J Korean Med Sci.
2024 May;39(18):e151. 10.3346/jkms.2024.39.e151.
Impact of Infection Prevention Programs on Catheter-Associated Urinary Tract Infections Analyzed in Multicenter Study
- Affiliations
-
- 1Division of Infectious Disease, Department of Internal Medicine, Kangnam Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea
- 2Division of Infectious Diseases, Department of Internal Medicine, Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 3Division of Infectious Diseases, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Division of Infectious Diseases, Department of Internal Medicine, Yonsei University Wonju Severance Christian Hospital, Yonsei University Wonju College of Medicine, Wonju, Korea
- 5Department of Laboratory Medicine, Hallym University Kangnam Sacred Heart Hospital, College of Medicine, Hallym University, Seoul, Korea
- 6Division of Infectious Diseases, Department of Internal Medicine, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea
- 7Infection Control Office, Korea University Guro Hospital, Seoul, Korea
- 8Infection Control Office, Inje University Sanggye Paik Hospital, Seoul, Korea
- 9Korean Association of Infection Control Nurses, Seoul, Korea
- 10Infection Control Office, Seoul National University Bundang Hospital, Seongnam, Korea
- 11Infection Control Office, Korea University Ansan Hospital, Ansan, Korea
- 12Infection Control Office, Chung-Ang University Healthcare System, Seoul, Korea
- 13Infection Control Office, Gangnam Severance Hospital, Yonsei University, Seoul, Korea
- 14Infection Control Office, Soonchunhyang University Seoul Hospital, Seoul, Korea
- 15Infection Control Office, Ewha Womans University Mokdong Hospital, Seoul, Korea
- 16School of Nursing, College of Medicine, Soonchunhyang University, Cheonan, Korea
- KMID: 2555501
- DOI: http://doi.org/10.3346/jkms.2024.39.e151
Abstract
- Background
Catheter-associated urinary tract infections (CAUTIs) account for a large proportion of healthcare-associated infections and have a significant impact on morbidity, length of hospital stay, and mortality. Adherence to the recommended infection prevention practices can effectively reduce the incidence of CAUTIs. This study aimed to assess the characteristics of CAUTIs and the efficacy of prevention programs across hospitals of various sizes.
Methods
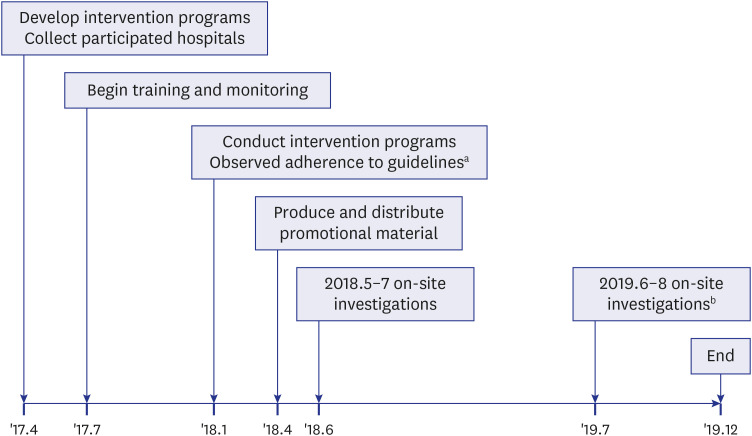
Intervention programs, including training, surveillance, and monitoring, were implemented. Data on the microorganisms responsible for CAUTIs, urinary catheter utilization ratio, rate of CAUTIs per 1,000 device days, and factors associated with the use of indwelling catheters were collected from 2017 to 2019. The incidence of CAUTIs and associated data were compared between university hospitals and small- and medium-sized hospitals.
Results
Thirty-two hospitals participated in the study, including 21 university hospitals and 11 small- and medium-sized hospitals. The microorganisms responsible for CAUTIs and their resistance rates did not differ between the two groups. In the first quarter of 2018, the incidence rate was 2.05 infections/1,000 device-days in university hospitals and 1.44 infections/1,000 device-days in small- and medium-sized hospitals. After implementing interventions, the rate gradually decreased in the first quarter of 2019, with 1.18 infections/1,000 device-days in university hospitals and 0.79 infections/1,000 device-days in small- and medium-sized hospitals. However, by the end of the study, the infection rate increased to 1.74 infections/1,000 device-days in university hospitals and 1.80 infections/1,000 device-days in small- and medium-sized hospitals.
Conclusion
We implemented interventions to prevent CAUTIs and evaluated their outcomes. The incidence of these infections decreased in the initial phases of the intervention when adequate support and personnel were present. The rate of these infections may be reduced by implementing active interventions such as consistent monitoring and adherence to guidelines for preventing infections.
