Korean J Pain.
2024 Apr;37(2):164-177. 10.3344/kjp.23301.
Effect of pain on cranio-cervico-mandibular function and postural stability in people with temporomandibular joint disorders
- Affiliations
-
- 1Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, Cyprus International University, Lefkoşa, Turkiye
- 2Department of Physiotherapy and Rehabilitation, Faculty of Health Sciences, Eastern Mediterranean University, Famagusta, Turkiye
- KMID: 2554956
- DOI: http://doi.org/10.3344/kjp.23301
Abstract
- Background
Neck and jaw pain is common and is associated with jaw functional limitations, postural stability, muscular endurance, and proprioception. This study aimed to investigate the effect of jaw and neck pain on craniocervico- mandibular functions and postural stability in patients with temporomandibular joint disorders (TMJDs).
Methods
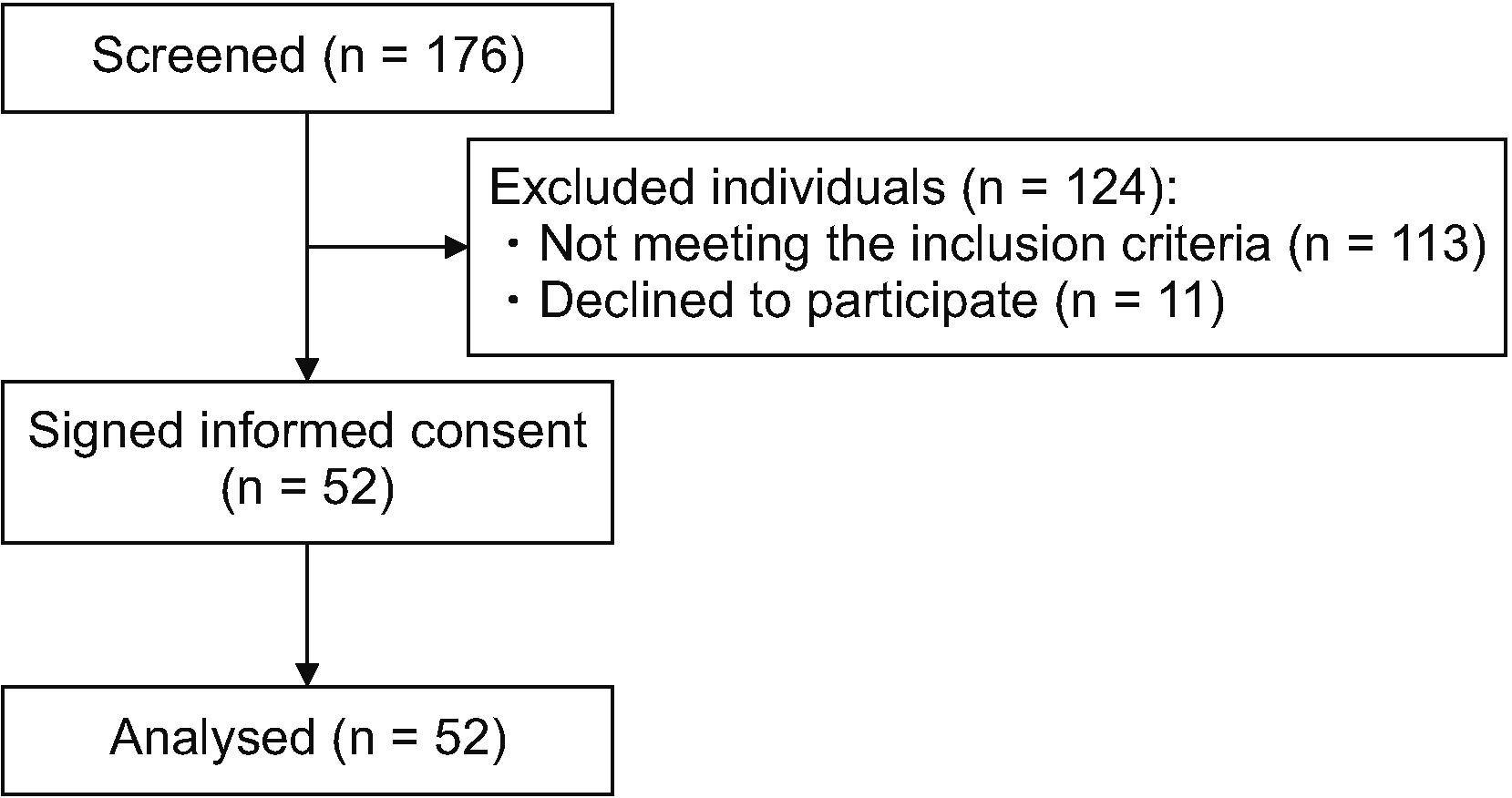
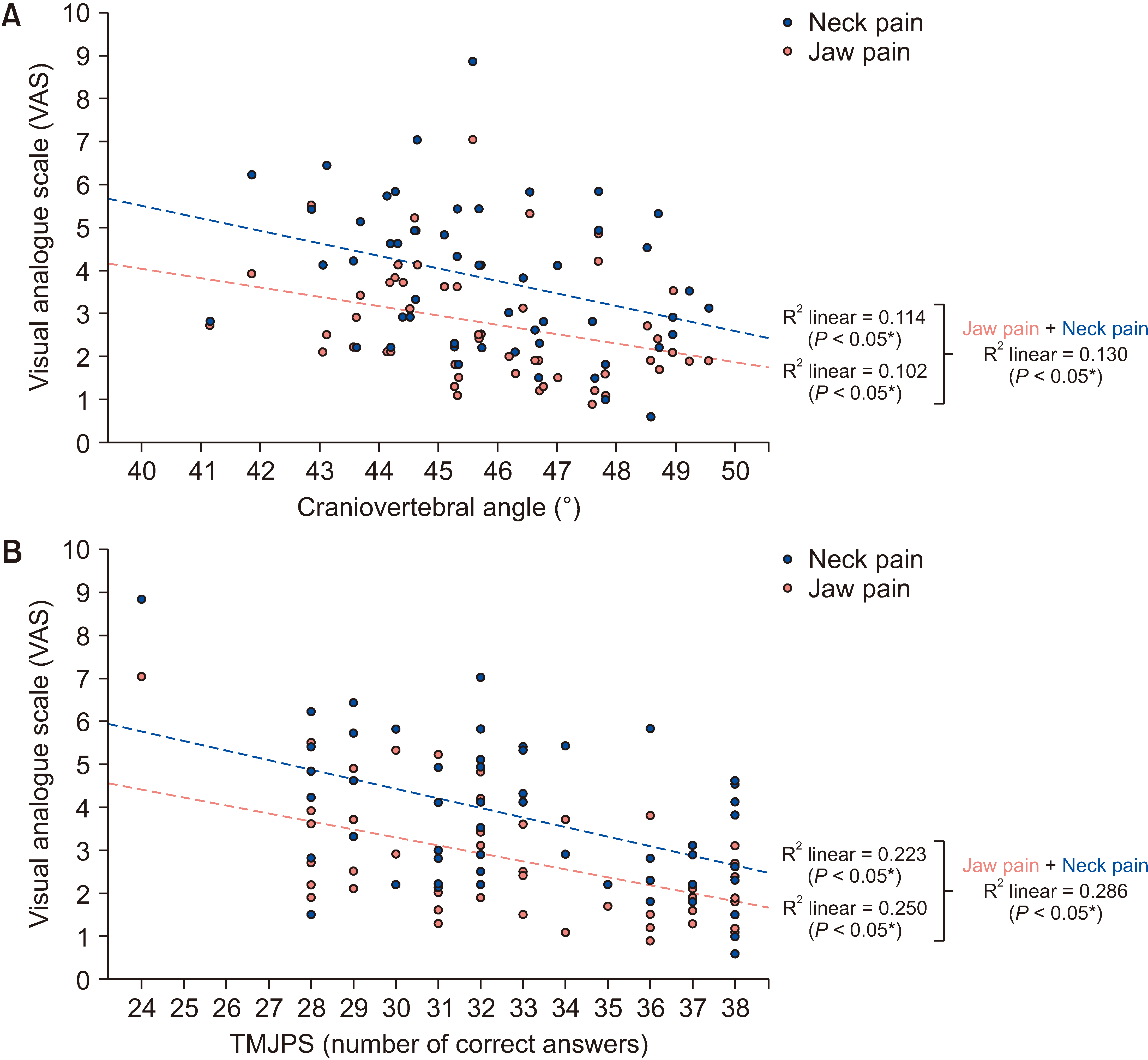
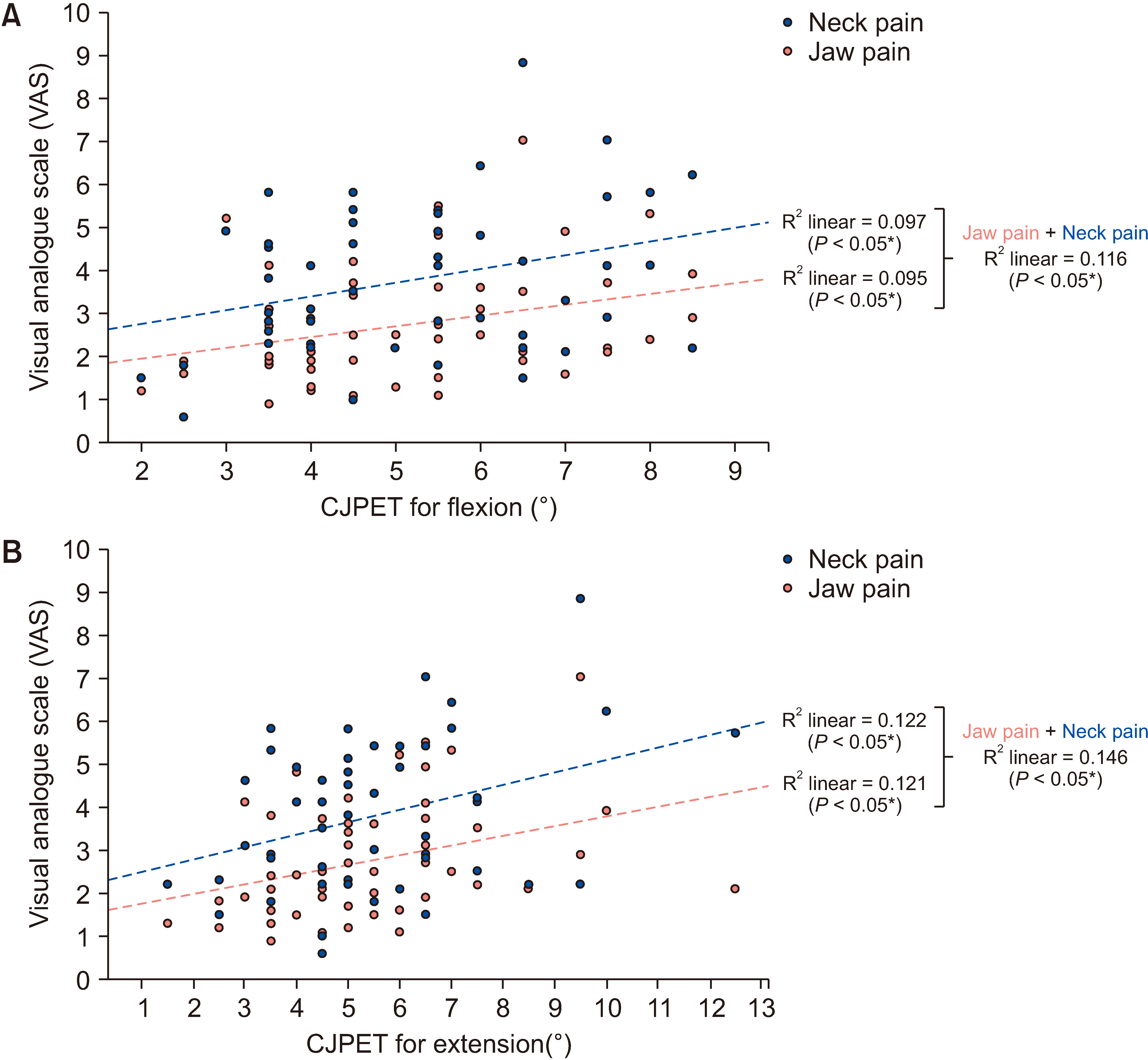
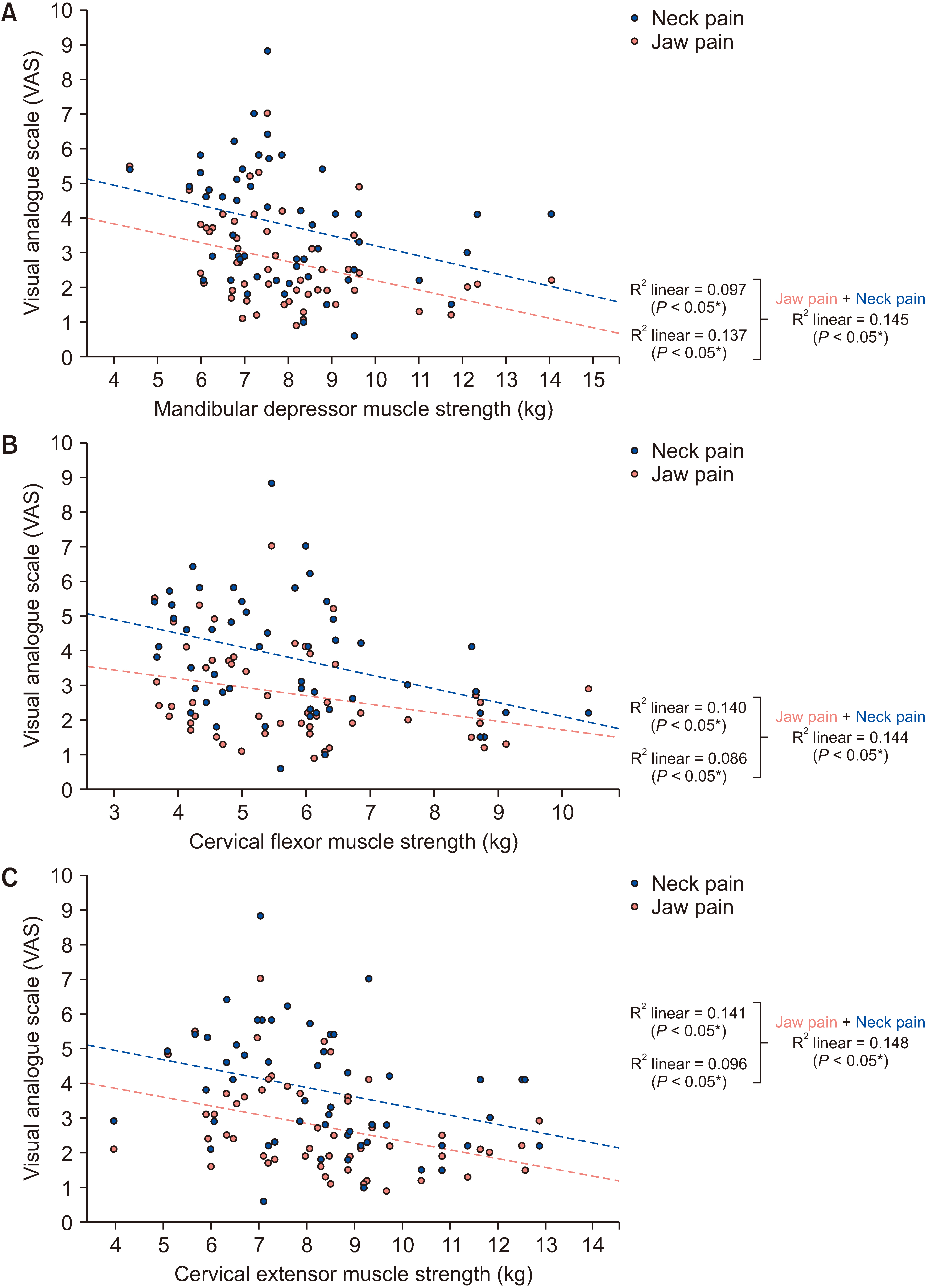
Fifty-two patients with TMJDs were included and assessed using Fonseca's Questionnaire and the Helkimo Clinical Dysfunction Index. An isometric strength test was performed for the TMJ depressor and cervical muscles. The TMJ position sense (TMJPS) test and cervical joint position error test (CJPET) were employed for proprioception. Total sway degree was obtained for the assessment of postural stability. Deep neck flexor endurance (DNFE) was assessed using the craniocervical flexion test. The mandibular function impairment questionnaire (MFIQ) was employed to assess mandibular function, and the craniovertebral angle (CVA) was measured for forward head posture.
