Korean J Pain.
2024 Apr;37(2):132-140. 10.3344/kjp.23292.
New insight into the vasto-adductor membrane for safer adductor canal blockade
- Affiliations
-
- 1Department of Anatomy, Wonkwang University School of Medicine, Iksan, Korea
- 2Jesaeng-Euise Clinical Anatomy Center, Wonkwang University School of Medicine, Iksan, Korea
- 3Sarcopenia Total Solution Center, Wonkwang University School of Medicine, Iksan, Korea
- 4Department of Anesthesiology and Pain Medicine, Wonkwang University School of Medicine, Wonkwang University Hospital, Iksan, Korea
- KMID: 2554953
- DOI: http://doi.org/10.3344/kjp.23292
Abstract
- Background
This study aimed to identify exact anatomical landmarks and ideal injection volumes for safe adductor canal blocks (ACB).
Methods
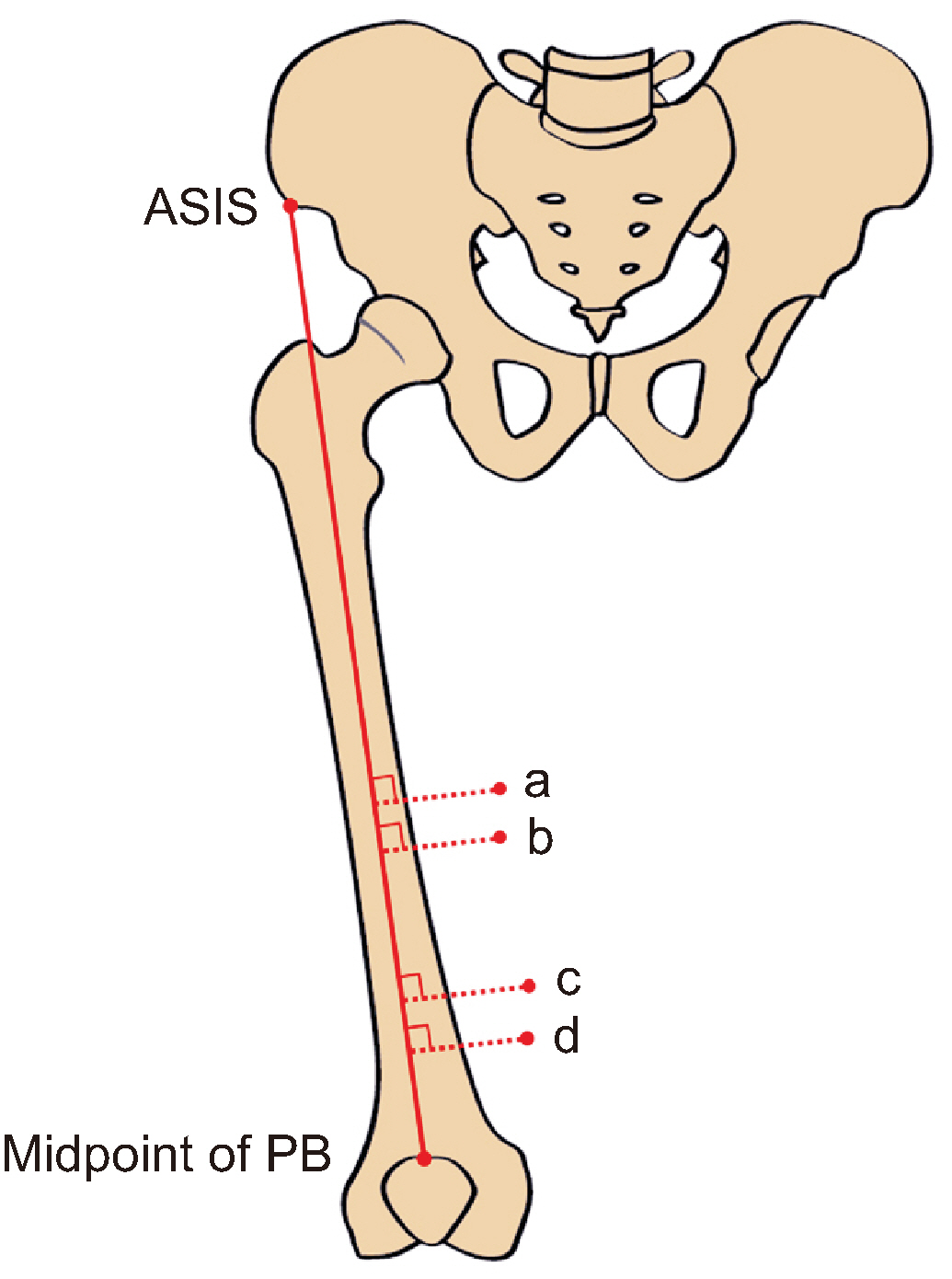
Fifty thighs from 25 embalmed adult Korean cadavers were used. The measurement baseline was the line connecting the anterior superior iliac spine (ASIS) to the midpoint of the patellar base. All target points were measured perpendicular to the baseline. The relevant cadaveric structures were observed using ultrasound (US) and confirmed in living individuals. US-guided dye injection was performed to determine the ideal volume.
