J Yeungnam Med Sci.
2024 Apr;41(2):120-127. 10.12701/jyms.2024.00087.
Optimal examination for traumatic nerve/muscle injuries in earthquake survivors: a retrospective observational study
- Affiliations
-
- 1Department of Physical and Rehabilitation Medicine, Hacettepe University Medical School, Ankara, Turkey
- KMID: 2554773
- DOI: http://doi.org/10.12701/jyms.2024.00087
Abstract
- Background
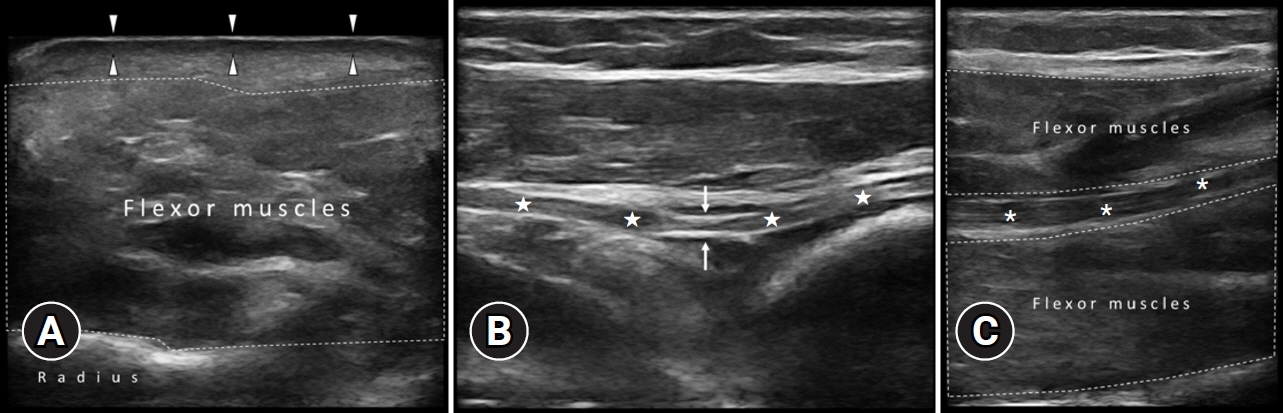
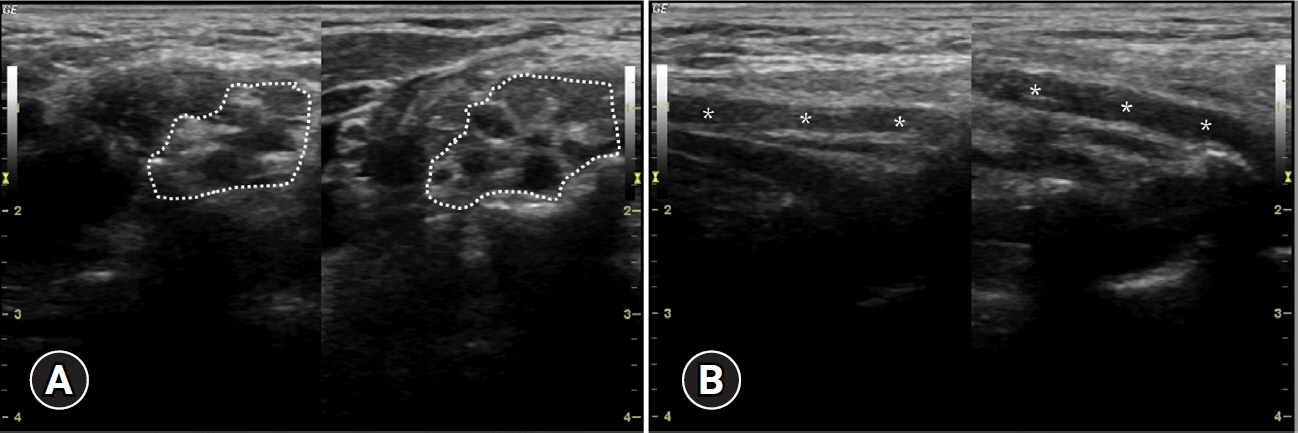
