Anesth Pain Med.
2024 Apr;19(2):117-124. 10.17085/apm.23146.
Relationship between intraoperative requirement for anesthetics and postoperative analgesic consumption in laparoscopic colectomy: a randomized controlled double-blinded study
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Jeonbuk National University Medical School and Hospital, Jeonju, Korea
- KMID: 2555248
- DOI: http://doi.org/10.17085/apm.23146
Abstract
- Background
This study investigated the relationship between intraoperative requirement for an inhalational anesthetic (sevoflurane) or an opioid (remifentanil) and postoperative analgesic consumption.
Methods
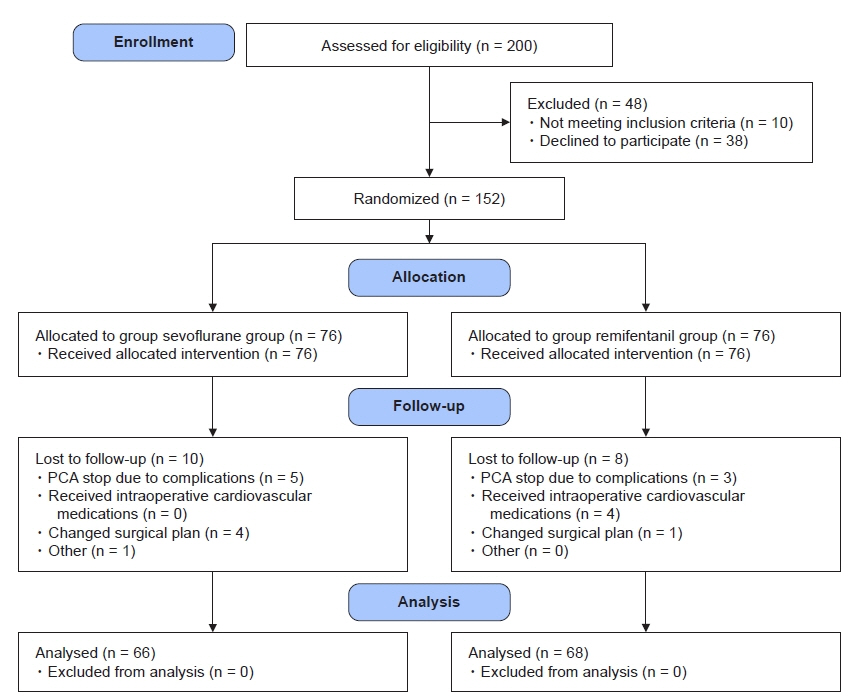
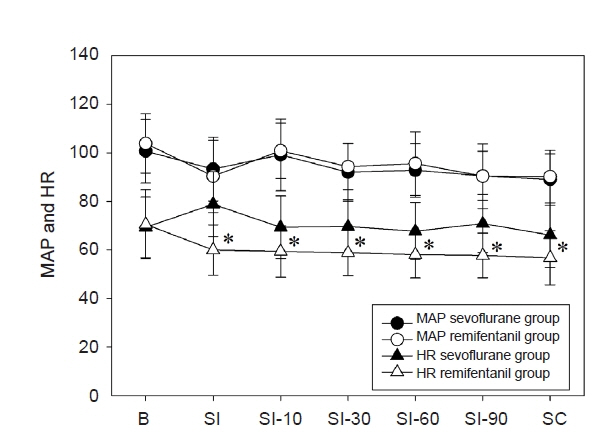
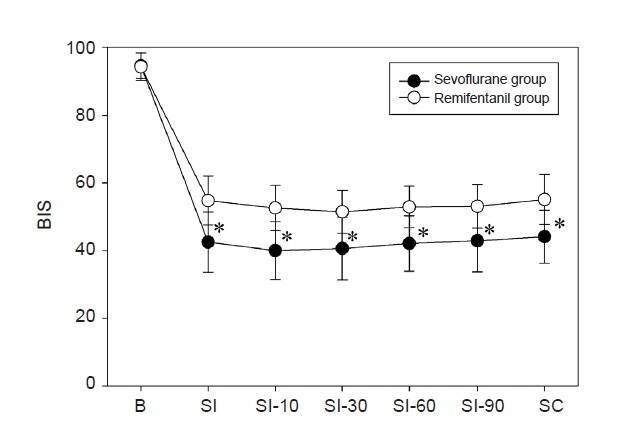
The study included 200 adult patients undergoing elective laparoscopic colectomy. In the sevoflurane group, the effect-site concentration of remifentanil was fixed at 1.0 ng/ml, while the inspiratory sevoflurane concentration was adjusted to maintain an appropriate anesthetic depth. In the remifentanil group, the end-expiratory sevoflurane concentration was fixed at 1.0 volume%, and the remifentanil concentration was adjusted. Pain scores and cumulative postoperative analgesic consumptions were evaluated at 2, 6, 24, and 48 h after surgery.