Results
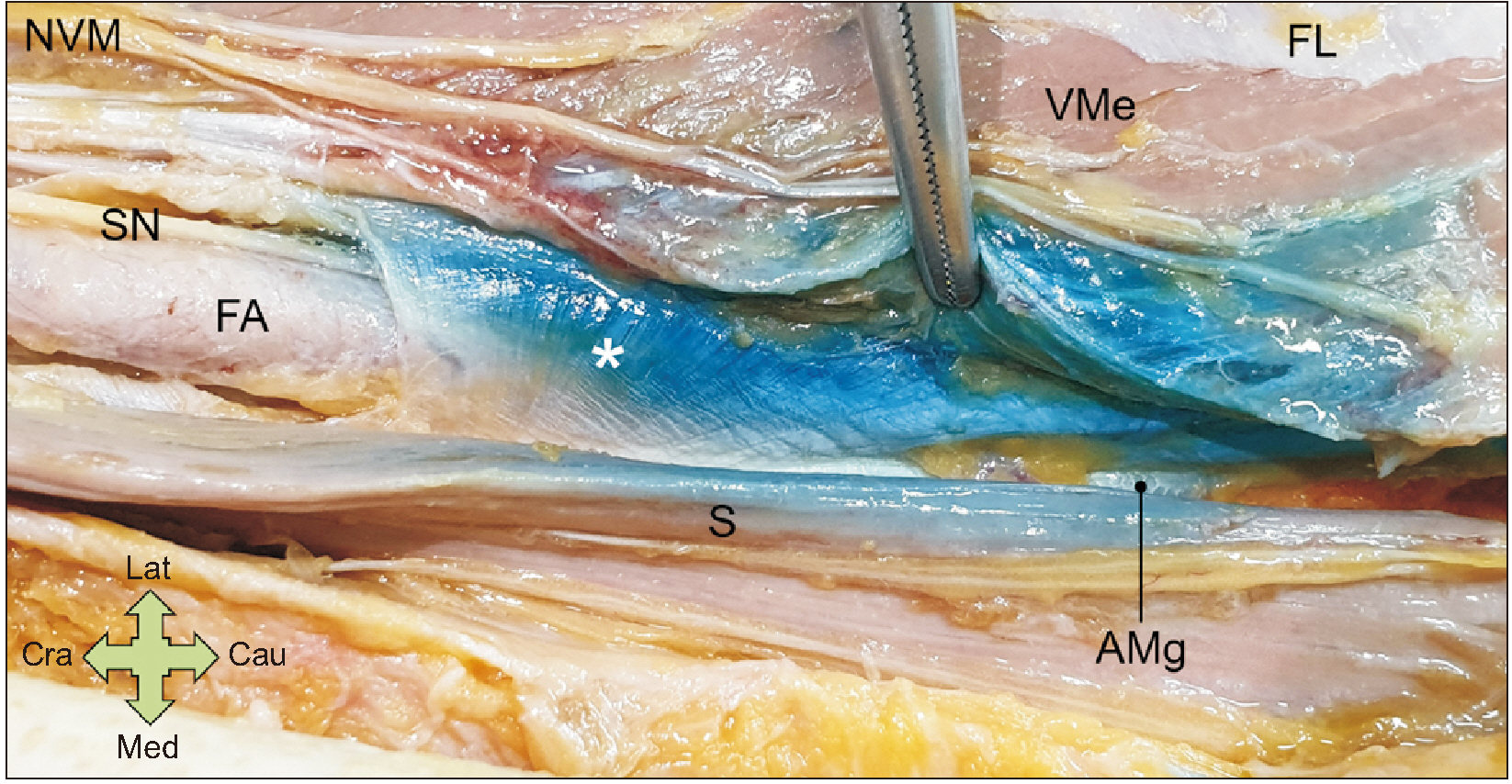
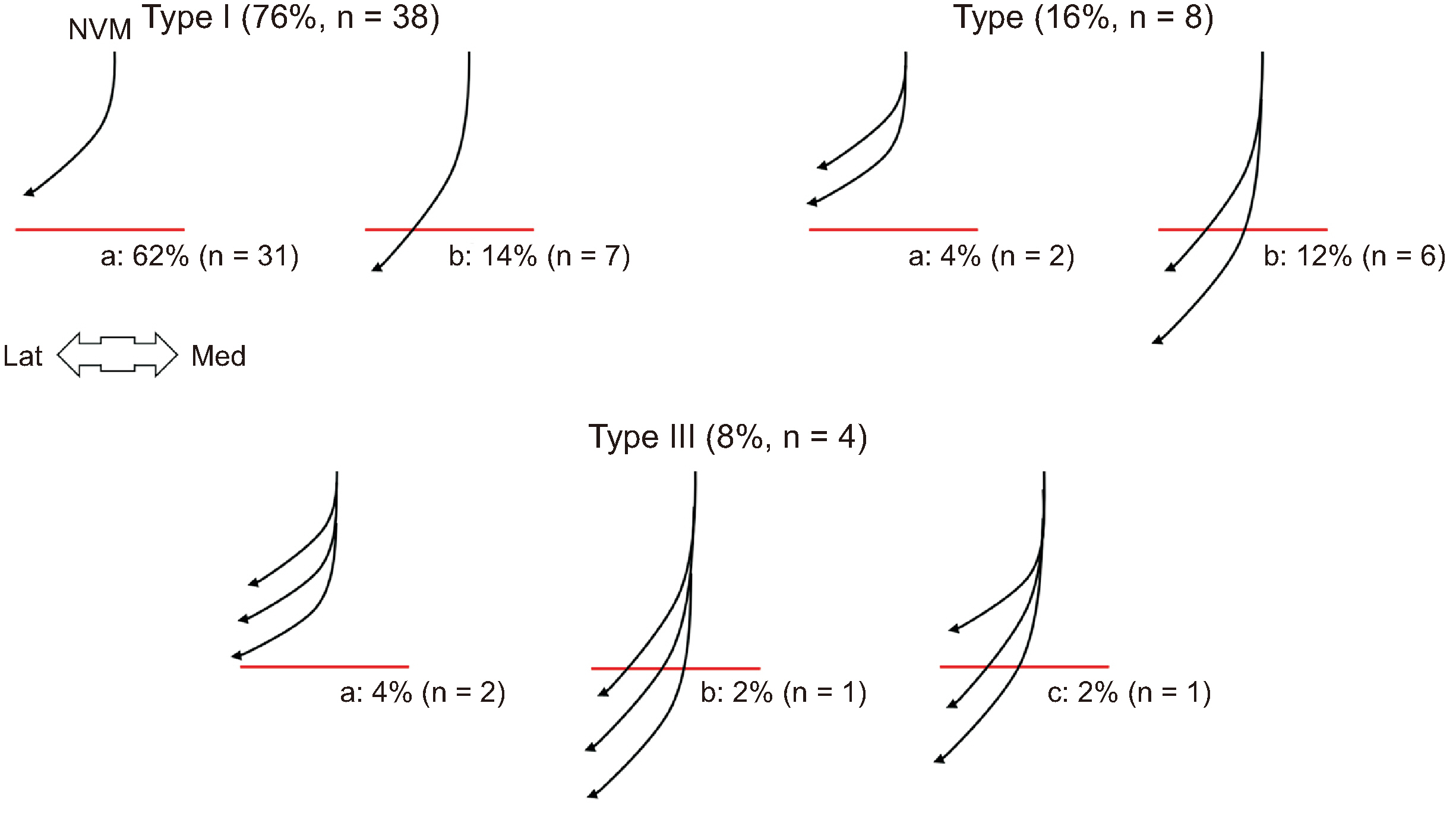
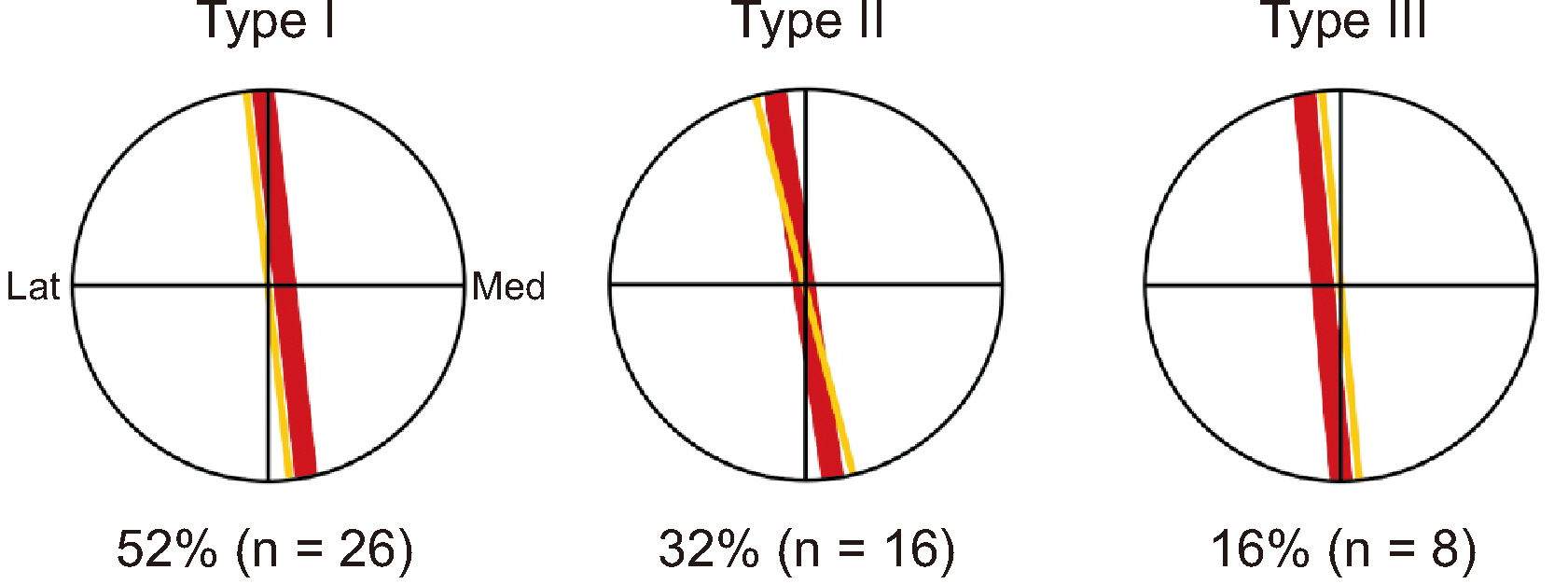
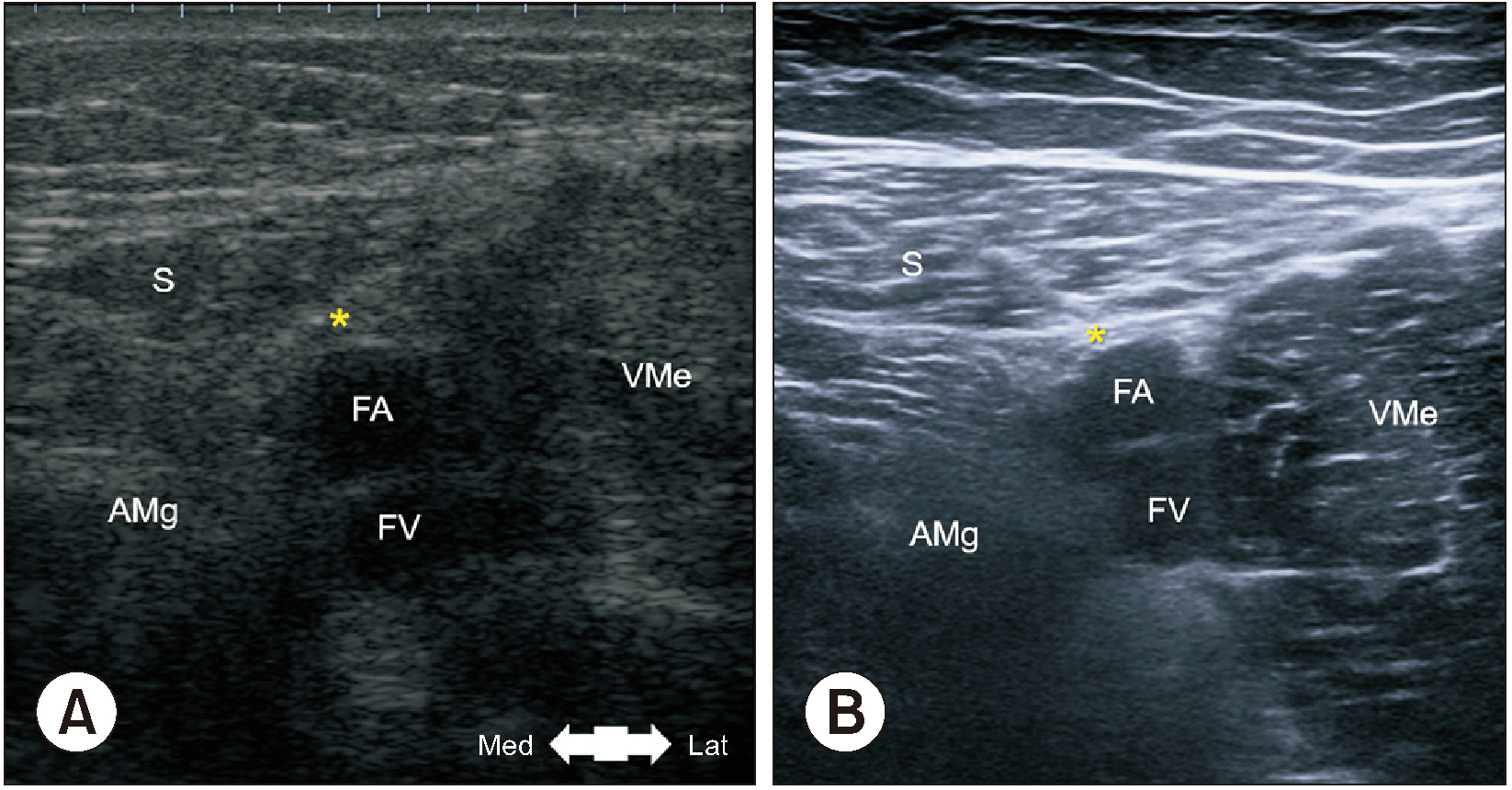
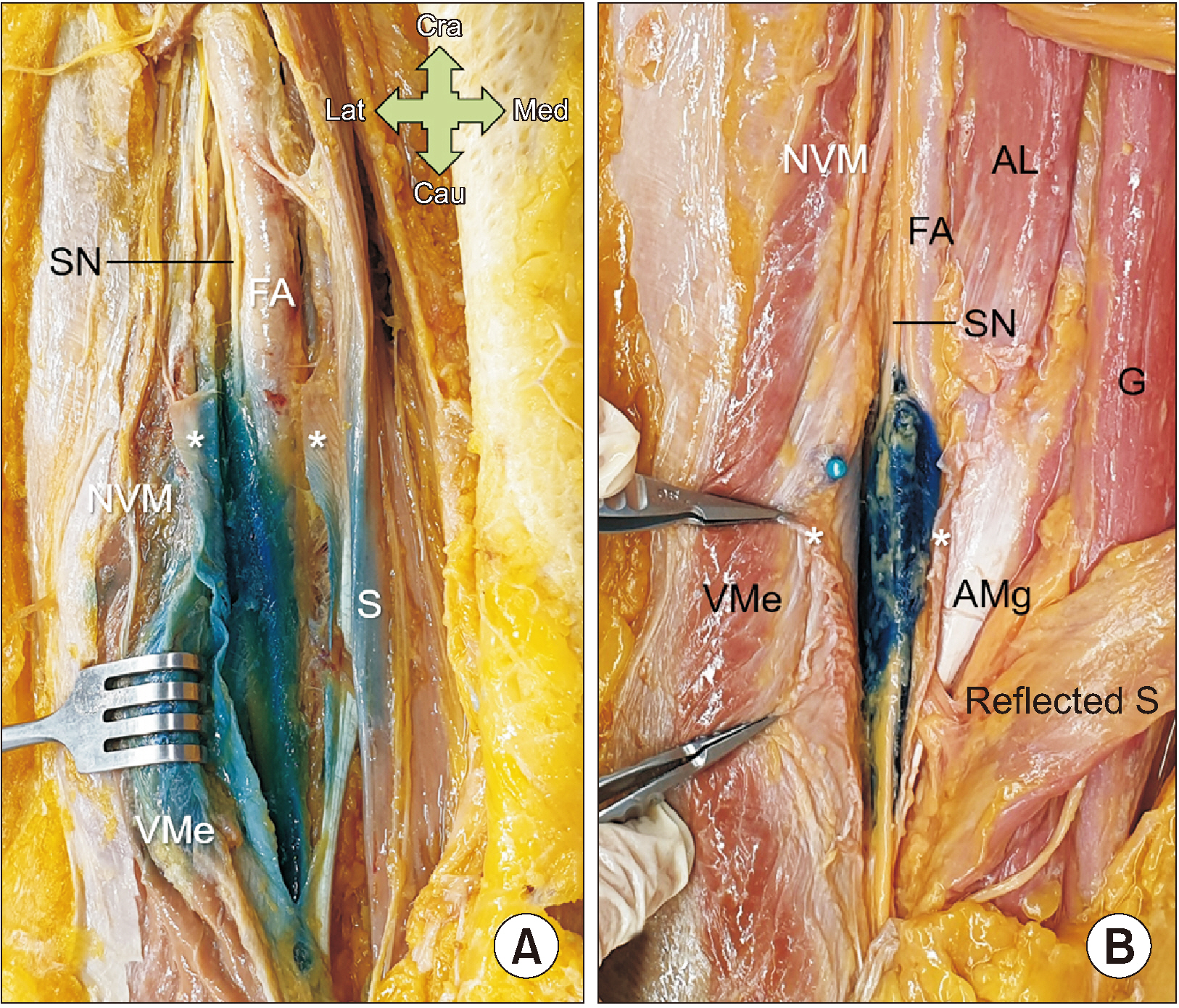
The apex of the femoral triangle was 25.3 ± 2.2 cm distal to the ASIS on the baseline and 5.3 ± 1.0 cm perpendicular to that point. The midpoint of the superior border of the vasto-adductor membrane (VAM) was 27.4 ± 2.0 cm distal to the ASIS on the baseline and 5.0 ± 1.1 cm perpendicular to that point. The VAM had a trapezoidal shape and was connected as an aponeurosis between the medial edge of the vastus medialis muscle and lateral edge of the adductor magnus muscle. The nerve to the vastus medialis penetrated the muscle proximal to the superior border of the VAM in 70% of specimens. The VAM appeared on US as a hyperechoic area connecting the vastus medialis and adductor magnus muscles between the sartorius muscle and femoral artery.
