J Korean Neurosurg Soc.
2024 May;67(3):280-288. 10.3340/jkns.2024.0037.
Natural history and clinical manifestation of Pediatric Brain Arteriovenous Malformations
- Affiliations
-
- 1Department of Neurosurgery, University College London, London, UK
- 2Great Ormond Street Hospital for Children, London, UK Great Ormond Street Institute of Child Health, University College London, London, UK
- KMID: 2554865
- DOI: http://doi.org/10.3340/jkns.2024.0037
Abstract
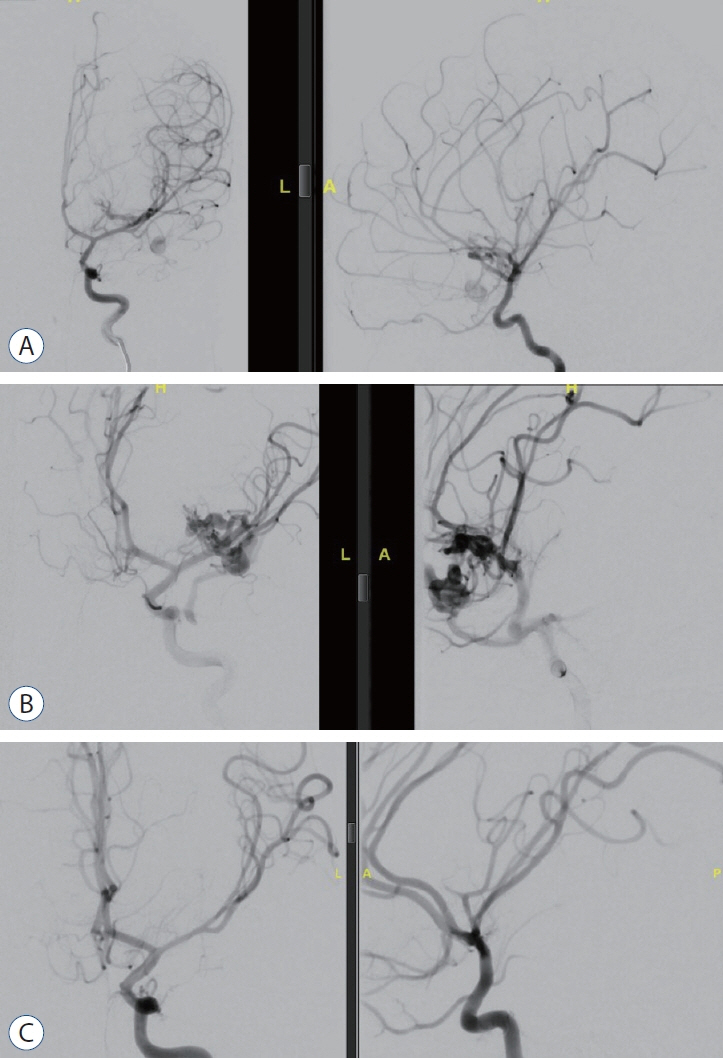
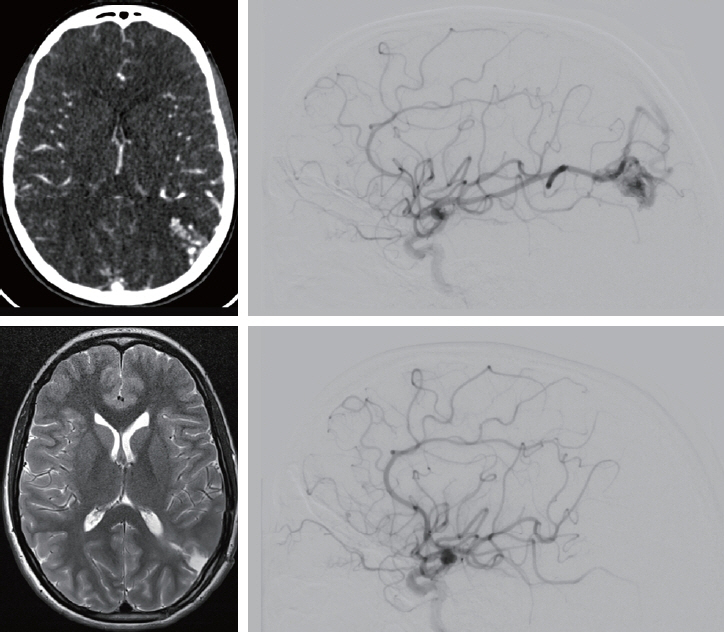
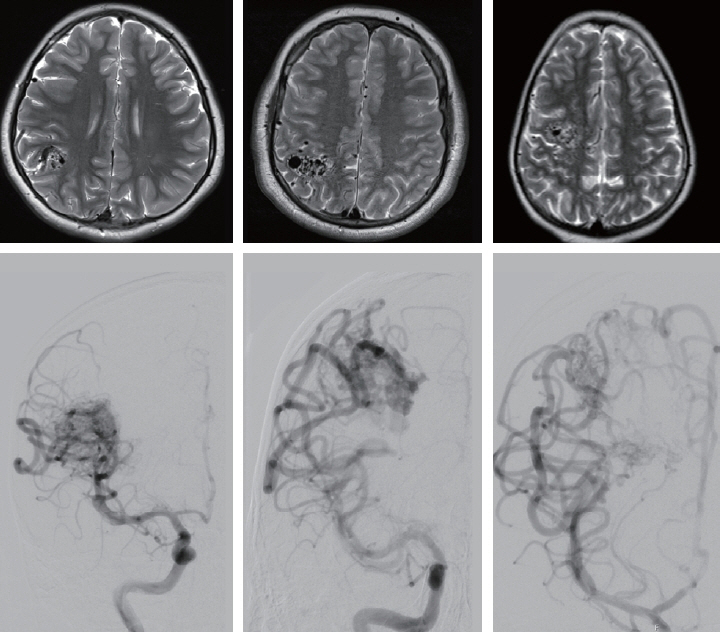
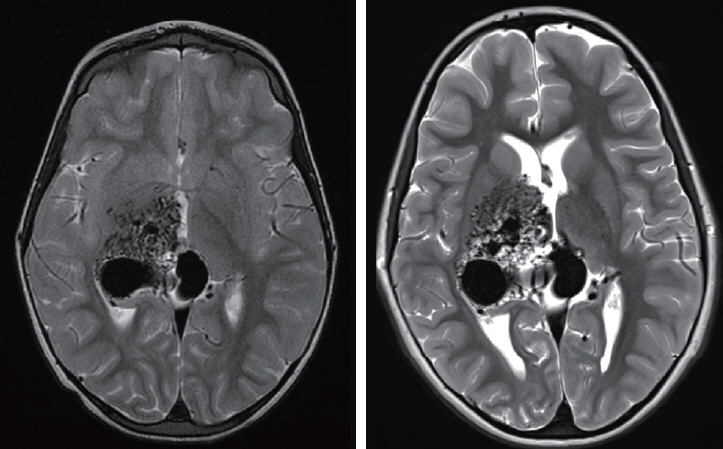
- Brain arteriovenous malformations (bAVMs) are aberrant arteriovenous shunts through a vascular nidus with no intervening capillary beds. They are one of the commonest causes of spontaneous intracranial haemorrhage in children and may be associated with significant morbidity and mortality in cases of rupture. Treatment strategies include microsurgical resection, endovascular embolisation, stereotactic radiosurgery, multimodality treatment with a combination thereof, and particularly in high-grade bAVMs, conservative management. Clinicians involved in treating bAVMs need to have familiarity with the natural history pertaining to bAVMs in terms of risk of rupture, risk factors elevating rupture risk as well as understanding the clinical manifestations of bAVMs. This invited review serves to provide a synthesis on natural history and clinical presentation of bAVMs with particular focus in children to inform decision-making pertaining to management.
Keyword
Figure
Reference
-
References
1. Abecassis IJ, Xu DS, Batjer HH, Bendok BR. Natural history of brain arteriovenous malformations: a systematic review. Neurosurg Focus. 37:E7. 2014.
Article2. Anderson RC, McDowell MM, Kellner CP, Appelboom G, Bruce SS, Kotchetkov IS, et al. Arteriovenous malformation-associated aneurysms in the pediatric population. J Neurosurg Pediatr. 9:11–16. 2012.
