Cardiovasc Prev Pharmacother.
2024 Apr;6(2):57-64. 10.36011/cpp.2024.6.e6.
Changes in cardiovascular-related health behaviors after the end of social distancing: the 2023 Cardiovascular Disease Prevention Awareness Survey
- Affiliations
-
- 1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2554782
- DOI: http://doi.org/10.36011/cpp.2024.6.e6
Abstract
- Background
The COVID-19 pandemic and the implementation of social distancing have been reported to negatively impact cardiovascular-related health behaviors. However, the effects of lifting social distancing restrictions on these health behaviors remain unclear. This study investigated public awareness and behavioral changes related to cardiovascular disease prevention after the end of social distancing.
Methods
Between June 5 and June 12, 2023, 2,000 adults participated in the 2023 Cardiovascular Disease Prevention Awareness Survey in Korea. The survey comprehensively addressed sociodemographic factors, cardiometabolic disease history, cardiovascular disease concern, prevention awareness, and behavioral changes after the end of social distancing. Logistic regression analyses were performed to assess the associations between behavioral changes and sociodemographic factors.
Results
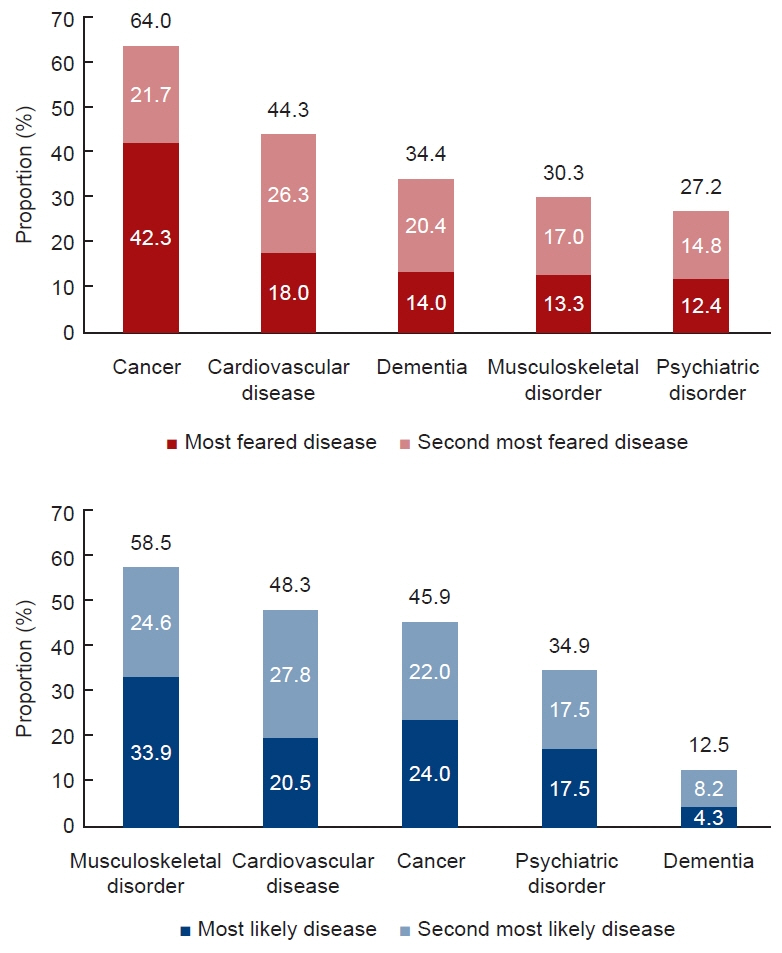
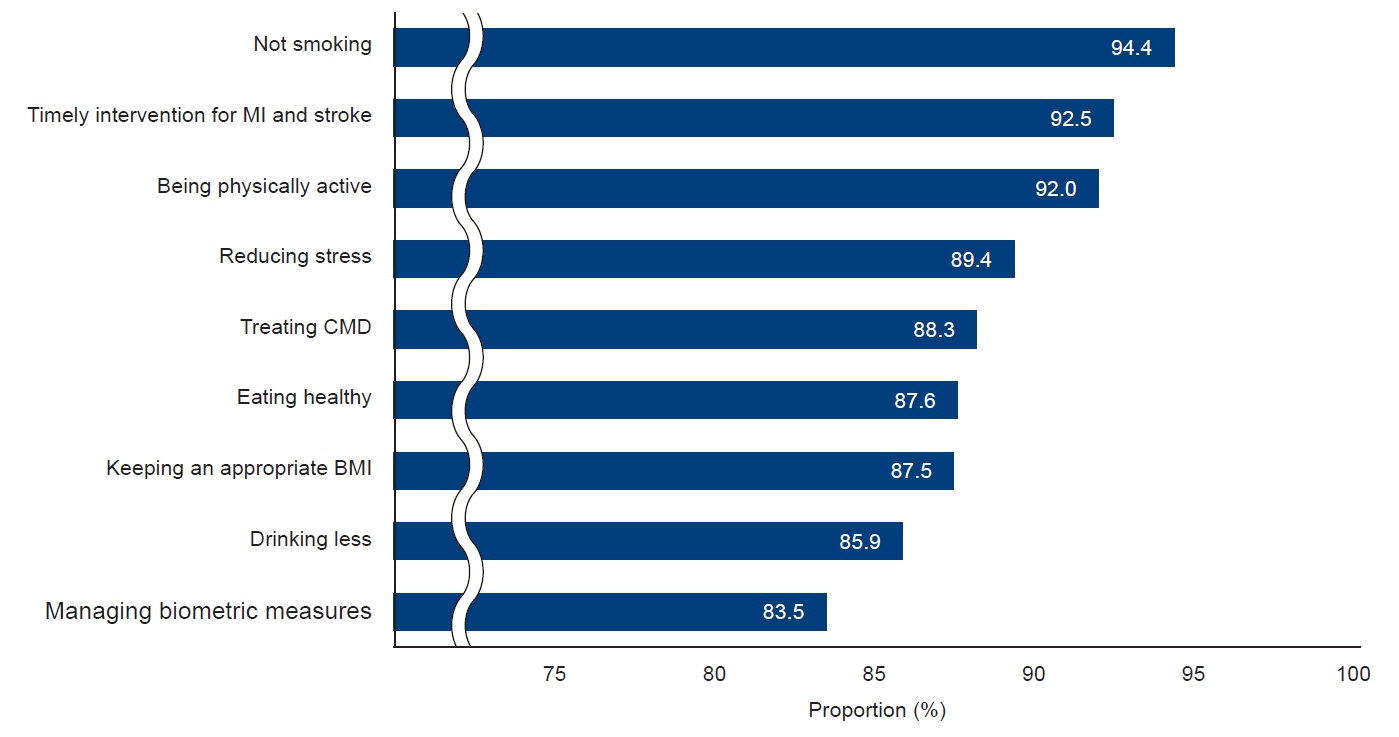
