Anesth Pain Med.
2024 Apr;19(2):73-84. 10.17085/apm.24038.
Revolutionizing trauma care: advancing coagulation management and damage control anesthesia
- Affiliations
-
- 1Department of Anesthesiology and pain medicine, Dankook University Hospital, Cheonan, Korea
- KMID: 2555244
- DOI: http://doi.org/10.17085/apm.24038
Abstract
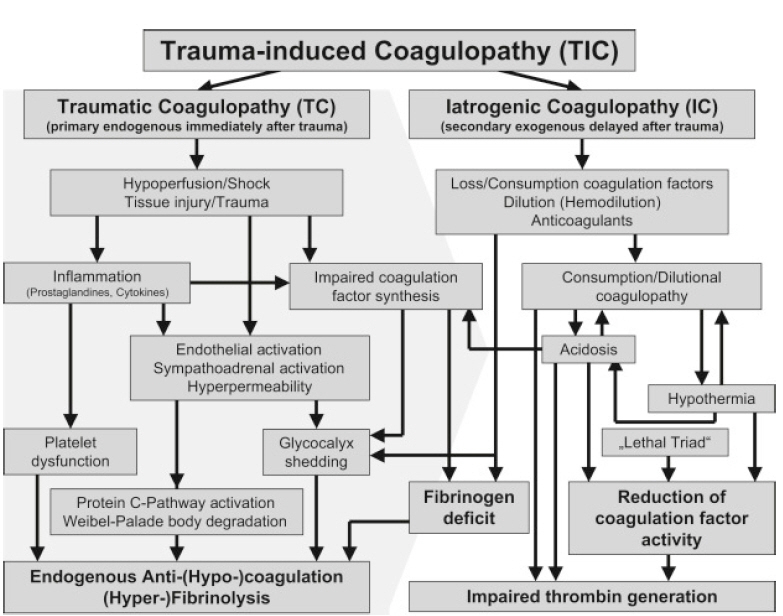
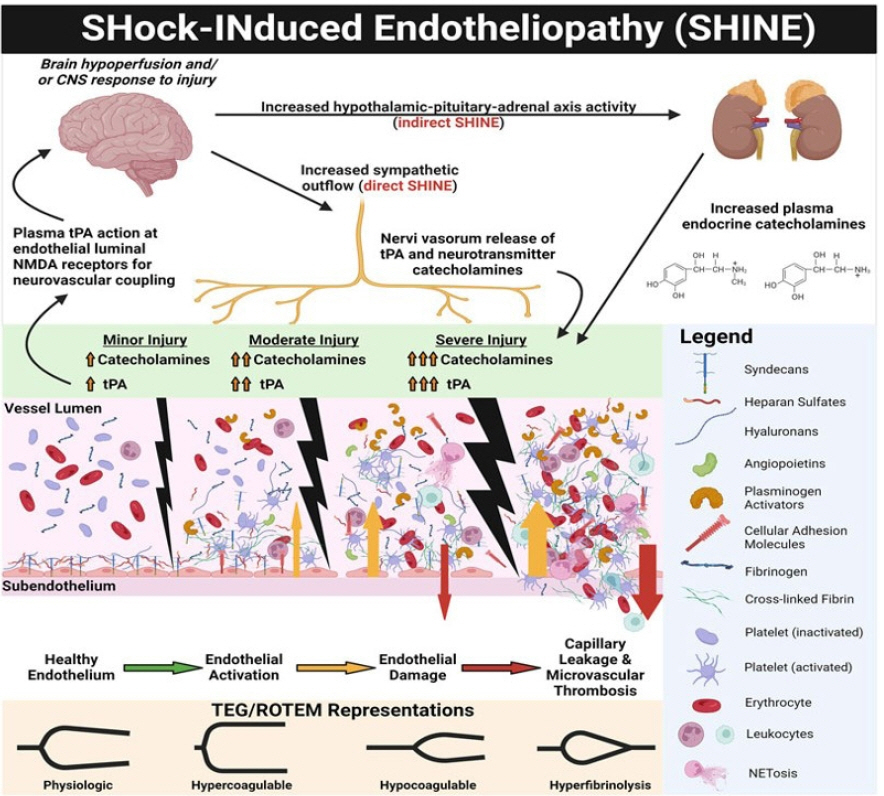
- Despite advances in emergency transfer systems and trauma medicine, the incidence of preventable deaths due to massive hemorrhage remains high. Recent immunological research has elucidated key mechanisms underlying trauma-induced coagulopathy in the early stages of trauma, including sympathoadrenal stimulation, shedding of the glycocalyx, and endotheliopathy. Consequently, the condition progresses to fibrinogen depletion, hyperfibrinolysis, and platelet dysfunction. Coexisting factors such as uncorrected acidosis, hypothermia, excessive crystalloid administration, and a history of anticoagulant use exacerbate coagulopathy. This study introduces damage-control anesthetic management based on recent insights into damage-control resuscitation, emphasizing the importance of rapid transport, timely bleeding control, early administration of antifibrinolytics and fibrinogen concentrates, and maintenance of calcium levels and body temperature. Additionally, this study discusses brain-protective strategies for trauma patients with brain injuries and the utilization of cartridge-based viscoelastic assays for goal-directed coagulation management in trauma settings. This comprehensive approach may provide potential insights for anesthetic management in the fast-paced field of trauma medicine.
Keyword
Figure
Reference
-
1. Lee S, Kim J, Lee J, Bae W. A community-based study of severe trauma, death, and disability, from 2015 to 2020. Public Health Weekly Report. 2023; 16:837–51.2. Moore EE, Moore HB, Kornblith LZ, Neal MD, Hoffman M, Mutch NJ, et al. Trauma-induced coagulopathy. Nat Rev Dis Primers. 2021; 7:30.
