Ann Rehabil Med.
2024 Apr;48(2):155-162. 10.5535/arm.23109.
Applying ICF Framework to Explore the Factors That Influence Quality of Life in Patients After Lung Surgery
- Affiliations
-
- 1The Second School of Clinical Medicine, Southern Medical University, Guangzhou, China
- 2Department of Physical Medicine and Rehabilitation, Guangdong Geriatric Institute, Guangdong Provincial People’s Hospital (Guangdong Academy of Medical Sciences), Southern Medical University, Guangzhou, China
- 3Department of Physical Medicine and Rehabilitation, Shenzhen Children’s Hospital, Shenzhen, China
- 4Department of Physical Medicine and Rehabilitation, He Xian Memorial Affiliated Hospital of Southern Medical University, Guangzhou, China
- 5Department of Physical Medicine and Rehabilitation, Gaozhou People’s Hospital, Maoming, China
- KMID: 2554791
- DOI: http://doi.org/10.5535/arm.23109
Abstract
Objective
To explore the relationship between pulmonary function, physical activity, and health-related quality of life (QoL) in resected lung cancer patients based on the International Classification of Functioning, Disability, and Health (ICF) framework developed by the World Health Organization to describe health and health-related states.
Methods
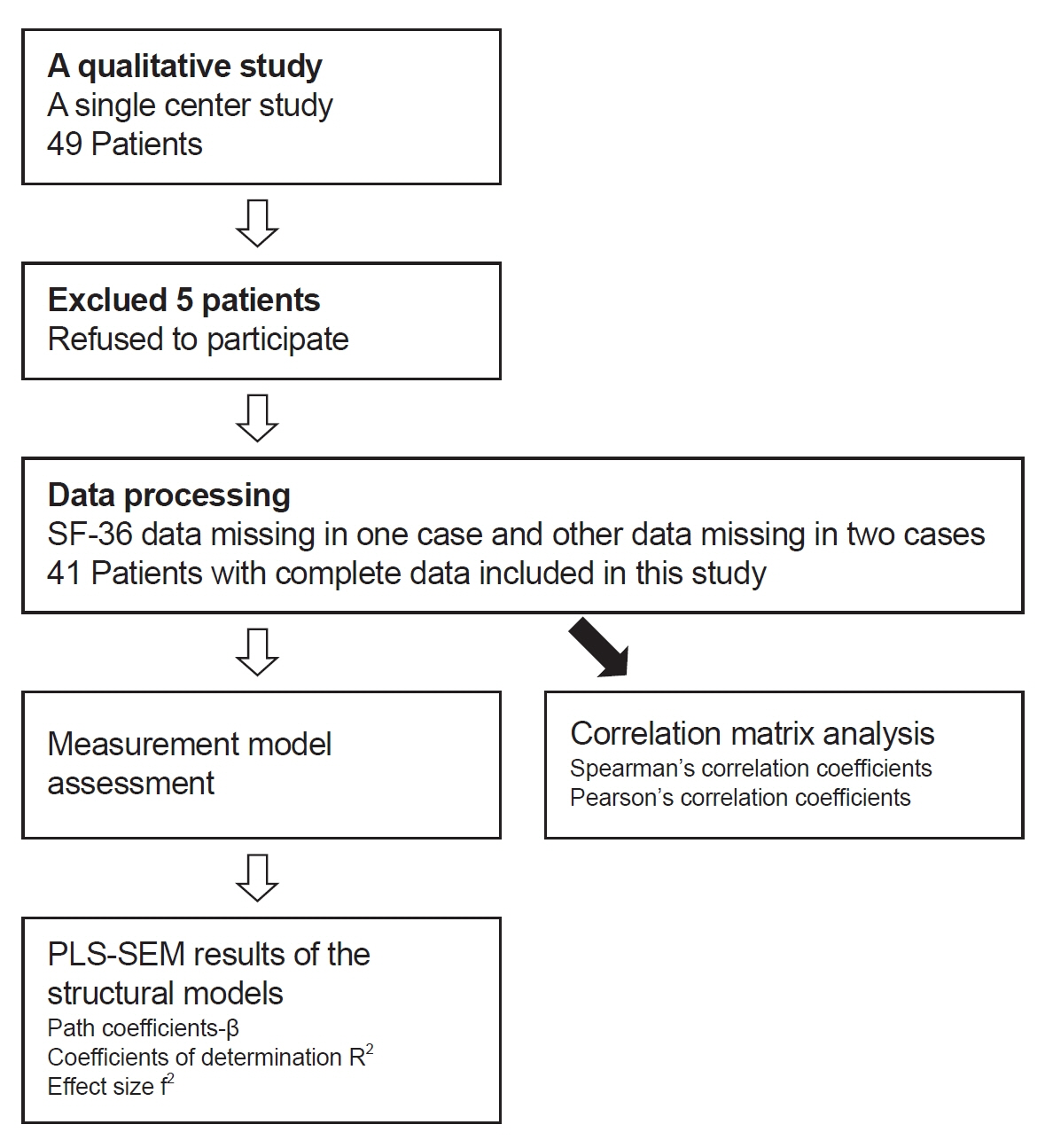
A quantitative study was designed with postoperative lung cancer survivors to assess personal characteristics. We also assessed functional impairment related to the lung using forced vital capacity (FVC) and forced expiratory volume at 1 second (FEV1), activity limitations using maximal oxygen consumption (VO2max), anaerobic threshold (AT) and 6-minute walking distance (6MWD), and participation restriction using the 36-item Short Form Health Survey V1 (SF-36). Data analyses were conducted using the multivariate method and Smart- PLS to examine path coefficient among the measures.