Results
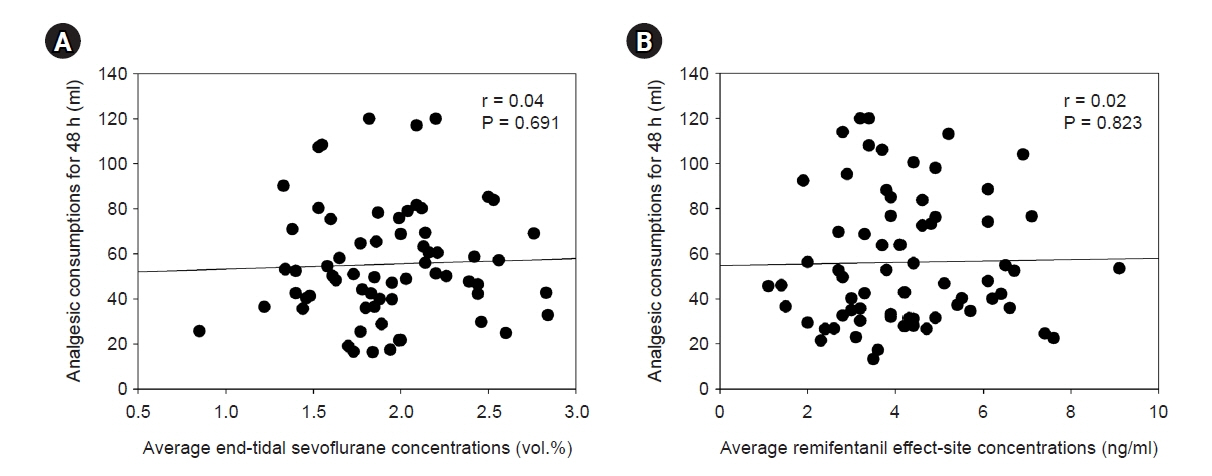
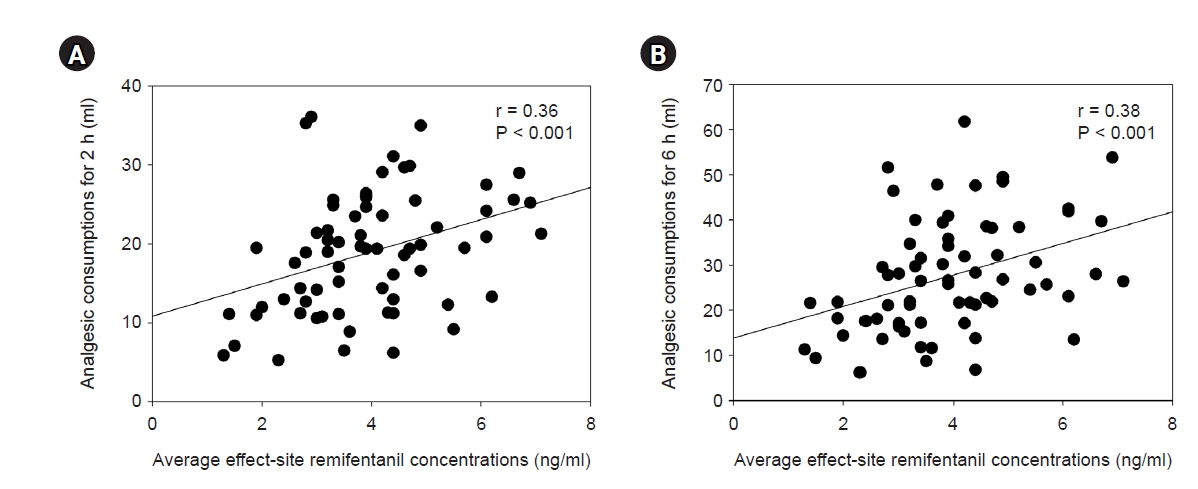
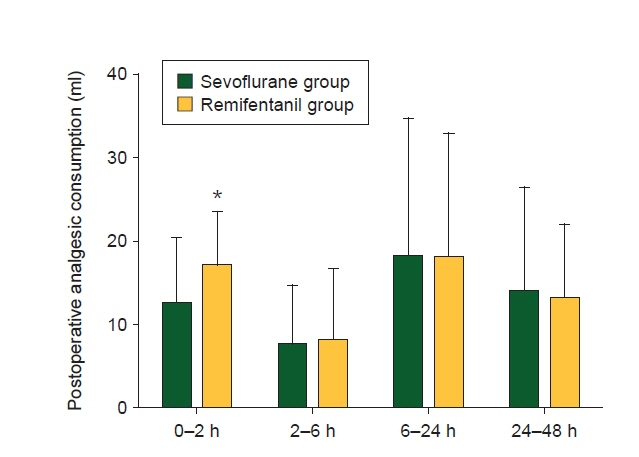
Average end-tidal concentration of sevoflurane and effect-site concentration of remifentanil were 2.0 ± 0.4 volume% and 3.9 ± 1.4 ng/ml in the sevoflurane and remifentanil groups, respectively. Cumulative postoperative analgesic consumption at 48 h postoperatively was 55 ± 26 ml in the sevoflurane group and 57 ± 33 ml in the remifentanil group. In the remifentanil group, the postoperative cumulative analgesic consumptions at 2 and 6 h were positively correlated with intraoperative remifentanil requirements (2 h: r = 0.36, P < 0.01; 6 h: r = 0.38, P < 0.01). However, there was no significant correlation in the sevoflurane group (r = 0.04, P = 0.69).
Conclusions
The amount of intraoperative requirement of short acting opioid, remifentanil, is correlated with postoperative analgesic consumption within postoperative 6 h. It may be contributed by the development of acute opioid tolerance. However, intraoperative sevoflurane requirement had no effect on postoperative analgesic consumption.
Keyword
Figure
Reference
-
1. Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017; 10:2287–98.
Article2. Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003; 97:534–40.
Article3. Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001; 87:62–72.
Article4. Tsui SL, Law S, Fok M, Lo JR, Ho E, Yang J, et al. Postoperative analgesia reduces mortality and morbidity after esophagectomy. Am J Surg. 1997; 173:472–8.
Article5. Li Y, Dong H, Tan S, Qian Y, Jin W. Effects of thoracic epidural anesthesia/analgesia on the stress response, pain relief, hospital stay, and treatment costs of patients with esophageal carcinoma undergoing thoracic surgery: A single-center, randomized controlled trial. Medicine (Baltimore). 2019; 98:e14362.6. Walder B, Schafer M, Henzi I, Tramer MR. Efficacy and safety of patient-controlled opioid analgesia for acute postoperative pain. A quantitative systematic review. Acta Anaesthesiol Scand. 2001; 45:795–804.
Article7. Bachiocco V, Morselli AM, Carli G. Self-control expectancy and postsurgical pain: relationships to previous pain, behavior in past pain, familial pain tolerance models, and personality. J Pain Symptom Manage. 1993; 8:205–14.