Conclusions
Confirming the crucial landmark, the VAM, is beneficial when performing ACB. It is advisable to insert the needle obliquely below the superior VAM border, and a 5 mL injection is considered sufficient.
Keyword
Figure
Reference
-
1. Rosse C, Gaddum-Rosse P. 1997. Hollinshead's textbook of anatomy. 5th ed. Lippincott-Raven.2. Seo SS, Kim OG, Seo JH, Kim DH, Kim YG, Park BY. 2017; Comparison of the effect of continuous femoral nerve block and adductor canal block after primary total knee arthroplasty. Clin Orthop Surg. 9:303–9. DOI: 10.4055/cios.2017.9.3.303. PMID: 28861197. PMCID: PMC5567025.
Article3. Romanes GJ. 1981. Cunningham's textbook of anatomy. 20th ed. Oxford University Press.4. Dong CC, Dong SL, He FC. 2016; Comparison of adductor canal block and femoral nerve block for postoperative pain in total knee arthroplasty: a systematic review and meta-analysis. Medicine (Baltimore). 95:e2983. DOI: 10.1097/MD.0000000000002983. PMID: 27015172. PMCID: PMC4998367.5. You D, Qin L, Li K, Li D, Zhao G, Li L. 2021; A meta-analysis on advantages of peripheral nerve block post-total knee arthroplasty. Korean J Pain. 34:271–87. DOI: 10.3344/kjp.2021.34.3.271. PMID: 34193634. PMCID: PMC8255149.
Article6. Runner RP, Boden SA, Godfrey WS, Premkumar A, Samady H, Gottschalk MB, et al. 2018; Quadriceps strength deficits after a femoral nerve block versus adductor canal block for anterior cruciate ligament reconstruction: a prospective, single-blinded, randomized trial. Orthop J Sports Med. 6:2325967118797990. DOI: 10.1177/2325967118797990. PMID: 30276220. PMCID: PMC6158619.
Article7. Romanoff ME, Cory PC Jr, Kalenak A, Keyser GC, Marshall WK. 1989; Saphenous nerve entrapment at the adductor canal. Am J Sports Med. 17:478–81. DOI: 10.1177/036354658901700405. PMID: 2782531.
Article8. Joe HB, Choo HS, Yoon JS, Oh SE, Cho JH, Park YU. 2016; Adductor canal block versus femoral nerve block combined with sciatic nerve block as an anesthetic technique for hindfoot and ankle surgery: a prospective, randomized noninferiority trial. Medicine (Baltimore). 95:e5758. DOI: 10.1097/MD.0000000000005758. PMID: 28033291. PMCID: PMC5207587.9. Wang CG, Ding YL, Wang YY, Liu JY, Zhang Q. 2020; Comparison of adductor canal block and femoral triangle block for total knee arthroplasty. Clin J Pain. 36:558–61. DOI: 10.1097/AJP.0000000000000833. PMID: 32271182.
Article10. Chen J, Lesser JB, Hadzic A, Reiss W, Resta-Flarer F. 2014; Adductor canal block can result in motor block of the quadriceps muscle. Reg Anesth Pain Med. 39:170–1. DOI: 10.1097/AAP.0000000000000053. PMID: 24553306.
Article11. Veal C, Auyong DB, Hanson NA, Allen CJ, Strodtbeck W. 2014; Delayed quadriceps weakness after continuous adductor canal block for total knee arthroplasty: a case report. Acta Anaesthesiol Scand. 58:362–4. DOI: 10.1111/aas.12244. PMID: 24372058.