Figure
Reference
-
1. Donlan RM. Biofilms and device-associated infections. Emerg Infect Dis. 2001; 7(2):277–281. PMID: 11294723.2. Saint S, Chenoweth CE. Biofilms and catheter-associated urinary tract infections. Infect Dis Clin North Am. 2003; 17(2):411–432. PMID: 12848477.3. Weber DJ, Sickbert-Bennett EE, Gould CV, Brown VM, Huslage K, Rutala WA. Incidence of catheter-associated and non-catheter-associated urinary tract infections in a healthcare system. Infect Control Hosp Epidemiol. 2011; 32(8):822–823. PMID: 21768769.4. World Health Organization. Report on the Burden of Endemic Health Care-Associated Infection Worldwide. Geneva, Switzerland: World Health Organization;2011.5. Nicolle LE, Gupta K, Bradley SF, Colgan R, DeMuri GP, Drekonja D, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the Infectious Diseases Society of America. Clin Infect Dis. 2019; 68(10):e83–110. PMID: 30895288.6. Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000; 28(1):68–75. PMID: 10679141.7. Platt R, Polk BF, Murdock B, Rosner B. Mortality associated with nosocomial urinary-tract infection. N Engl J Med. 1982; 307(11):637–642. PMID: 7110215.8. Tambyah PA, Knasinski V, Maki DG. The direct costs of nosocomial catheter-associated urinary tract infection in the era of managed care. Infect Control Hosp Epidemiol. 2002; 23(1):27–31. PMID: 11868889.9. Chant C, Smith OM, Marshall JC, Friedrich JO. Relationship of catheter-associated urinary tract infection to mortality and length of stay in critically ill patients: a systematic review and meta-analysis of observational studies. Crit Care Med. 2011; 39(5):1167–1173. PMID: 21242789.10. Fortin E, Rocher I, Frenette C, Tremblay C, Quach C. Healthcare-associated bloodstream infections secondary to a urinary focus: the Québec provincial surveillance results. Infect Control Hosp Epidemiol. 2012; 33(5):456–462. PMID: 22476271.11. Umscheid CA, Mitchell MD, Doshi JA, Agarwal R, Williams K, Brennan PJ. Estimating the proportion of healthcare-associated infections that are reasonably preventable and the related mortality and costs. Infect Control Hosp Epidemiol. 2011; 32(2):101–114. PMID: 21460463.12. Hooton TM, Bradley SF, Cardenas DD, Colgan R, Geerlings SE, Rice JC, et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010; 50(5):625–663. PMID: 20175247.13. Lo E, Nicolle LE, Coffin SE, Gould C, Maragakis LL, Meddings J, et al. Strategies to prevent catheter-associated urinary tract infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol. 2014; 35(5):464–479. PMID: 24709715.14. Gould CV, Umscheid CA, Agarwal RK, Kuntz G, Pegues DA. Healthcare Infection Control Practices Advisory Committee. Guideline for prevention of catheter-associated urinary tract infections 2009. Infect Control Hosp Epidemiol. 2010; 31(4):319–326. PMID: 20156062.15. Saint S, Greene MT, Krein SL, Rogers MA, Ratz D, Fowler KE, et al. A program to prevent catheter-associated urinary tract infection in acute care. N Engl J Med. 2016; 374(22):2111–2119. PMID: 27248619.16. Korea Disease Control and Prevention Agency. 2017 Korean National Healthcare-Associated Infections Surveillance System (KONIS) and Korean Society for Healthcare-associated Infection Control (KOSHIC) guideline. Updated 2017. Accessed December 16, 2023. https://www.kdca.go.kr/filepath/boardSyview.es?bid=0019&list_no=138061&seq=1 .17. Centers for Disease Control and Prevention. Urinary Tract Infection (Catheter-Associated Urinary Tract Infection [CAUTI] and Non-Catheter-Associated Urinary Tract Infection [UTI] and Other Urinary System Infection [USI]) Events. Atlanta, GA, USA: Centers for Disease Control and Prevention;2015.18. Saint S, Wiese J, Amory JK, Bernstein ML, Patel UD, Zemencuk JK, et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000; 109(6):476–480. PMID: 11042237.19. Park SH, Cho SY, Choi SH, Choi JY, Son HJ, Kim HB, et al. Applicability of New Indicators for Healthcare-associated Infections Surveillance in Korea. Korean J Healthc Assoc Infect Control Prev. 2022; 27(2):104–117.20. Kim HJ, Oh DK, Lim SY, Cho YJ, Park S, Suh GY, et al. Antibiogram of multidrug-resistant bacteria based on sepsis onset location in Korea: a multicenter cohort study. J Korean Med Sci. 2023; 38(10):e75. PMID: 36918029.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Catheter-associated Urinary Tract Infection
- Influences of Prevention Knowledge Regarding Catheter-associated Urinary Tract Infection (CAUTI), Workplace Learning, and Recognition of Infection Control Organization Culture on the Prevention Performance of CAUTI among Long-term Care Hospitals Nurses
- Incidence of Catheter-associated Urinary Tract Infection in Hospitals with Less than 300 Beds
- Management of urinary tract infection in geriatric hospital patients
- The Control of Catheter-associated Urinary Tract Infection: An Experimental Nursing Study: This study examined the effect of daily meatal care on the urinary tract infection rate of an experimental group