Article3. Jones DG, Nantais J, Rezende-Neto JB, Yazdani S, Vegas P, Rizoli S. Crystalloid resuscitation in trauma patients: deleterious effect of 5L or more in the first 24h. BMC Surg. 2018; 18:93.
Article4. Holzmacher JL, Reynolds C, Patel M, Maluso P, Holland S, Gamsky N, et al. Platelet transfusion does not improve outcomes in patients with brain injury on antiplatelet therapy. Brain Inj. 2018; 32:325–30.
Article5. Sugeir S, Grunstein I, Tobin JM. Damage Control Anesthesia. InL Damage Control in Trauma Care: An Evolving Comprehensive Team Approach. In : Duchesne J, Inaba K, Khan MA, editors. Cham: Springer International Publishing;2018. p. 193–207.6. Rossaint R, Afshari A, Bouillon B, Cerny V, Cimpoesu D, Curry N, et al. The European guideline on management of major bleeding and coagulopathy following trauma: sixth edition. Crit Care. 2023; 27:80.
Article7. Malgras B, Prunet B, Lesaffre X, Boddaert G, Travers S, Cungi PJ, et al. Damage control: Concept and implementation. J Visc Surg. 2017; 154 Suppl 1:S19–s29.
Article8. Oyeniyi BT, Fox EE, Scerbo M, Tomasek JS, Wade CE, Holcomb JB. Trends in 1029 trauma deaths at a level 1 trauma center: Impact of a bleeding control bundle of care. Injury. 2017; 48:5–12.
Article9. Yang Z, Le TD, Simovic MO, Liu B, Fraker TL, Cancio TS, et al. Traumatized triad of complementopathy, endotheliopathy, and coagulopathy ˗ Impact on clinical outcomes in severe polytrauma patients. Front Immunol. 2022; 13:991048.
Article10. Johansson PI, Henriksen HH, Stensballe J, Gybel-Brask M, Cardenas JC, Baer LA, et al. Traumatic endotheliopathy: a prospective observational study of 424 severely injured patients. Ann Surg. 2017; 265:597–603.11. Becker BF, Jacob M, Leipert S, Salmon AHJ, Chappell D. Degradation of the endothelial glycocalyx in clinical settings: searching for the sheddases. Br J Clin Pharmacol. 2015; 80:389–402.
Article12. Uchimido R, Schmidt EP, Shapiro NI. The glycocalyx: a novel diagnostic and therapeutic target in sepsis. Crit Care. 2019; 23:16.