Results
Jaw and neck pain negatively affected CVA (R2 = 0.130), TMJPS (R2 = 0.286), DNFE (R2 = 0.355), TMJ depressor (R2 = 0.145), cervical flexor (R2 = 0.144), and extensor (R2 = 0.148) muscle strength. Jaw and neck pain also positively affected CJPET for flexion (R2 = 0.116) and extension (R2 = 0.146), as well as total sway degree (R2 = 0.128) and MFIQ (R2 = 0.230).
Conclusions
Patients with painful TMJDs, could have impaired muscle strength and proprioception of the TMJ and cervical region. The jaw and neck pain could also affect postural stability, and the endurance of deep neck flexors as well as mandibular functions in TMJDs.
Keyword
Figure
Reference
-
1. Tantawy SA, Abdul Rahman A, Abdul Ameer M. 2017; The relationship between the development of musculoskeletal disorders, body mass index, and academic stress in Bahraini University students. Korean J Pain. 30:126–33. DOI: 10.3344/kjp.2017.30.2.126. PMID: 28416996. PMCID: PMC5392656.
Article2. Camparis CM, Formigoni G, Teixeira MJ, Bittencourt LR, Tufik S, de Siqueira JT. 2006; Sleep bruxism and temporomandibular disorder: clinical and polysomnographic evaluation. Arch Oral Biol. 51:721–8. DOI: 10.1016/j.archoralbio.2006.03.002. PMID: 16584706.
Article3. Kazeminasab S, Nejadghaderi SA, Amiri P, Pourfathi H, Araj-Khodaei M, Sullman MJM, et al. 2022; Neck pain: global epidemiology, trends and risk factors. BMC Musculoskelet Disord. 23:26. DOI: 10.1186/s12891-021-04957-4. PMID: 34980079. PMCID: PMC8725362.
Article4. Valesan LF, Da-Cas CD, Réus JC, Denardin ACS, Garanhani RR, Bonotto D, et al. 2021; Prevalence of temporomandibular joint disorders: a systematic review and meta-analysis. Clin Oral Investig. 25:441–53. DOI: 10.1007/s00784-020-03710-w. PMID: 33409693.
Article5. Isong U, Gansky SA, Plesh O. 2008; Temporomandibular joint and muscle disorder-type pain in U.S. adults: the National Health Interview Survey. J Orofac Pain. 22:317–22.6. Dominick CH, Blyth FM, Nicholas MK. 2012; Unpacking the burden: understanding the relationships between chronic pain and comorbidity in the general population. Pain. 153:293–304. DOI: 10.1016/j.pain.2011.09.018. PMID: 22071318.
Article7. Dinsdale A, Liang Z, Thomas L, Treleaven J. 2020; Are jaw range of motion, muscle function and proprioception impaired in adults with persistent temporomandibular disorders? A systematic review and meta-analysis. J Oral Rehabil. 47:1448–78. DOI: 10.1111/joor.13090. PMID: 32896911.
Article8. Madhan S, Nascimento GG, Ingerslev J, Cornelis M, Pinholt EM, Cattaneo PM, et al. 2023; Associations between temporomandibular disorders, pain, jaw and masticatory function in dentofacial deformity patients: a cross-sectional study. J Oral Rehabil. 50:746–57. DOI: 10.1111/joor.13483. PMID: 37119394.