Article3. Aoun SG, Bendok BR, Batjer HH. Acute management of ruptured arteriovenous malformations and dural arteriovenous fistulas. Neurosurg Clin N Am. 23:87–103. 2012.
Article4. Beecher JS, Lyon K, Ban VS, Vance A, McDougall CM, Whitworth LA, et al. Delayed treatment of ruptured brain AVMs: is it ok to wait? J Neurosurg. 128:999–1005. 2018.
Article5. Berman MF, Sciacca RR, Pile-Spellman J, Stapf C, Connolly ES Jr, Mohr JP, et al. The epidemiology of brain arteriovenous malformations. Neurosurgery. 47:389–396. discussion 397. 2000.
Article6. Bervini D, Morgan MK, Ritson EA, Heller G. Surgery for unruptured arteriovenous malformations of the brain is better than conservative management for selected cases: a prospective cohort study. J Neurosurg. 121:878–890. 2014.
Article7. Bristol RE, Albuquerque FC, Spetzler RF, Rekate HL, McDougall CG, Zabramski JM. Surgical management of arteriovenous malformations in children. J Neurosurg. 105(2 Suppl):88–93. 2006.
Article8. Chen CJ, Ding D, Derdeyn CP, Lanzino G, Friedlander RM, Southerland AM, et al. Brain arteriovenous malformations: a review of natural history, pathobiology, and interventions. Neurology. 95:917–927. 2020.9. Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP, et al. Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke. 37:1243–1247. 2006.
Article10. Choi JH, Mohr JP. Brain arteriovenous malformations in adults. Lancet Neurol. 4:299–308. 2005.
Article11. Cockroft KM. Natural history of brain arteriovenous malformations. In : Harbaugh RE, Shaffrey C, Couldwell WT, Berger MS, editors. Neurosurgery Knowledge Update: A Comprehensive Review. 1st ed. New York: Thieme;2015. p. 155–160.12. da Costa L, Wallace MC, Ter Brugge KG, O’Kelly C, Willinsky RA, Tymianski M. The natural history and predictive features of hemorrhage from brain arteriovenous malformations. Stroke. 40:100–105. 2009.
Article13. Darsaut TE, Guzman R, Marcellus ML, Edwards MS, Tian L, Do HM, et al. Management of pediatric intracranial arteriovenous malformations: experience with multimodality therapy. Neurosurgery. 69:540–556. discussion 556. 2011.
Article14. Derdeyn CP, Zipfel GJ, Albuquerque FC, Cooke DL, Feldmann E, Sheehan JP, et al. Management of brain arteriovenous malformations: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 48:e200–e224. 2017.
Article15. Dicpinigaitis AJ, Ogulnick JV, Mayer SA, Gandhi CD, Al‐Mufti F. Increase in ruptured cerebral arteriovenous malformations and mortality in the united states: unintended consequences of the ARUBA trial? Stroke Vasc Interv Neurol. 3:e000442. 2023.
Article16. Dodier P, Kranawetter B, Hirschmann D, Dogan M, Cho A, Untersteiner H, et al. Outcome of 107 conservatively managed unruptured brain arteriovenous malformations: a single center’s 30-year experience. J Neurosurg. 139:1025–1035. 2023.
Article17. Ellis JA, Mejia Munne JC, Lavine SD, Meyers PM, Connolly ES Jr, Solomon RA. Arteriovenous malformations and headache. J Clin Neurosci. 23:38–43. 2016.
Article18. Ellis MJ, Armstrong D, Vachhrajani S, Kulkarni AV, Dirks PB, Drake JM, et al. Angioarchitectural features associated with hemorrhagic presentation in pediatric cerebral arteriovenous malformations. J Neurointerv Surg. 5:191–195. 2013.
Article19. Friedlander RM. Clinical practice. Arteriovenous malformations of the brain. N Engl J Med. 356:2704–2712. 2007.20. Fung LW, Ganesan V. Arteriovenous malformations presenting with papilloedema. Dev Med Child Neurol. 46:626–627. 2004.
Article21. Goldberg J, Raabe A, Bervini D. Natural history of brain arteriovenous malformations: systematic review. J Neurosurg Sci. 62:437–443. 2018.
Article22. Gross BA, Du R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg. 118:437–443. 2013.