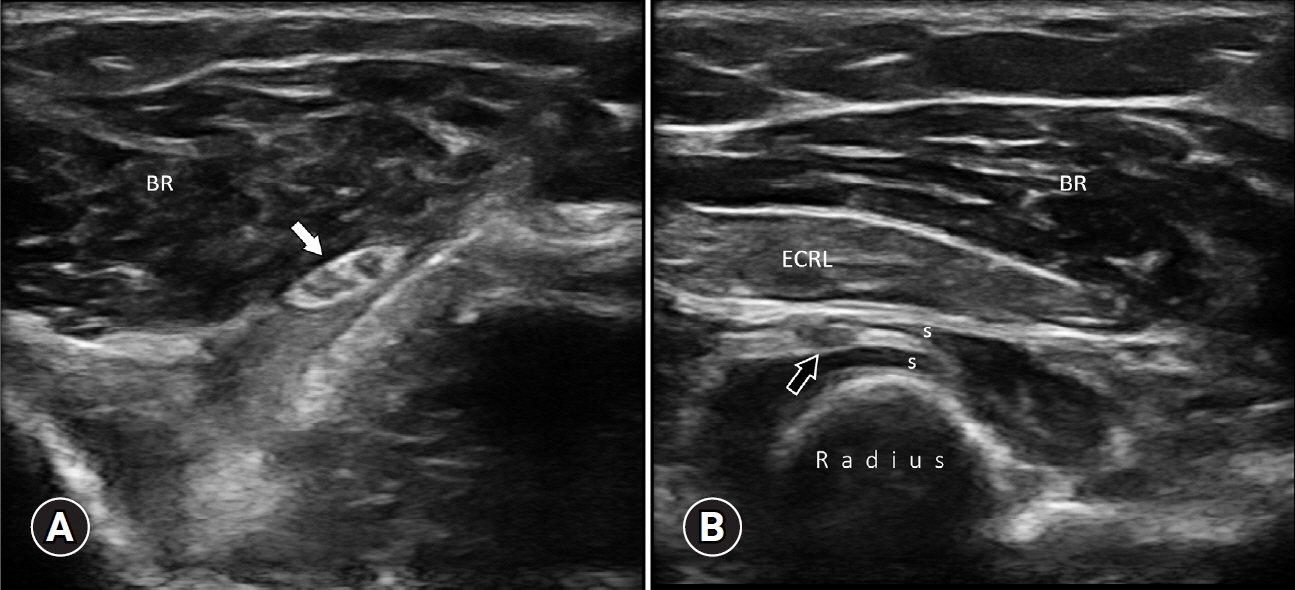
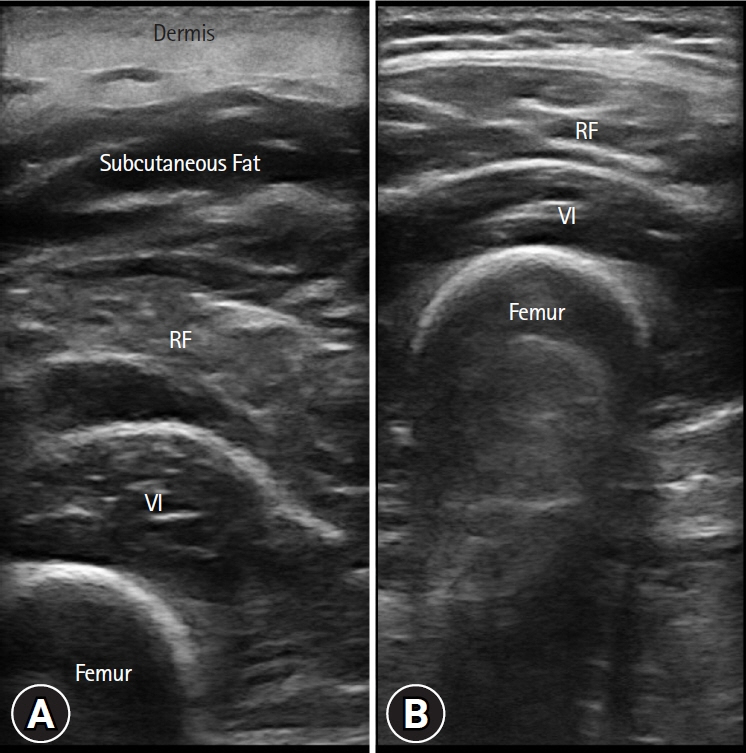
Physiatrists are facing with survivors from disasters in both the acute and chronic phases of muscle and nerve injuries. Similar to many other clinical conditions, neuromusculoskeletal ultrasound can play a key role in the management of such cases (with various muscle/nerve injuries) as well. Accordingly, in this article, a recent single-center experience after the Turkey-Syria earthquake will be rendered.