Article12. Ahuja V, Thapa D, Chander A, Gombar S, Gupta R, Gupta S. 2020; Role of dexmedetomidine as adjuvant in postoperative sciatic popliteal and adductor canal analgesia in trauma patients: a randomized controlled trial. Korean J Pain. 33:166–75. DOI: 10.3344/kjp.2020.33.2.166. PMID: 32235017. PMCID: PMC7136291.
Article13. Ming LH, Chin CS, Yang CT, Suhaimi A. 2022; Adductor canal block versus intra-articular steroid and lidocaine injection for knee osteoarthritis: a randomized controlled study. Korean J Pain. 35:191–201. DOI: 10.3344/kjp.2022.35.2.191. PMID: 35354682. PMCID: PMC8977207.
Article14. Kim YD. 2021; Necessity of an exact anatomical understanding for the better pain practice. Korean J Pain. 34:373–4. DOI: 10.3344/kjp.2021.34.4.373. PMID: 34593655. PMCID: PMC8494956.
Article15. Bouaziz H, Benhamou D, Narchi P. 1996; A new approach for saphenous nerve block. Reg Anesth. 21:490.16. Tubbs RS, Loukas M, Shoja MM, Apaydin N, Oakes WJ, Salter EG. 2007; Anatomy and potential clinical significance of the vastoadductor membrane. Surg Radiol Anat. 29:569–73. DOI: 10.1007/s00276-007-0230-4. PMID: 17618402.
Article17. Kapoor R, Adhikary SD, Siefring C, McQuillan PM. 2012; The saphenous nerve and its relationship to the nerve to the vastus medialis in and around the adductor canal: an anatomical study. Acta Anaesthesiol Scand. 56:365–7. DOI: 10.1111/j.1399-6576.2011.02645.x. PMID: 22335278.
Article18. Bendtsen TF, Moriggl B, Chan V, Pedersen EM, Børglum J. 2014; Defining adductor canal block. Reg Anesth Pain Med. 39:253–4. DOI: 10.1097/AAP.0000000000000052. PMID: 24747312.
Article19. Burckett-St Laurant D, Peng P, Girón Arango L, Niazi AU, Chan VW, Agur A, et al. 2016; The nerves of the adductor canal and the innervation of the knee: an anatomic study. Reg Anesth Pain Med. 41:321–7. DOI: 10.1097/AAP.0000000000000389. PMID: 27015545.20. Wong WY, Bjørn S, Strid JM, Børglum J, Bendtsen TF. 2017; Defining the location of the adductor canal using ultrasound. Reg Anesth Pain Med. 42:241–5. DOI: 10.1097/AAP.0000000000000539. PMID: 28002228. PMCID: PMC5318152.
Article21. Kavolus JJ, Sia D, Potter HG, Attarian DE, Lachiewicz PF. 2018; Saphenous nerve block from within the knee is feasible for TKA: MRI and cadaveric study. Clin Orthop Relat Res. 476:30–6. DOI: 10.1007/s11999.0000000000000006. PMID: 29529612. PMCID: PMC5919220.
Article22. Kendir S, Torun Bİ, Akkaya T, Comert A, Tuccar E, Tekdemir I. 2018; Re-defining the anatomical structures for blocking the nerves in adductor canal and sciatic nerve through the same injection site: an anatomical study. Surg Radiol Anat. 40:1267–74. DOI: 10.1007/s00276-018-2094-1. PMID: 30167824.
Article23. Nair A, Dolan J, Tanner KE, Kerr CM, Jones B, Pollock PJ, et al. 2018; Ultrasound-guided adductor canal block: a cadaver study investigating the effect of a thigh tourniquet. Br J Anaesth. 121:890–8. DOI: 10.1016/j.bja.2018.04.044. PMID: 30236251.
Article24. Thiayagarajan MK, Kumar SV, Venkatesh S. 2019; An exact localization of adductor canal and its clinical significance: a cadaveric study. Anesth Essays Res. 13:284–6. DOI: 10.4103/aer.AER_35_19. PMID: 31198246. PMCID: PMC6545962.
Article25. Andersen HL, Andersen SL, Tranum-Jensen J. 2015; The spread of injectate during saphenous nerve block at the adductor canal: a cadaver study. Acta Anaesthesiol Scand. 59:238–45. DOI: 10.1111/aas.12451. PMID: 25496028.
Article26. Goffin P, Lecoq JP, Ninane V, Brichant JF, Sala-Blanch X, Gautier PE, et al. 2016; Interfascial spread of injectate after adductor canal injection in fresh human cadavers. Anesth Analg. 123:501–3. DOI: 10.1213/ANE.0000000000001441. PMID: 27442773.