Article9. Knapstad MK, Goplen FK, Ask T, Skouen JS, Nordahl SHG. 2019; Associations between pressure pain threshold in the neck and postural control in patients with dizziness or neck pain - a cross-sectional study. BMC Musculoskelet Disord. 20:528. DOI: 10.1186/s12891-019-2922-4. PMID: 31707980. PMCID: PMC6844061.
Article10. Minervini G, Franco R, Marrapodi MM, Crimi S, Badnjević A, Cervino G, et al. 2023; Correlation between temporomandibular disorders (TMD) and posture evaluated trough the diagnostic criteria for temporomandibular disorders (DC/TMD): a systematic review with meta-analysis. J Clin Med. 12:2652. DOI: 10.3390/jcm12072652. PMID: 37048735. PMCID: PMC10095000.
Article11. Ciancaglini R, Testa M, Radaelli G. 1999; Association of neck pain with symptoms of temporomandibular dysfunction in the general adult population. Scand J Rehabil Med. 31:17–22. DOI: 10.1080/003655099444687. PMID: 10229999.
Article12. Moustafa IM, Youssef A, Ahbouch A, Tamim M, Harrison DE. 2020; Is forward head posture relevant to autonomic nervous system function and cervical sensorimotor control? Cross sectional study. Gait Posture. 77:29–35. DOI: 10.1016/j.gaitpost.2020.01.004. PMID: 31955048.
Article13. Pérez Rojas AA. 2015. Prevalence of craniocervical posture alterations in patients with class II skeletal relationship [Doctoral dissertation]. National University of San Marcos;Lima:14. Mahmoud NF, Hassan KA, Abdelmajeed SF, Moustafa IM, Silva AG. 2019; The relationship between forward head posture and neck pain: a systematic review and meta-analysis. Curr Rev Musculoskelet Med. 12:562–77. DOI: 10.1007/s12178-019-09594-y. PMID: 31773477. PMCID: PMC6942109.
Article15. Yoo WG, Kim MH. 2010; Effect of different seat support characteristics on the neck and trunk muscles and forward head posture of visual display terminal workers. Work. 36:3–8. DOI: 10.3233/WOR-2010-1002. PMID: 20555171.
Article16. Alghadir AH, Zafar H, Iqbal ZA. 2015; Effect of three different jaw positions on postural stability during standing. Funct Neurol. 30:53–7.17. Zafar H, Alghadir AH, Iqbal ZA. 2017; Effect of different head-neck-jaw postures on cervicocephalic kinesthetic sense. J Musculoskelet Neuronal Interact. 17:341–6.18. Zafar H, Nordh E, Eriksson PO. 2000; Temporal coordination between mandibular and head-neck movements during jaw opening-closing tasks in man. Arch Oral Biol. 45:675–82. DOI: 10.1016/S0003-9969(00)00032-7. PMID: 10869479.
Article19. Dahlström L, Haraldson T, Carlsson GE. 1989; Perception of jaw position during different conditions. J Craniomandib Disord. 3:147–51.20. Monteiro AA, Clark GT, Pullinger AG. 1987; Relationship between mandibular movement accuracy and masticatory dysfunction symptoms. J Craniomandib Disord. 1:237–42.21. van den Berghe L, de Boever JA, Broekhuijsen ML, van Willigen JD. 1987; On the perception of the preferred jaw position in patients with symptoms of temporomandibular disorders. Cranio. 5:344–50. DOI: 10.1080/08869634.1987.11678209. PMID: 3482170.
Article22. Guarda-Nardini L, Piccotti F, Mogno G, Favero L, Manfredini D. 2012; Age-related differences in temporomandibular disorder diagnoses. Cranio. 30:103–9. DOI: 10.1179/crn.2012.015. PMID: 22606853.
Article23. Alonso-Royo R, Sánchez-Torrelo CM, Ibáñez-Vera AJ, Zagalaz-Anula N, Castellote-Caballero Y, Obrero-Gaitán E, et al. 2021; Validity and reliability of the Helkimo clinical dysfunction index for the diagnosis of temporomandibular disorders. Diagnostics (Basel). 11:472. DOI: 10.3390/diagnostics11030472. PMID: 33800185. PMCID: PMC8000811.
