Cardiovasc Prev Pharmacother.
2023 Jan;5(1):15-23. 10.36011/cpp.2023.5.e2.
Changes in cardiovascular-related health behaviors during the COVID-19 pandemic
- Affiliations
-
- 1Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Soonchunhyang University College of Medicine, Asan, Korea
- 3Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea
- 4Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
- 5Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 6Department of Neurology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
- 7Center of Biomedical Data Science, Yonsei University Wonju College of Medicine, Wonju, Korea
- 8Department of Health Promotion Medicine, Ewha Womans University College of Medicine, Seoul, Korea
- 9Division of Endocrinology and Metabolism, Department of Internal Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2540036
- DOI: http://doi.org/10.36011/cpp.2023.5.e2
Abstract
- Background
The COVID-19 pandemic has been the most pressing health challenge in recent years. Meanwhile, prevention for other diseases, such as cardiovascular disease (CVD) has been less prioritized during the pandemic. COVID-19, a novel infectious disease, both had a direct impact on public health and provoked changes in health-related behaviors, including those for CVD prevention. This study sought to examine changes in CVD-related health behaviors during the COVID-19 pandemic and related sociodemographic factors.
Methods
We used data from the Cardiovascular Disease Prevention Awareness Survey conducted in Korea in June 2022. A total of 2,000 adults across Korea’s 17 provinces completed a structured questionnaire online or on a mobile device. Self-reported changes in CVD-related health behaviors were investigated. We used unadjusted and adjusted logistic regression models to explore the associations between negative changes and sociodemographic factors.
Results
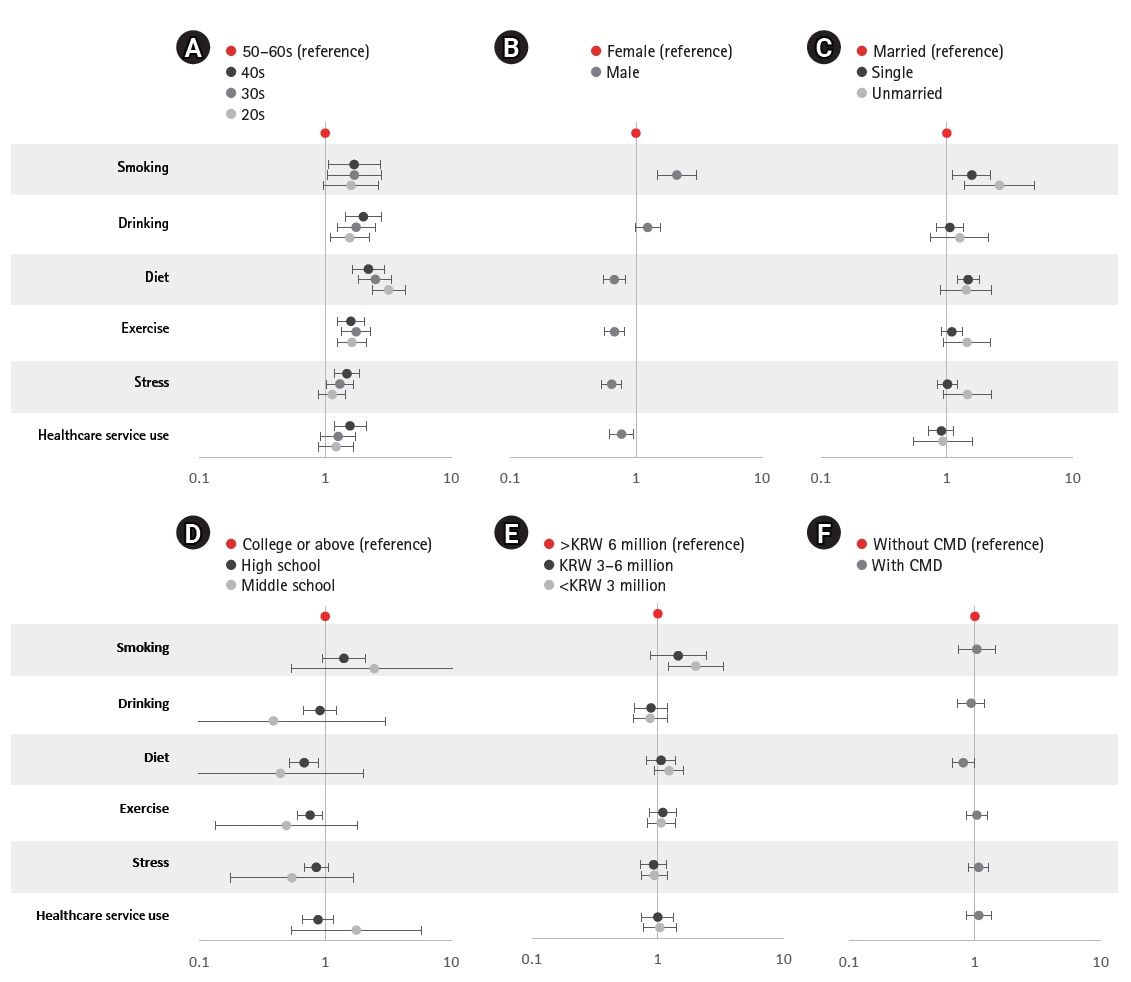
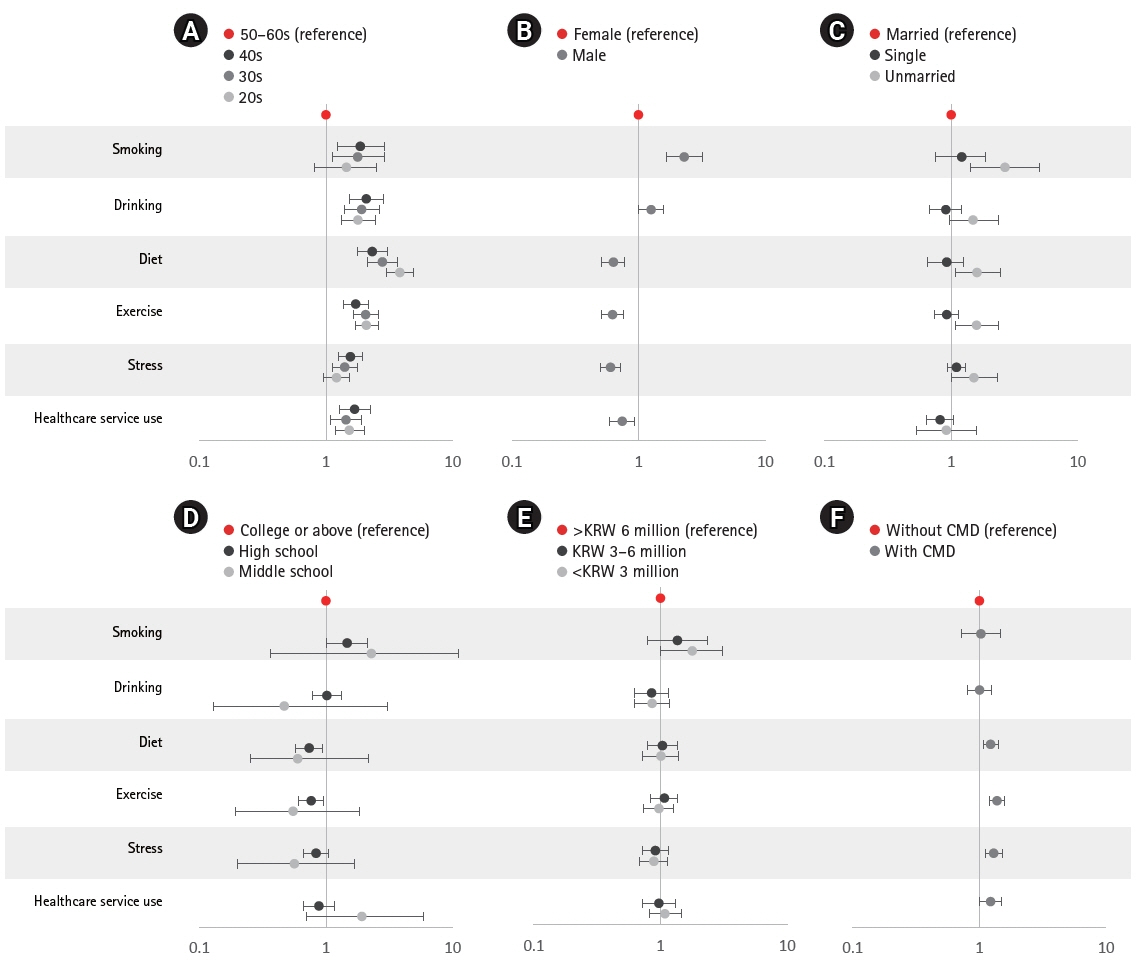
In smoking, drinking, and healthcare service use, the proportion of those with positive changes surpassed the proportion of respondents who reported negative changes. In contrast, negative changes predominated for diet, exercise, and stress. Most individuals (52.6%) reported a deterioration of psychological distress. These negative changes were significantly associated with age, sex, marital status, and the presence of cardiometabolic disease.
Conclusions
The COVID-19 pandemic has affected CVD-related health behaviors. Based on these changes, CVD prevention should be encouraged with appropriate and prioritized strategies.