Results
Forty-one patients were enrolled in this study. FVC and FEV1 were poorly correlated with QoL, and 6MWD, AT, or VO2max were positively associated with QoL. AT or VO2max showed a significant (p<0.01) direct path with SF-36 in the ICF model. Although age and body mass index were not strongly correlated with QoL, these personal factors had a medium to large effect on perceived QoL.
Conclusion
Disability is a complex in patients with lung resection, and physical activity plays an important role in enabling participation. Improving VO2max and AT is needed to improve the QoL of resected lung cancer patients. We should also pay more attention to contextual factors that have a significant impact on social participation.
Keyword
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA Cancer J Clin. 2019; 69:7–34.
Article2. Chen HL, Liu K, You QS. Self-efficacy, cancer-related fatigue, and quality of life in patients with resected lung cancer. Eur J Cancer Care (Engl). 2018; 27:e12934.
Article3. Brocki BC, Westerdahl E, Langer D, Souza DSR, Andreasen JJ. Decrease in pulmonary function and oxygenation after lung resection. ERJ Open Res. 2018; 4:00055–2017.
Article4. Saito H, Shiraishi A, Nomori H, Matsui H, Yoshida K, Matsue Y, et al. Impact of age on the recovery of six-minute walking distance after lung cancer surgery: a retrospective cohort study. Gen Thorac Cardiovasc Surg. 2020; 68:150–7.
Article5. Szeliga E, Czenczek-Lewandowska E, Kontek A, Wolan-Nieroda A, Guzik A, Walicka-Cupryś K. Evaluation of the quality of life after surgical removal of lung cancer. Adv Respir Med. 2019; 87:14–9.
Article6. Halank M, Einsle F, Lehman S, Bremer H, Ewert R, Wilkens H, et al. Exercise capacity affects quality of life in patients with pulmonary hypertension. Lung. 2013; 191:337–43.
Article7. Engberg E, Tikkanen HO, Koponen A, Hägglund H, Kukkonen-Harjula K, Tiitinen A, et al. Cardiorespiratory fitness and health-related quality of life in women at risk for gestational diabetes. Scand J Med Sci Sports. 2018; 28:203–11.
Article8. Ha D, Ries AL, Mazzone PJ, Lippman SM, Fuster MM. Exercise capacity and cancer-specific quality of life following curative intent treatment of stage I-IIIA lung cancer. Support Care Cancer. 2018; 26:2459–69.
Article9. Brunelli A, Socci L, Refai M, Salati M, Xiumé F, Sabbatini A. Quality of life before and after major lung resection for lung cancer: a prospective follow-up analysis. Ann Thorac Surg. 2007; 84:410–6.
Article10. Leonardi M. Measuring health and disability: supporting policy development. The European MHADIE project. Disabil Rehabil. 2010; 32 Suppl 1:S1–8.11. Moulton E, Wilson R, Deluzio K. Movement and mobility: a concept analysis. ANS Adv Nurs Sci. 2019; 42:E11–23.12. Polański J, Jankowska-Polańska B, Mazur G. Relationship between nutritional status and quality of life in patients with lung cancer. Cancer Manag Res. 2021; 13:1407–16.
Article13. Luszczynska A, Pawlowska I, Cieslak R, Knoll N, Scholz U. Social support and quality of life among lung cancer patients: a systematic review. Psychooncology. 2013; 22:2160–8.
Article14. Pearman T. Psychosocial factors in lung cancer: quality of life, economic impact, and survivorship implications. J Psychosoc Oncol. 2008; 26:69–80.15. Bade BC, Gan G, Li F, Lu L, Tanoue L, Silvestri GA, et al. Randomized trial of physical activity on quality of life and lung cancer biomarkers in patients with advanced stage lung cancer: a pilot study. BMC Cancer. 2021; 21:352.
Article16. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005; 26:319–38.17. Mänttäri A, Suni J, Sievänen H, Husu P, Vähä-Ypyä H, Valkeinen H, et al. Six-minute walk test: a tool for predicting maximal aerobic power (VO2 max) in healthy adults. Clin Physiol Funct Imaging. 2018; 38:1038–45.18. Ware JE Jr, Gandek B. Overview of the SF-36 Health Survey and the International Quality of Life Assessment (IQOLA) Project. J Clin Epidemiol. 1998; 51:903–12.
Article19. Hair JF, Ringle CM, Sarstedt M. PLS-SEM: indeed a silver bullet. J Mark Theory Pract. 2011; 19:139–52.
Article20. Hair JF, Risher JJ, Sarstedt M, Ringle CM. When to use and how to report the results of PLS-SEM. Eur Bus Rev. 2019; 31:2–24.
Article21. Yang P, Cheville AL, Wampfler JA, Garces YI, Jatoi A, Clark MM, et al. Quality of life and symptom burden among long-term lung cancer survivors. J Thorac Oncol. 2012; 7:64–70.
Article22. Wang PP, Badley EM, Gignac M. Exploring the role of contextual factors in disability models. Disabil Rehabil. 2006; 28:135–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Research on the Quality of Life of the Parents by Functions, Activities, Participation, and Environmental Factors of Children with Cerebral Palsy Using ICF-CY Checklist
- Predictors of Quality of Life Among Older Residents in Rural and Urban Areas in Indonesia: An Approach Using the International Classification of Functioning, Disability, and Health
- Assessment of Upper Extremity Function in People With Stroke Based on the Framework of the ICF: A Narrative Review
- Moderating Effect of Inner Strength between Mood Status and Quality of Life in Female Patients with Lung Cancer
- Functioning Characteristics of Patients with Neck Pain: ICF Concept Based