Methods
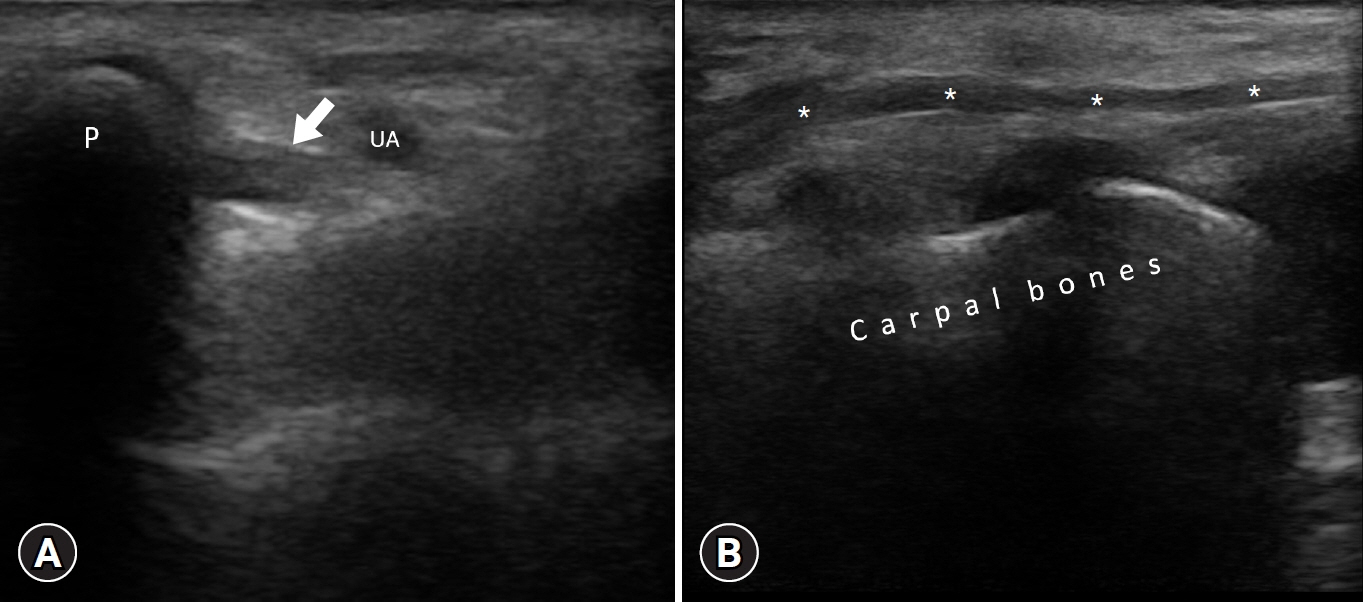
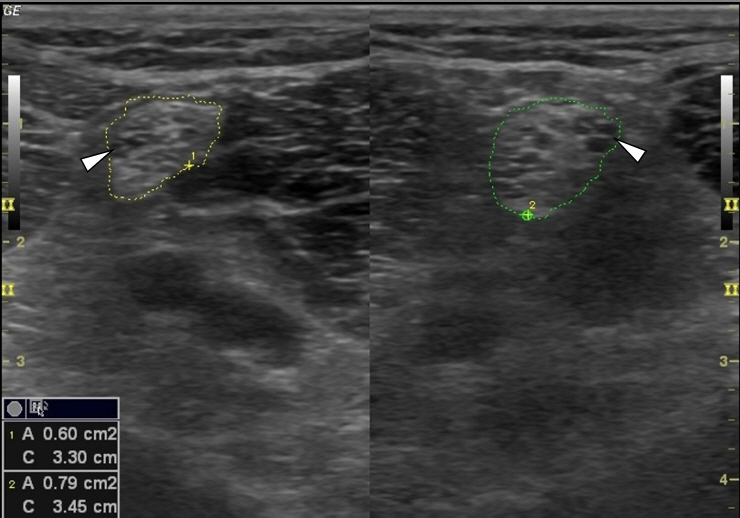
Ultrasound examinations were performed for various nerve/muscle lesions in 52 earthquake victims referred from different cities. Demographic features, type of injuries, and applied treatment procedures as well as detailed ultrasonographic findings are illustrated.