Article23. Gross BA, Du R. Rate of re-bleeding of arteriovenous malformations in the first year after rupture. J Clin Neurosci. 19:1087–1088. 2012.
Article24. Gross BA, Storey A, Orbach DB, Scott RM, Smith ER. Microsurgical treatment of arteriovenous malformations in pediatric patients: the Boston Children’s Hospital experience. J Neurosurg Pediatr. 15:71–77. 2015.
Article25. Haas DC. Arteriovenous malformations and migraine: case reports and an analysis of the relationship. Headache. 31:509–513. 1991.
Article26. Halim AX, Johnston SC, Singh V, McCulloch CE, Bennett JP, Achrol AS, et al. Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain within a defined population. Stroke. 35:1697–1702. 2004.
Article27. Haridas A, Dashti R, Shokunhfar T, Shaibani A. Pediatric Arteriovenous Malformations. In : Di Rocco C, Pang D, Rutka JT, editors. Textbook of Pediatric Neurosurgery. Cham: Springer;2020. Vol 2:p. 1135–1168.28. Hirschmann D, Goebl P, Witte FH, Gatterbauer B, Wang WT, Dodier P, et al. Evaluation of the radiosurgical treatment of cerebral arteriovenous malformations: a retrospective single-center analysis of three decades. J Neurointerv Surg. 12:401–406. 2020.
Article29. Hoffman C, Riina HA, Stieg P, Allen B, Gobin YP, Santillan A, et al. Associated aneurysms in pediatric arteriovenous malformations and the implications for treatment. Neurosurgery. 69:315–322. 2011.
Article30. Karlsson B, Jokura H, Yang HC, Yamamoto M, Martinez R, Kawagishi J, et al. The NASSAU (new assessment of cerebral arteriovenous malformations yet unruptured) analysis: are the results from the ARUBA trial also applicable to unruptured arteriovenous malformations deemed suitable for Gamma Knife surgery? Neurosurgery. 85:E118–E124. 2019.
Article31. Kellner CP, McDowell MM, Phan MQ, Connolly ES, Lavine SD, Meyers PM, et al. Number and location of draining veins in pediatric arteriovenous malformations: association with hemorrhage. J Neurosurg Pediatr. 14:538–545. 2014.
Article32. Kondziolka D, McLaughlin MR, Kestle JR. Simple risk predictions for arteriovenous malformation hemorrhage. Neurosurgery. 37:851–855. 1995.
Article33. Kupersmith MJ, Vargas ME, Yashar A, Madrid M, Nelson K, Seton A, et al. Occipital arteriovenous malformations: visual disturbances and presentation. Neurology. 46:953–957. 1996.34. Magro E, Gentric JC, Darsaut TE, Ziegler D, Bojanowski MW, Raymond J. Responses to ARUBA: a systematic review and critical analysis for the design of future arteriovenous malformation trials. J Neurosurg. 126:486–494. 2017.
Article35. Mahalick DM, Ruff RM, Hoi SU. Neuropsychological sequelae of arteriovenous malformations. Neurosurgery. 29:351–357. 1991.
Article36. Mast H, Mohr JP, Osipov A, Pile-Spellman J, Marshall RS, Lazar RM, et al. ‘Steal’ is an unestablished mechanism for the clinical presentation of cerebral arteriovenous malformations. Stroke. 26:1215–1220. 1995.
Article37. Mohr JP, Overbey JR, Hartmann A, Kummer RV, Al-Shahi Salman R, Kim H, et al. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol. 19:573–581. 2020.
Article38. Mohr JP, Parides MK, Stapf C, Moquete E, Moy CS, Overbey JR, et al. Medical management with or without interventional therapy for unruptured brain arteriovenous malformations (ARUBA): a multicentre, nonblinded, randomised trial. Lancet. 383:614–621. 2014.
Article39. Nagata S, Morioka T, Natori Y, Sasaki T. Surgical treatment of nonruptured giant occipital arteriovenous malformations with frequent migraine-like headache. Neurol Med Chir (Tokyo). 46:441–445. 2006.
Article40. Niazi TN, Klimo P Jr, Anderson RC, Raffel C. Diagnosis and management of arteriovenous malformations in children. Neurosurg Clin N Am. 21:443–456. 2010.