Article24. Berni KC, Dibai-Filho AV, Rodrigues-Bigaton D. 2015; Accuracy of the Fonseca anamnestic index in the identification of myogenous temporomandibular disorder in female community cases. J Bodyw Mov Ther. 19:404–9. DOI: 10.1016/j.jbmt.2014.08.001. PMID: 26118509.
Article25. Kaynak BA, Tas S, Salkın Y. 2023; The accuracy and reliability of the Turkish version of the Fonseca anamnestic index in temporomandibular disorders. Cranio. 41:78–83. DOI: 10.1080/08869634.2020.1812808. PMID: 32840464.
Article26. Ara T, Iizuka H, Sorimachi Y, Iizuka Y, Nakajima T, Nishinome M, et al. 2010; Evaluation of neck pain by using a visual analog scale before and after laminoplasty in patients with cervical myelopathy: relationship with clinical results. J Neurosurg Spine. 12:635–40. DOI: 10.3171/2009.12.SPINE09181. PMID: 20515349.
Article27. Suvarnnato T, Puntumetakul R, Uthaikhup S, Boucaut R. 2019; Effect of specific deep cervical muscle exercises on functional disability, pain intensity, craniovertebral angle, and neck-muscle strength in chronic mechanical neck pain: a randomized controlled trial. J Pain Res. 12:915–25. DOI: 10.2147/JPR.S190125. PMID: 30881101. PMCID: PMC6411318.28. Bucci R, Lobbezoo F, Michelotti A, Orfanou C, Koutris M. 2017; Delayed-onset muscle soreness does not influence occlusal sensitivity and position sense of the mandible. J Oral Rehabil. 44:655–63. DOI: 10.1111/joor.12528. PMID: 28548304.
Article29. Clark GT, Jacobson R, Beemsterboer PL. 1984; Interdental thickness discrimination in myofascial pain dysfunction subjects. J Oral Rehabil. 11:381–6. DOI: 10.1111/j.1365-2842.1984.tb00589.x. PMID: 6589383.
Article30. Koseoglu A, Coskunsu DK, Mutlu EK. 2022; Validity and reliability of a new method to measure cervical proprioception. Phys Med Rehab Kuror. 32:306–13. DOI: 10.1055/a-1761-5962.31. Abdelkader NA, Mahmoud AY, Fayaz NA, Saad El-Din Mahmoud L. 2020; Decreased neck proprioception and postural stability after induced cervical flexor muscles fatigue. J Musculoskelet Neuronal Interact. 20:421–8.32. Iida T, Tohara H, Wada S, Nakane A, Sanpei R, Ueda K. 2013; Aging decreases the strength of suprahyoid muscles involved in swallowing movements. Tohoku J Exp Med. 231:223–8. DOI: 10.1620/tjem.231.223. PMID: 24240663.
Article33. Florencio LL, de Oliveira AS, Carvalho GF, Tolentino Gde A, Dach F, Bigal ME, et al. 2015; Cervical muscle strength and muscle coactivation during isometric contractions in patients with migraine: a cross-sectional study. Headache. 55:1312–22. DOI: 10.1111/head.12644. PMID: 26388193.
Article34. Eris F, Uzun R, Hazir A, Güvenc C. 2023; Comparison of some anthropometric features and balance ability of basketball and volleyball athletes. Eur J Mol Clin Med. 10:1–8.35. James G, Doe T. 2010; The craniocervical flexion test: intra-tester reliability in asymptomatic subjects. Physiother Res Int. 15:144–9. DOI: 10.1002/pri.456. PMID: 20146239.
Article36. Yıldız NT, Alkan A, Külünkoğlu BA. 2024; Validity and reliability of the Turkish version of mandibular function impairment questionnaire. Cranio. 42:160–70. DOI: 10.1080/08869634.2021.2004715. PMID: 34789075.
Article37. Walczyńska-Dragon K, Baron S, Nitecka-Buchta A, Tkacz E. 2014; Correlation between TMD and cervical spine pain and mobility: is the whole body balance TMJ related? Biomed Res Int. 2014:582414. DOI: 10.1155/2014/582414. PMID: 25050363. PMCID: PMC4090505.