Results
Of the 52 patients, 19 had incomplete peripheral nerve lesions of the brachial plexus (n=4), lumbosacral plexus (n=1), and upper and lower limbs (n=14).
Conclusion
The ultrasonographic approach during disaster relief is paramount as regards subacute and chronic phases of rehabilitation. Considering technological advances (e.g., portable machines), the use of on-site ultrasound examination in the (very) early phases of disaster response also needs to be on the agenda of medical personnel.
Keyword
Figure
Reference
-
References
1. Khan F, Amatya B, Gosney J, Rathore FA, Burkle FM Jr. Medical rehabilitation in natural disasters: a review. Arch Phys Med Rehabil. 2015; 96:1709–27.
Article2. Amatya B, Galea M, Li J, Khan F. Medical rehabilitation in disaster relief: towards a new perspective. J Rehabil Med. 2017; 49:620–8.
Article3. Dal Zilio L, Ampuero JP. Earthquake doublet in Turkey and Syria. Commun Earth Environ. 2023; 4:71.
Article4. Wikipedia contributors. 2023 Turkey-Syria earthquake [Internet]. Wikipedia, The Free Encyclopedia;2023. Apr. 26. [cited 2024 Jan 25]. https://en.wikipedia.org/w/index.php?title=2023_Turkey%E2%80%93Syria_earthquake&oldid=1151836296.5. Ricci V, Ricci C, Cocco G, Gervasoni F, Donati D, Farì G, et al. Histopathology and high-resolution ultrasound imaging for peripheral nerve (injuries). J Neurol. 2022; 269:3663–75.
Article6. Chang KV, Wu WT, Özçakar L. Ultrasound ımaging and rehabilitation of muscle disorders: Part 1. Traumatic ınjuries. Am J Phys Med Rehabil. 2019; 98:1133–41.
Article7. Feger J, Bell D. Muscle contusion [Internet]. Radiopaedia.org;[cited 2024 Mar 7]. https://doi.org/10.53347/rID-82383.
Article8. Ricci V, Özçakar L. Life after ultrasound: are we speaking the same (or a new) language in Physical and Rehabilitation Medicine? J Rehabil Med. 2019; 51:234–5.
Article9. Özçakar L, Ricci V, Chang KV, Mezian K, Kara M. Musculoskeletal ultrasonography: ninety-nine reasons for physiatrists. Med Ultrason. 2022; 24:137–9.
Article10. Baloch N, Hasan OH, Jessar MM, Hattori S, Yamada S. “Sports Ultrasound”, advantages, indications and limitations in upper and lower limbs musculoskeletal disorders: review article. Int J Surg. 2018; 54(Pt B):333–40.
Article11. Cocco G, Ricci V, Villani M, Delli Pizzi A, Izzi J, Mastandrea M, et al. Ultrasound imaging of bone fractures. Insights Imaging. 2022; 13:189.
Article12. Menorca RM, Fussell TS, Elfar JC. Nerve physiology: mechanisms of injury and recovery. Hand Clin. 2013; 29:317–30.13. Rathore FA, Gosney JE, Reinhardt JD, Haig AJ, Li J, DeLisa JA. Medical rehabilitation after natural disasters: why, when, and how? Arch Phys Med Rehabil. 2012; 93:1875–81.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Patterns of Depression and Resilience in Children and Adolescents Exposed to an Earthquake: A Latent Profile Analysis
- Earthquake-related Crush Injury versus Non-Earthquake Injury in Abdominal Trauma Patients on Emergency Multidetector Computed Tomography: A Comparative Study
- Associated Injuries and Prognosis in Traumatic Isolated 3rd, 4th, and 6th Cranial Nerve Palsies
- Psychological Distress and Health-related Quality of Life in Relocated and Nonrelocated Older Survivors after the 2008 Sichuan Earthquake
- Diagnostic Usefulness of Neuromuscular Ultrasound in Anatomical Localization of Peripheral Nerve Injury: Detailed Lesion Localization Using Neuromuscular Ultrasound in a Patient with Traumatic Ulnar Nerve Injury at the Hand