight DS, Augustine DX, et al. Echocardiographic assessment of the right heart in adults: a practical guideline from the British Society of Echocardiography. Echo Res Pract. 2020; 7:G19–G41. PMID: 32105053.8. Rudski LG, Lai WW, Afilalo J, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. 2010; 23:685–713. PMID: 20620859.9. Kim M, Lee HJ, Park JB, et al. Preoperative right ventricular free-wall longitudinal strain as a prognosticator in isolated surgery for severe functional tricuspid regurgitation. J Am Heart Assoc. 2021; 10:e019856. PMID: 33870734.10. Prihadi EA, van der Bijl P, Dietz M, et al. Prognostic implications of right ventricular free wall longitudinal strain in patients with significant functional tricuspid regurgitation. Circ Cardiovasc Imaging. 2019; 12:e008666. PMID: 30879327.11. Lee JH, Park JH. Strain analysis of the right ventricle using two-dimensional echocardiography. J Cardiovasc Imaging. 2018; 26:111–124. PMID: 30310878.12. Park JH, Park YS, Park SJ, et al. Midventricular peak systolic strain and Tei index of the right ventricle correlated with decreased right ventricular systolic function in patients with acute pulmonary thromboembolism. Int J Cardiol. 2008; 125:319–324. PMID: 17434620.13. Hindricks G, Potpara T, Dagres N, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021; 42:373–498. PMID: 32860505.14. Pieske B, Tschöpe C, de Boer RA, et al. How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur Heart J. 2019; 40:3297–3317. PMID: 31504452.15. Skali H, Uno H, Levey AS, Inker LA, Pfeffer MA, Solomon SD. Prognostic assessment of estimated glomerular filtration rate by the new Chronic Kidney Disease Epidemiology Collaboration equation in comparison with the Modification of Diet in Renal Disease Study equation. Am Heart J. 2011; 162:548–554. PMID: 21884875.16. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.17. Badano LP, Kolias TJ, Muraru D, et al. Standardization of left atrial, right ventricular, and right atrial deformation imaging using two-dimensional speckle tracking echocardiography: a consensus document of the EACVI/ASE/Industry Task Force to standardize deformation imaging. Eur Heart J Cardiovasc Imaging. 2018; 19:591–600. PMID: 29596561.18. Morris DA, Krisper M, Nakatani S, et al. Normal range and usefulness of right ventricular systolic strain to detect subtle right ventricular systolic abnormalities in patients with heart failure: a multicentre study. Eur Heart J Cardiovasc Imaging. 2017; 18:212–223. PMID: 26873461.19. Writing Committee Members. Joglar JA, Chung MK, et al. 2023 ACC/AHA/ACCP/HRS guideline for the diagnosis and management of atrial fibrillation: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2024; 83:109–279. PMID: 38043043.20. Mahmud M, Champion HC. Right ventricular failure complicating heart failure: pathophysiology, significance, and management strategies. Curr Cardiol Rep. 2007; 9:200–208. PMID: 17470333.21. Généreux P, Pibarot P, Redfors B, et al. Staging classification of aortic stenosis based on the extent of cardiac damage. Eur Heart J. 2017; 38:3351–3358. PMID: 29020232.22. Freed BH, Tsang W, Bhave NM, et al. Right ventricular strain in pulmonary arterial hypertension: a 2D echocardiography and cardiac magnetic resonance study. Echocardiography. 2015; 32:257–263. PMID: 24975738.23. Lee K, Kwon O, Lee EJ, et al. Prognostic value of echocardiographic parameters for right ventricular function in patients with acute non-massive pulmonary embolism. Heart Vessels. 2019; 34:1187–1195. PMID: 30671642.24. Kim D, Park Y, Choi KH, et al. Prognostic implication of RV coupling to pulmonary circulation for successful weaning from extracorporeal membrane oxygenation. JACC Cardiovasc Imaging. 2021; 14:1523–1531. PMID: 33865793.25. Nishimura S, Izumi C, Yamasaki S, et al. Impact of right ventricular function on development of significant tricuspid regurgitation in patients with chronic atrial fibrillation. J Cardiol. 2020; 76:431–437. PMID: 32763125.26. Tian F, Zhang L, Xie Y, et al. 3-Dimensional versus 2-dimensional STE for right ventricular myocardial fibrosis in patients with end-stage heart failure. JACC Cardiovasc Imaging. 2021; 14:1309–1320. PMID: 33744147.27. Andersen S, Nielsen-Kudsk JE, Vonk Noordegraaf A, de Man FS. Right ventricular fibrosis. Circulation. 2019; 139:269–285. PMID: 30615500.28. Park JH, Negishi K, Kwon DH, Popovic ZB, Grimm RA, Marwick TH. Validation of global longitudinal strain and strain rate as reliable markers of right ventricular dysfunction: comparison with cardiac magnetic resonance and outcome. J Cardiovasc Ultrasound. 2014; 22:113–120. PMID: 25309687.29. Kim HK, Kim YJ, Park JS, et al. Determinants of the severity of functional tricuspid regurgitation. Am J Cardiol. 2006; 98:236–242. PMID: 16828600.30. Liżewska-Springer A, Dąbrowska-Kugacka A, Lewicka E, et al. Echocardiographic assessment in patients with atrial fibrillation (AF) and normal systolic left ventricular function before and after catheter ablation: if AF begets AF, does pulmonary vein isolation terminate the vicious circle? Cardiol J. 2020; 27:126–135. PMID: 30701515.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Successful Ablation of Right-Sided Accessory Pathway during Atrial Fibrillation
- A Case of Chronic Radiodermatitis following Radiofrequency Catheter Ablation for Atrial Fibrillation
- Catheter ablation for treatment of tachyarrhythmia
- Radiofrequency Catheter Ablation of Persistent Atrial Fibrillation with Myotonic Dystrophy and Achalasia-like Esophageal Dilatation
- Cerebral Infarction After Radiofrequency Catheter Ablation in Patients With Paroxysmal Atrial Fibrillation