Article13. Bunch CM, Chang E, Moore EE, Moore HB, Kwaan HC, Miller JB, et al. SHock-INduced Endotheliopathy (SHINE): A mechanistic justification for viscoelastography-guided resuscitation of traumatic and non-traumatic shock. Front Physiol. 2023; 14:1094845.
Article14. Bainbridge FJ, Sinha R, Tocchetti R, Clarke C, Martin D, Foo N, et al. Introduction of point-of-care ROTEM testing in the emergency department of an Australian level 1 trauma centre and its effect on blood product use. Emerg Med Australas. 2021; 33:893–9.15. Chignalia AZ, Yetimakman F, Christiaans SC, Unal S, Bayrakci B, Wagener BM, et al. The glycocalyx and trauma: a review. Shock. 2016; 45:338–48.16. Lin VS Sun E, Yau S, Abeyakoon C, Seamer G, Bhopal S, et al. Definitions of massive transfusion in adults with critical bleeding: a systematic review. Crit Care. 2023; 27:265.
Article17. Johansson PI, Stensballe J, Ostrowski SR. Shock induced endotheliopathy (SHINE) in acute critical illness - a unifying pathophysiologic mechanism. Crit Care. 2017; 21:25.
Article18. Patterson EK, Cepinskas G, Fraser DD. Endothelial glycocalyx degradation in critical illness and injury. Front Med (Lausanne). 2022; 9:898592.
Article19. Engström M, Schött U, Romner B, Reinstrup P. Acidosis impairs the coagulation: A thromboelastographic study. J Trauma. 2006; 61:624–8.
Article20. Lester ELW, Fox EE, Holcomb LB, Brasel KJ, Bulger EM, Cohen MJ, et al. The impact of hypothermia on outcomes in massively transfused patients. J Trauma Acute Care Surg. 2019; 86:458–63.
Article21. Chen X, Shi S, Hu L. High levels of D-dimer are associated with poor hospitalization outcome of spontaneous intraparenchymal haemorrhage. Neuropsychiatr Dis Treat. 2022; 18:1079–86.
Article22. Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015; 313:471–82.23. Hayakawa M. Dynamics of fibrinogen in acute phases of trauma. J Intensive Care. 2017; 5:3.
Article24. Lang T, Johanning K, Metzler H, Piepenbrock S, Solomon C, Rahe-Meyer N, et al. The effects of fibrinogen levels on thromboelastometric variables in the presence of thrombocytopenia. Anesth Analg. 2009; 108:751–8.
Article25. Heo Y, Chang SW, Lee SW, Ma DS, Kim DH. Hemostatic effect of fibrinogen concentrate on traumatic massive hemorrhage: a propensity score matching study. Trauma Surg Acute Care Open. 2024; 9:e001271.
Article26. Innerhofer P, Fries D, Mittermayr M, Innerhofer N, Von Langen D, Hell T, et al. Reversal of trauma-induced coagulopathy using first-line coagulation factor concentrates or fresh frozen plasma (RETIC): a single-centre, parallel-group, open-label, randomised trial. Lancet Haematol. 2017; 4:e258–71.
Article27. Tauber H, Innerhofer N, Von Langen D, Ströhle M, Fries D, Mittermayr M, et al. Dynamics of platelet counts in major trauma: the impact of haemostatic resuscitation and effects of platelet transfusion-a sub-study of the randomized controlled RETIC trial. J Clin Med. 2020; 9:2420.
Article28. CRASH-2 trial collaborators 1, Shakur H, Roberts I, Bautista R, Caballero J, Coats T, Dewan T, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010; 376:23–32.
Article29. CRASH-3 trial collaborators. Effects of tranexamic acid on death, disability, vascular occlusive events and other morbidities in patients with acute traumatic brain injury (CRASH-3): a randomised, placebo-controlled trial. Lancet. 2019; 394:1713–23.30. Dixon AL, McCully BH, Rick EA, Dewey E, Farrell DH, Morrison LJ, et al. Tranexamic acid administration in the field does not affect admission thromboelastography after traumatic brain injury. J Trauma Acute Care Surg. 2020; 89:900–7.