Article8. Maranets I, Kain ZN. Preoperative anxiety and intraoperative anesthetic requirements. Anesth Analg. 1999; 89:1346–51.
Article9. Rhudy JL, Meagher MW. Fear and anxiety: divergent effects on human pain thresholds. Pain. 2000; 84:65–75.
Article10. Vahabi S, Abaszadeh A, Yari F, Yousefi N. Postoperative pain, nausea and vomiting among pre- and postmenopausal women undergoing cystocele and rectocele repair surgery. Korean J Anesthesiol. 2015; 68:581–5.
Article11. Brown EN, Pavone KJ, Naranjo M. Multimodal general anesthesia: theory and practice. Anesth Analg. 2018; 127:1246–58.
Article12. Wang H, Cai Y, Liu J, Dong Y, Lai J. Pain sensitivity: a feasible way to predict the intensity of stress reaction caused by endotracheal intubation and skin incision? J Anesth. 2015; 29:904–11.
Article13. Kim D, Lim HS, Kim MJ, Jeong W, Ko S. High-dose intraoperative remifentanil infusion increases early postoperative analgesic consumption: a prospective, randomized, double-blind controlled study. J Anesth. 2018; 32:886–92.
Article14. Guignard B, Bossard AE, Coste C, Sessler DI, Lebrault C, Alfonsi P, et al. Acute opioid tolerance: intraoperative remifentanil increases postoperative pain and morphine requirement. Anesthesiology. 2000; 93:409–17.15. Chu LF, Angst MS, Clark D. Opioid-induced hyperalgesia in humans: molecular mechanisms and clinical considerations. Clin J Pain. 2008; 24:479–96.16. Colvin LA, Fallon MT. Opioid-induced hyperalgesia: a clinical challenge. Br J Anaesth. 2010; 104:125–7.
Article17. Sommer M, De Rijke JM, Van Kleef M, Kessels AG, Peters ML, Geurts JW, et al. Predictors of acute postoperative pain after elective surgery. Clin J Pain. 2010; 26:87–94.
Article18. Ip HYV, Abrishami A, Peng PWH, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009; 111:657–77.19. Lanitis S, Mimigianni C, Raptis D, Sourtse G, Sgourakis G, Karaliotas C. The impact of educational status on the postoperative perception of pain. Korean J Pain. 2015; 28:265–74.
Article20. Hayashida M, Nagashima M, Satoh Y, Katoh R, Tagami M, Ide S, et al. Analgesic requirements after major abdominal surgery are associated with OPRM1 gene polymorphism genotype and haplotype. Pharmacogenomics. 2008; 9:1605–16.
Article21. Kil HK, Kim WO, Chung WY, Kim GH, Seo H, Hong JY. Preoperative anxiety and pain sensitivity are independent predictors of propofol and sevoflurane requirements in general anaesthesia. Br J Anaesth. 2012; 108:119–25.
Article22. Ozalp G, Sarioglu R, Tuncel G, Aslan K, Kadiogullari N. Preoperative emotional states in patients with breast cancer and postoperative pain. Acta Anaesthesiol Scand. 2003; 47:26–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparing postoperative pain in various pressure pneumoperitoneum of laparoscopic cholecystectomy: a double-blind randomized controlled study
- Efficacy and Safety of Ramosetron Injection for Nausea and Vomiting in Colorectal-Cancer Patients Undergoing a Laparoscopic Colectomy: A Randomized, Double-Blind, Comparative Study
- The analgesic effect of nefopam combined with low dose remifentanil in patients undergoing middle ear surgery under desflurane anesthesia: a randomized controlled trial
- Ultrasound-guided anterior quadratus lumborum block for postoperative pain after percutaneous nephrolithotomy: a randomized controlled trial
- Effect of addition of buprenorphine or dexamethasone to levobupivacaine on postoperative analgesia in ultrasound guided transversus abdominis plane block in patients undergoing unilateral inguinal hernia repair: a prospective randomized double blind controlled trial