Article41. Plumptre I, Robertson F, Rennie A, James G, Syed SB. Atypical capillary malformations with subsequent diplegia: a difficult case of capillary malformation-arteriovenous malformation syndrome. Pediatr Dermatol. 37:162–164. 2020.
Article42. Pollock BE, Link MJ, Stafford SL, Garces YI, Foote RL. Stereotactic radiosurgery for arteriovenous malformations: the effect of treatment period on patient outcomes. Neurosurgery. 78:499–509. 2016.43. Reitz M, von Spreckelsen N, Vettorazzi E, Burkhardt T, Grzyska U, Fiehler J, et al. Angioarchitectural risk factors for hemorrhage and clinical long-term outcome in pediatric patients with cerebral arteriovenous malformations. World Neurosurg. 89:540–551. 2016.
Article44. Sahlein DH, Mora P, Becske T, Huang P, Jafar JJ, Connolly ES, et al. Features predictive of brain arteriovenous malformation hemorrhage: extrapolation to a physiologic model. Stroke. 45:1964–1970. 2014.
Article45. Sheth RD, Bodensteiner JB. Progressive neurologic impairment from an arteriovenous malformation vascular steal. Pediatr Neurol. 13:352–354. 1995.
Article46. Solomon RA, Connolly ES Jr. Arteriovenous malformations of the brain. N Engl J Med. 376:1859–1866. 2017.
Article47. Soltanolkotabi M, Schoeneman SE, Alden TD, Hurley MC, Ansari SA, DiPatri AJ Jr, et al. Onyx embolization of intracranial arteriovenous malformations in pediatric patients. J Neurosurg Pediatr. 11:431–437. 2013.
Article48. Spetzler RF, Ponce FA. A 3-tier classification of cerebral arteriovenous malformations. Clinical article. J Neurosurg. 114:842–849. 2011.49. Stapf C, Mast H, Sciacca RR, Berenstein A, Nelson PK, Gobin YP, et al. The New York Islands AVM Study: design, study progress, and initial results. Stroke. 34:e29–e33. 2003.50. Stapf C, Mast H, Sciacca RR, Choi JH, Khaw AV, Connolly ES, et al. Predictors of hemorrhage in patients with untreated brain arteriovenous malformation. Neurology. 66:1350–1355. 2006.
Article51. Stapf C, Mohr JP, Pile-Spellman J, Solomon RA, Sacco RL, Connolly ES Jr. Epidemiology and natural history of arteriovenous malformations. Neurosurg Focus. 11:e1. 2001.
Article52. Valdivielso-Ramos M, Martin-Santiago A, Azaña JM, Hernández-Nuñez A, Vera A, Perez B, et al. Capillary malformation-arteriovenous malformation syndrome: a multicentre study. Clin Exp Dermatol. 46:300–305. 2021.
Article53. van Beijnum J, Lovelock CE, Cordonnier C, Rothwell PM, Klijn CJ, AlShahi Salman R, et al. Outcome after spontaneous and arteriovenous malformation-related intracerebral haemorrhage: population-based studies. Brain. 132:537–543. 2009.
Article54. Yamada S, Takagi Y, Nozaki K, Kikuta K, Hashimoto N. Risk factors for subsequent hemorrhage in patients with cerebral arteriovenous malformations. J Neurosurg. 107:965–972. 2007.
Article55. Yang W, Liu A, Hung AL, Braileanu M, Wang JY, Caplan JM, et al. Lower risk of intracranial arteriovenous malformation hemorrhage in patients with hereditary hemorrhagic telangiectasia. Neurosurgery. 78:684–693. 2016.
Article56. Zhang Y, Chen Y, Han H, Ma L, Li R, Li Z, et al. Timing of microsurgical resection for ruptured brain arteriovenous malformations: a propensity score-matched analysis using prospective single-center registry data. J Neurosurg. 140:164–171. 2023.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Pathophysiology of Cerebral Arteiovenous Malformation
- 3 Cases of Surgically Treated Arteriovenous Malformations of the Brain
- The Multiple Brain Abscesses Associated with Congenital Pulmonary Arteriovenous Malformations: A Case Report
- Management of Pediatric Intracranial Arteriovenous Malformations
- Dural Arteriovenous Malformation Associated with Meningioma: Spontaneous Disappearance after Tumor Removal: Case Report