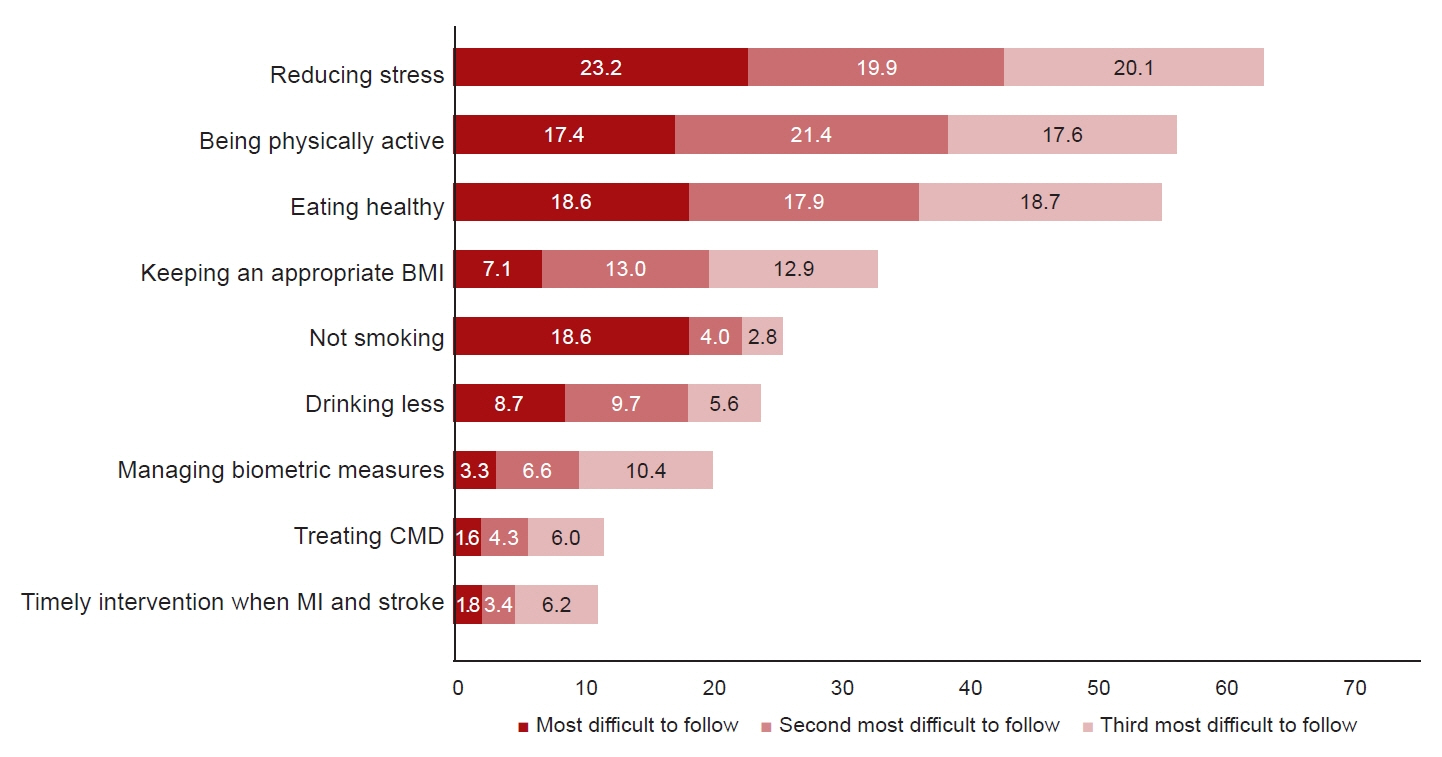
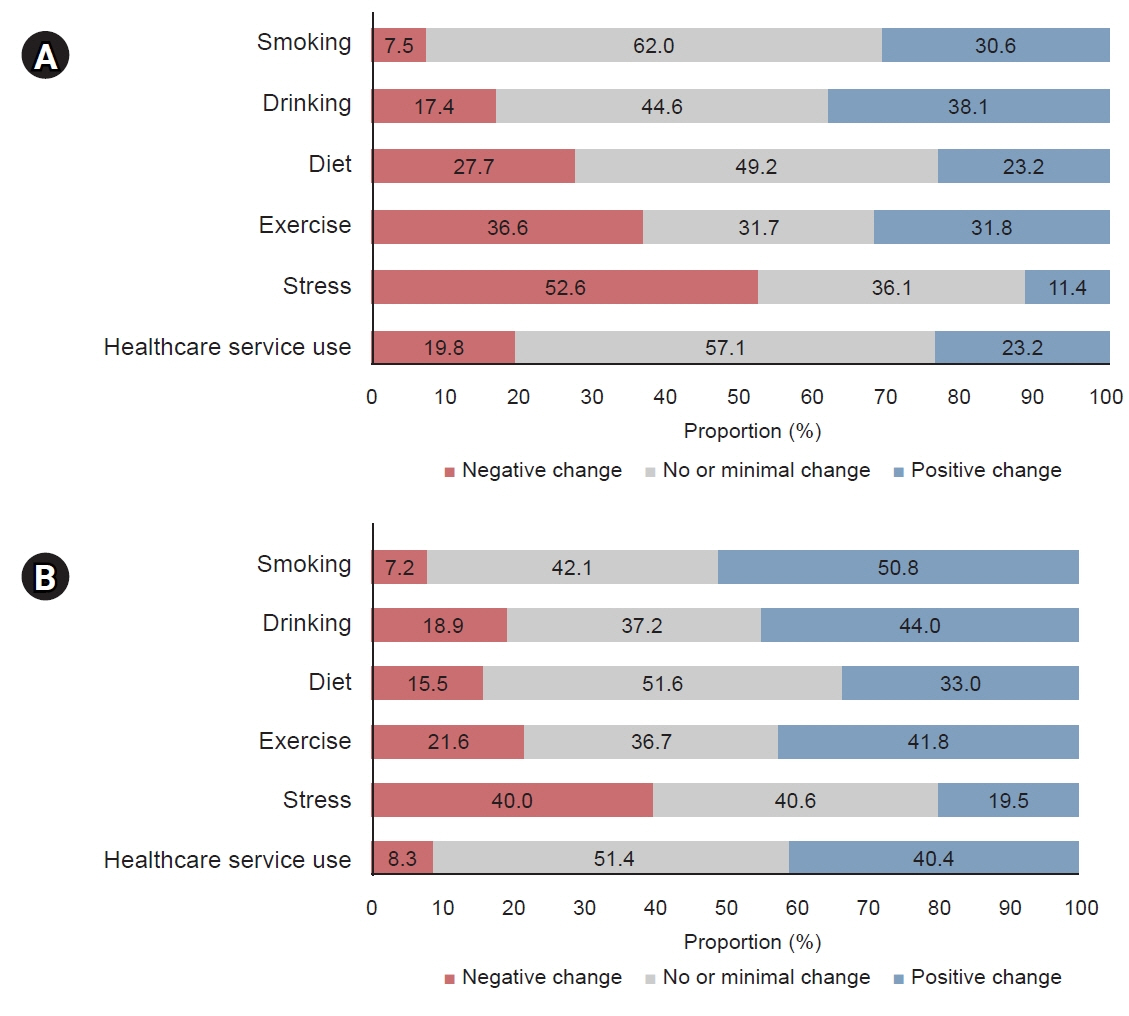
Cardiovascular disease ranked as the second most feared disease (most feared, 18.0%; second most feared, 26.3%) after cancer (most feared, 42.3%; second most feared, 21.7%). Among nine cardiovascular disease prevention recommendations, stress management, being physically active, and maintaining a healthy diet were perceived as the most challenging recommendations. After the end of social distancing, there were more positive changes than negative changes in smoking, alcohol consumption, dietary habits, physical activity, and healthcare service use, whereas stress management more frequently changed negatively (40.0%) than it changed positively (19.5%).
Conclusions
Positive changes in cardiovascular-related health behaviors, except for stress management, were observed after the end of social distancing. Further research is necessary to fully comprehend the impact of discontinuing social distancing practices.
Figure
Reference
-
1. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392:1736–88.2. Roth GA, Forouzanfar MH, Moran AE, Barber R, Nguyen G, Feigin VL, et al. Demographic and epidemiologic drivers of global cardiovascular mortality. N Engl J Med. 2015; 372:1333–41.
Article3. Zhao D. Epidemiological features of cardiovascular disease in Asia. JACC Asia. 2021; 1:1–13.