Article27. Pepper AM, North TW, Sunderland AM, Davis JJ. 2016; Intraoperative adductor canal block for augmentation of periarticular injection in total knee arthroplasty: a cadaveric study. J Arthroplasty. 31:2072–6. DOI: 10.1016/j.arth.2016.02.030. PMID: 26996675.
Article28. Runge C, Moriggl B, Børglum J, Bendtsen TF. 2017; The spread of ultrasound-guided injectate from the adductor canal to the genicular branch of the posterior obturator nerve and the popliteal plexus: a cadaveric study. Reg Anesth Pain Med. 42:725–30. DOI: 10.1097/AAP.0000000000000675. PMID: 28937534.29. Johnston DF, Black ND, Cowden R, Turbitt L, Taylor S. 2019; Spread of dye injectate in the distal femoral triangle versus the distal adductor canal: a cadaveric study. Reg Anesth Pain Med. 44:39–45. DOI: 10.1136/rapm-2018-000002. PMID: 30640651.
Article30. Tran J, Chan VWS, Peng PWH, Agur AMR. 2020; Evaluation of the proximal adductor canal block injectate spread: a cadaveric study. Reg Anesth Pain Med. 45:124–30. DOI: 10.1136/rapm-2019-101091. PMID: 31879373.
Article31. Ham HD, Kim YD, Won HS. 2021; Introduction of a reasonable manner for injection studies using cadavers. Braz J Anesthesiol. 71:188–9. DOI: 10.1016/j.bjane.2020.10.016. PMID: 33894863. PMCID: PMC9373090.
Article32. Callander CL. 1939. Surgical anatomy. 2nd ed. W.B. Saunders.33. Woodburne RT, Burkel WE. 1994. Essentials of human anatomy. 9th ed. Oxford University Press.34. Luerssen TG, Campbell RL, Defalque RJ, Worth RM. 1983; Spontaneous saphenous neuralgia. Neurosurgery. 13:238–41. DOI: 10.1227/00006123-198309000-00004. PMID: 6621837.
Article35. Imani F, Rahimzadeh P, Abolhasan Gharehdag F, Faiz SH. 2013; Sonoanatomic variation of pes anserine bursa. Korean J Pain. 26:249–54. DOI: 10.3344/kjp.2013.26.3.249. PMID: 23861998. PMCID: PMC3710938.
Article36. Benzon HT, Sharma S, Calimaran A. 2005; Comparison of the different approaches to saphenous nerve block. Anesthesiology. 102:633–8. DOI: 10.1097/00000542-200503000-00023. PMID: 15731603.
Article37. Orebaugh SL, Moreno M, Breneman SM, Bigeleisen PE. Bigeleisen PE, Gofeld M, Orebaugh SL, editors. 2009. Ultrasound-guided saphenous nerve block. In: Ultrasound-guided regional anesthesia and pain medicine. Lippincott Williams & Wilkins;p. 108–13.38. Saranteas T, Anagnostis G, Paraskeuopoulos T, Koulalis D, Kokkalis Z, Nakou M, et al. 2011; Anatomy and clinical implications of the ultrasound-guided subsartorial saphenous nerve block. Reg Anesth Pain Med. 36:399–402. DOI: 10.1097/AAP.0b013e318220f172. PMID: 21697687.
Article39. Davis JJ, Bond TS, Swenson JD. 2009; Adductor canal block: more than just the saphenous nerve? Reg Anesth Pain Med. 34:618–9. DOI: 10.1097/AAP.0b013e3181bfbf00. PMID: 19901788.40. Lund J, Jenstrup MT, Jaeger P, Sørensen AM, Dahl JB. 2011; Continuous adductor-canal-blockade for adjuvant post-operative analgesia after major knee surgery: preliminary results. Acta Anaesthesiol Scand. 55:14–9. DOI: 10.1111/j.1399-6576.2010.02333.x. PMID: 21039357.
Article41. Gautier PE, Hadzic A, Lecoq JP, Brichant JF, Kuroda MM, Vandepitte C. 2016; Distribution of injectate and sensory-motor blockade after adductor canal block. Anesth Analg. 122:279–82. DOI: 10.1213/ANE.0000000000001025. PMID: 26678473.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rupture of The Adductor Longus Muscle of The Thigh: 5 Cases Report
- Obturator Nerve Conduction Study Using Magnetic Stimulation in Healthy Adults
- Onset and Duration of Succinylcholine and Vecuronium Neuromuscular Blockade at Laryngeal Adductor and Adductor Pollicis Muscles
- The relative analgesic value of a femoral nerve block versus adductor canal block following total knee arthroplasty: a randomized, controlled, double-blinded study
- The feasibility of direct adductor canal block (DACB) as a part of periarticular injection in total knee arthroplasty