Article31. Moore HB, Moore EE, Gonzalez E, Chapman MP, Chin TL, Silliman CC, et al. Hyperfibrinolysis, physiologic fibrinolysis, and fibrinolysis shutdown: the spectrum of postinjury fibrinolysis and relevance to antifibrinolytic therapy. J Trauma Acute Care Surg. 2014; 77:811–7; discussion 817.32. Raza I, Davenport R, Rourke C, Platton S, Manson J, Spoors C, et al. The incidence and magnitude of fibrinolytic activation in trauma patients. J Thromb Haemost. 2013; 11:307–14.33. Cardenas JC, Wade CE, Cotton BA, George MJ, Holcomb JB, Schreiber MA, et al. TEG lysis shutdown represents coagulopathy in bleeding trauma patients: analysis of the PROPPR cohort. Shock. 2019; 51:273–83.
Article34. Peralta R, Vijay A, El-Menyar A, Consunji R, Afifi I, Mahmood I, et al. Early high ratio platelet transfusion in trauma resuscitation and its outcomes. Int J Crit Illn Inj Sci. 2016; 6:188–93.35. Gratz J, Güting H, Thorn S, Brazinova A, Görlinger K, Schäfer N, et al. Protocolised thromboelastometric-guided haemostatic management in patients with traumatic brain injury: a pilot study. Anaesthesia. 2019; 74:883–90.
Article36. Kornblith LZ, Decker A, Conroy AS, Hendrickson CM, Fields AT, Robles AJ, et al. It's about time: transfusion effects on postinjury platelet aggregation over time. J Trauma Acute Care Surg. 2019; 87:1042–51.
Article37. DeBot M, Sauaia A, Schaid T, Moore EE. Trauma-induced hypocalcemia. Transfusion. 2022; 62 Suppl 1:S274–80.
Article38. Carson JL, Stanworth SJ, Dennis JA, Trivella M, Roubinian N, Fergusson DA, et al. Transfusion thresholds for guiding red blood cell transfusion. Cochrane Database Syst Rev. 2021; 12:CD002042.
Article39. Robertson CS, Hannay HJ, Yamal JM, Gopinath S, Goodman JC, Tilley BC, et al. Effect of erythropoietin and transfusion threshold on neurological recovery after traumatic brain injury: a randomized clinical trial. JAMA. 2014; 312:36–47.
Article40. Chen H, Wu F, Yang P, Shao J, Chen Q, Zheng R. A meta-analysis of the effects of therapeutic hypothermia in adult patients with traumatic brain injury. Crit Care. 2019; 23:396.
Article41. Lou X, Lu G, Zhao M, Jin P. Preoperative fluid management in traumatic shock: A retrospective study for identifying optimal therapy of fluid resuscitation for aged patients. Medicine (Baltimore). 2018; 97:e9966.42. Singer M, Young PJ, Laffey JG, Asfar P, Taccone FS, Skrifvars MB, et al. Dangers of hyperoxia. Crit Care. 2021; 25:440.43. Chen ST, Min S. Oxygen reserve index, a new method of monitoring oxygenation status: what do we need to know? Chin Med J (Engl). 2020; 133:229–34.
Article44. Lou X, Lu G, Zhao M, Jin P. Preoperative fluid management in traumatic shock: A retrospective study for identifying optimal therapy of fluid resuscitation for aged patients. Medicine (Baltimore). 2018; 97:e9966.45. Gamal M, Abdelhamid B, Zakaria D, Dayem OAE, Rady A, Fawzy M, et al. Evaluation of noninvasive hemoglobin monitoring in trauma patients with low hemoglobin levels. Shock. 2018; 49:150–3.
Article46. Geerts WH, Code KI, Jay RM, Chen E, Szalai JP. A prospective study of venous thromboembolism after major trauma. N Engl J Med. 1994; 331:1601–6.
Article47. Maegele M, Gu ZT, Huang QB, Yang H. Updated concepts on the pathophysiology and the clinical management of trauma hemorrhage and coagulopathy. Chin J Traumatol. 2017; 20:125–32.