Article4. Rodgers JL, Jones J, Bolleddu SI, Vanthenapalli S, Rodgers LE, Shah K, et al. Cardiovascular risks associated with gender and aging. J Cardiovasc Dev Dis. 2019; 6:19.
Article5. Korean Statistical Information Service. Future population projection. Statistics Korea;[updated 2022 May 26; cited 2023 Nov 27]. Available from: https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1BPB001&conn_path=I2.6. Lloyd-Jones DM, Allen NB, Anderson CA, Black T, Brewer LC, Foraker RE, et al. Life’s essential 8: updating and enhancing the American Heart Association’s Construct of Cardiovascular Health: a presidential advisory from the American Heart Association. Circulation. 2022; 146:e18–43.
Article7. Siervo M, Lara J, Chowdhury S, Ashor A, Oggioni C, Mathers JC. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta-analysis. Br J Nutr. 2015; 113:1–15.
Article8. Ahmed HM, Blaha MJ, Nasir K, Rivera JJ, Blumenthal RS. Effects of physical activity on cardiovascular disease. Am J Cardiol. 2012; 109:288–95.
Article9. Hackshaw A, Morris JK, Boniface S, Tang JL, Milenkovic D. Low cigarette consumption and risk of coronary heart disease and stroke: meta-analysis of 141 cohort studies in 55 study reports. BMJ. 2018; 360:j5855.
Article10. Wang D, Li W, Cui X, Meng Y, Zhou M, Xiao L, et al. Sleep duration and risk of coronary heart disease: a systematic review and meta-analysis of prospective cohort studies. Int J Cardiol. 2016; 219:231–9.
Article11. Korea Disease Control and Prevention Agency (KDCA). Chronic disease prevention and management. KDCA;[updated 2023 Aug 30; cited 2023 Nov 27]. Available from: https://www.kdca.go.kr/contents.es?mid=a20303020300.12. Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw Open. 2020; 3:e2019686.
Article13. Fuzeki E, Groneberg DA, Banzer W. Physical activity during COVID-19 induced lockdown: recommendations. J Occup Med Toxicol. 2020; 15:25.
Article14. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020; 75:2871–2.
Article15. Kim E, Jung CH, Kim DJ, Ko SH, Lee HY, Lee KY, et al. Changes in cardiovascular-related health behaviors during the COVID-19 pandemic. Cardiovasc Prev Pharmacother. 2023; 5:15–23.
Article16. Yoon J, Yoon SJ. Quantifying burden of disease to measure population health in Korea. J Korean Med Sci. 2016; 31 Suppl 2(Suppl 2):S101–7.
Article17. Lim S, Lim H, Despres JP. Collateral damage of the COVID-19 pandemic on nutritional quality and physical activity: perspective from South Korea. Obesity (Silver Spring). 2020; 28:1788–90.
Article18. Ferrante G, Camussi E, Piccinelli C, Senore C, Armaroli P, Ortale A, et al. Did social isolation during the SARS-CoV-2 epidemic have an impact on the lifestyles of citizens? Epidemiol Prev. 2020; 44(5-6 Suppl 2):353–62.19. Pecanha T, Goessler KF, Roschel H, Gualano B. Social isolation during the COVID-19 pandemic can increase physical inactivity and the global burden of cardiovascular disease. Am J Physiol Heart Circ Physiol. 2020; 318:H1441–6.20. Aldwin C, Stokols D. The effects of environmental change on individuals and groups: some neglected issues in stress research. J Environ Psychol. 1988; 8:57–75.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Associations Between Conventional Healthy Behaviors and Social Distancing During the COVID-19 Pandemic: Evidence From the 2020 Community Health Survey in Korea
- Comparison of Oral Health Promotion and Dementia Prevention Behavior according to the Perception Level on the Relationship between Them
- Changes in cardiovascular-related health behaviors during the COVID-19 pandemic
- Suicide and Suicide Prevention Awareness in Korea During the COVID-19 Pandemic
- Metabolic syndrome awareness in the general Korean population: results from a nationwide survey