Figure
Cited by 1 articles
-
Changes in cardiovascular-related health behaviors after the end of social distancing: the 2023 Cardiovascular Disease Prevention Awareness Survey
Jaeyong Lee, Eunji Kim, Won-Young Lee, Eun-Jung Rhee, Hyeon Chang Kim
Cardiovasc Prev Pharmacother. 2024;6(2):57-64. doi: 10.36011/cpp.2024.6.e6.
Reference
-
1. Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions: United States, January-May 2020. MMWR Morb Mortal Wkly Rep. 2020; 69:795–800.2. Razavi AC, Kelly TN, He J, Fernandez C, Whelton PK, Krousel-Wood M, et al. Cardiovascular disease prevention and implications of coronavirus disease 2019: an evolving case study in the crescent city. J Am Heart Assoc. 2020; 9:e016997.3. Duffy EY, Cainzos-Achirica M, Michos ED. Primary and secondary prevention of cardiovascular disease in the era of the coronavirus pandemic. Circulation. 2020; 141:1943–5.4. Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020; 75:2871–2.5. De Filippo O, D'Ascenzo F, Angelini F, Bocchino PP, Conrotto F, Saglietto A, et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020; 383:88–9.6. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018; 392:1736–88.7. Statistics Korea. Causes of death statistics in 2020. Statistics Korea; 2021.8. Arafa A, Lee HH, Eshak ES, Shirai K, Liu K, Li J, et al. Modifiable risk factors for cardiovascular disease in Korea and Japan. Korean Circ J. 2021; 51:643–55.9. Yang J, Zheng Y, Gou X, Pu K, Chen Z, Guo Q, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis. 2020; 94:91–5.10. Korea Disease Control and Prevention Agency (KDCA). Chronic disease prevention and management [Internet]. KDCA; 2022 [cited 2022 Jul 29]. Available from: https://www.kdca.go.kr/contents.es?mid=a20303020300.11. Metzler B, Siostrzonek P, Binder RK, Bauer A, Reinstadler SJ. Decline of acute coronary syndrome admissions in Austria since the outbreak of COVID-19: the pandemic response causes cardiac collateral damage. Eur Heart J. 2020; 41:1852–3.12. Dzaye O, Adelhoefer S, Boakye E, Blaha MJ. Cardiovascular-related health behaviors and lifestyle during the COVID-19 pandemic: an infodemiology study. Am J Prev Cardiol. 2021; 5:100148.13. Knell G, Robertson MC, Dooley EE, Burford K, Mendez KS. Health behavior changes during COVID-19 pandemic and subsequent "Stay-at-Home" orders. Int J Environ Res Public Health. 2020; 17:6268.14. Vardavas CI, Nikitara K. COVID-19 and smoking: a systematic review of the evidence. Tob Induc Dis. 2020; 18:20.15. Lim S, Lim H, Despres JP. Collateral damage of the COVID-19 pandemic on nutritional quality and physical activity: perspective from South Korea. Obesity (Silver Spring). 2020; 28:1788–90.16. Kim MH, Yeon JY. Change of dietary habits and the use of home meal replacement and delivered foods due to COVID-19 among college students in Chungcheong province, Korea. J Nutr Health. 2021; 54:383–97.17. Lakhan R, Agrawal A, Sharma M. Prevalence of depression, anxiety, and stress during COVID-19 pandemic. J Neurosci Rural Pract. 2020; 11:519–25.18. Stanton R, To QG, Khalesi S, Williams SL, Alley SJ, Thwaite TL, et al. Depression, anxiety and stress during COVID-19: associations with changes in physical activity, sleep, tobacco and alcohol use in Australian adults. Int J Environ Res Public Health. 2020; 17:4065.19. Papageorge NW, Zahn MV, Belot M, van den Broek-Altenburg E, Choi S, Jamison JC, et al. Socio-demographic factors associated with self-protecting behavior during the Covid-19 pandemic. J Popul Econ. 2021; 34:691–738.20. Yan AF, Sun X, Zheng J, Mi B, Zuo H, Ruan G, et al. Perceived risk, behavior changes and health-related outcomes during COVID-19 pandemic: findings among adults with and without diabetes in China. Diabetes Res Clin Pract. 2020; 167:108350.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Nurses’ healthy behaviors during the COVID-19 pandemic and related factors
- Psychological Predictors of Anxious Responses to the COVID-19 Pandemic: Evidence from Pakistan
- Assessment and Management of Dysphagia during the COVID-19 Pandemic
- Comparison of health behaviors of adult women in Korea before and during the COVID-19 pandemic: secondary analysis of the Korea National Health and Nutrition Examination Survey 2019–2020
- Prevalence and associated factors of prenatal depression in pregnant Korean women during the COVID-19 pandemic: a cross-sectional study