Article38. Maini K, Dua A. 2024. Temporomandibular syndrome. StatPearls Publishing.39. Ries LG, Bérzin F. 2008; Analysis of the postural stability in individuals with or without signs and symptoms of temporomandibular disorder. Braz Oral Res. 22:378–83. DOI: 10.1590/S1806-83242008000400016. PMID: 19148396.
Article40. Armijo-Olivo S, Silvestre RA, Fuentes JP, da Costa BR, Major PW, Warren S, et al. 2012; Patients with temporomandibular disorders have increased fatigability of the cervical extensor muscles. Clin J Pain. 28:55–64. DOI: 10.1097/AJP.0b013e31822019f2. PMID: 21677569.
Article41. Goiato MC, Zuim PRJ, Moreno A, Dos Santos DM, da Silva EVF, de Caxias FP, et al. 2017; Does pain in the masseter and anterior temporal muscles influence maximal bite force? Arch Oral Biol. 83:1–6. DOI: 10.1016/j.archoralbio.2017.06.029. PMID: 28688272.
Article42. Armijo-Olivo S, Fuentes JP, da Costa BR, Major PW, Warren S, Thie NM, et al. 2010; Reduced endurance of the cervical flexor muscles in patients with concurrent temporomandibular disorders and neck disability. Man Ther. 15:586–92. DOI: 10.1016/j.math.2010.07.001. PMID: 20688556.
Article43. Manfredini D, Castroflorio T, Perinetti G, Guarda-Nardini L. 2012; Dental occlusion, body posture and temporomandibular disorders: where we are now and where we are heading for. J Oral Rehabil. 39:463–71. DOI: 10.1111/j.1365-2842.2012.02291.x. PMID: 22435603.
Article44. Treleaven J. 2008; Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 13:2–11. DOI: 10.1016/j.math.2007.06.003. PMID: 17702636.
Article45. Kim JY, Yeo SS. 2022; Change of balance ability in subjects with pain-related temporomandibular disorders. J Kor Phys Ther. 34:321–5. DOI: 10.18857/jkpt.2022.34.6.321.
Article46. Sforza C, Tartaglia GM, Solimene U, Morgun V, Kaspranskiy RR, Ferrario VF. 2006; Occlusion, sternocleidomastoid muscle activity, and body sway: a pilot study in male astronauts. Cranio. 24:43–9. DOI: 10.1179/crn.2006.008. PMID: 16541845.
Article47. Ishii H. 1990; [A study on the relationships between imbalance of stomatognathic function and asymmetry of craniofacial morphology, and the center of gravity of the upright posture]. Osaka Daigaku Shigaku Zasshi. 35:517–56. Japanese.48. Wang H, Ji Z, Jiang G, Liu W, Jiao X. 2016; Correlation among proprioception, muscle strength, and balance. J Phys Ther Sci. 28:3468–72. DOI: 10.1589/jpts.28.3468. PMID: 28174475. PMCID: PMC5276784.
Article49. Pedroni CR, de Oliveira AS, Bérzin F. 2006; Pain characteristics of temporomandibular disorder: a pilot study in patients with cervical spine dysfunction. J Appl Oral Sci. 14:388–92. DOI: 10.1590/S1678-77572006000500016. PMID: 19089063. PMCID: PMC4327233.
Article50. Walczyńska-Dragon K, Baron S. 2011; The biomechanical and functional relationship between temporomandibular dysfunction and cervical spine pain. Acta Bioeng Biomech. 13:93–8.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Study for Treatment fo Temporo-mandibular Joint Pain
- A study on simultation of the mandibular movement of the patients with temporomandibular joint disorder
- Treatment of Temporomandibular Joint Disorder by Alloplastic Total Temporomandibular Joint Replacement
- Mischievous mandibular third molars camouflaging temporomandibular joint disorders
- Application of botulinum toxin in maxillofacial field: Part II. Wrinkle, intraoral ulcer, and cranio-maxillofacial pain