Ann Pediatr Endocrinol Metab.
2024 Apr;29(2):119-129. 10.6065/apem.2346122.061.
Predictive factors of bone strength variation in adolescent girls according to body composition
- Affiliations
-
- 1School of Medicine, Walailak University, Nakhonsithammarat, Thailand
- KMID: 2554683
- DOI: http://doi.org/10.6065/apem.2346122.061
Abstract
- Purpose
This study examined correlations among anthropometric parameters, body composition, bone parameters and predictive factors of bone mass in adolescent girls with different body fat percentages (%fat).
Methods
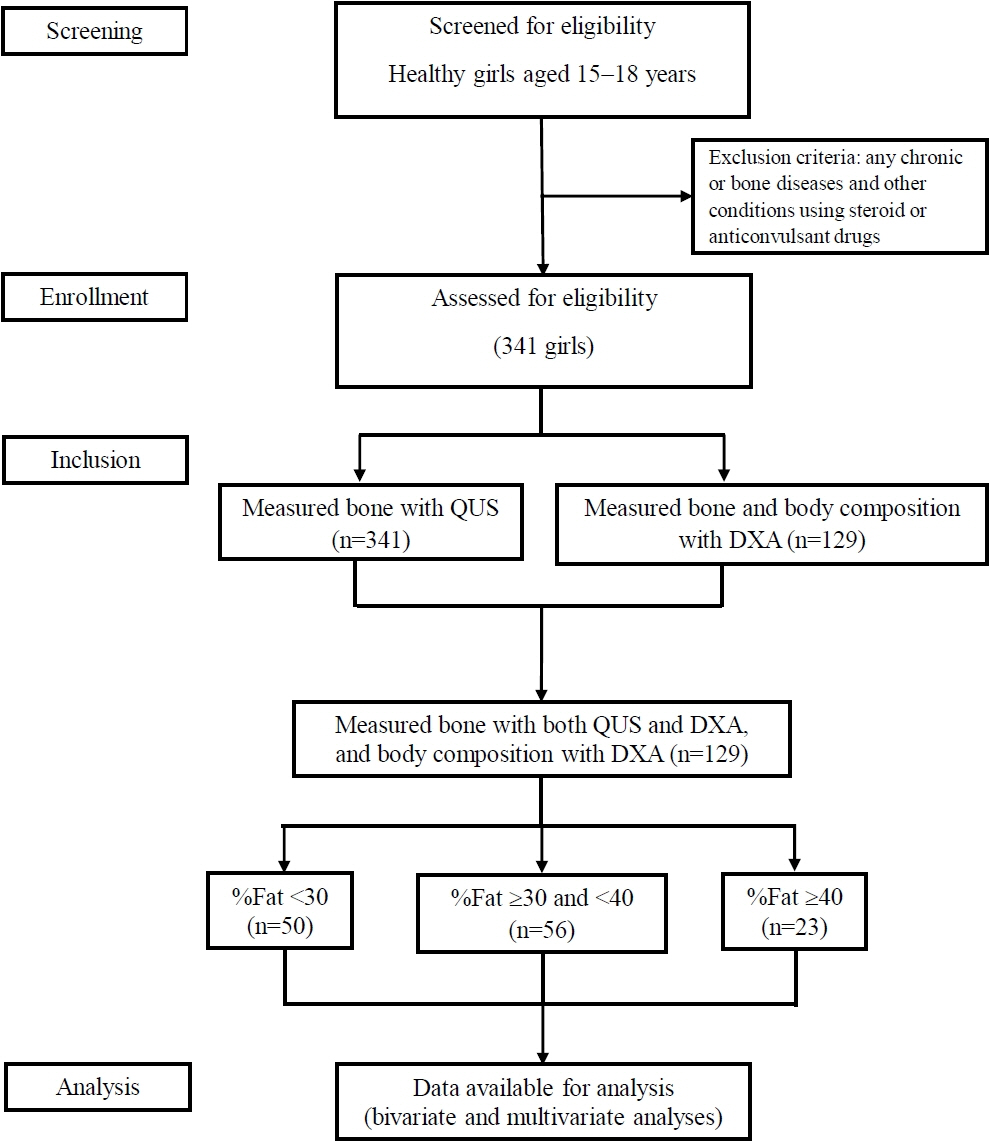
A total of 129 females aged 15–18 years were categorized into 3 groups using %fat-for-age at the 50th and 95th percentiles as cutoff points (normal, over, and excess %fat groups). We recorded anthropometric data and measured the speed of sound at the tibia and radius using quantitative ultrasound. Dual-energy x-ray absorptiometry (DXA) was used to measure body composition and bone parameters, including bone mineral density (BMD), bone mineral content (BMC), and the BMD-z-score (z-score) in the lumbar spine (LS) and whole body (WB). These parameters were compared among the 3 groups using bivariate and multivariate correlation analyses.
Results
There were strong correlations among all anthropometric parameters, body composition, and DXA in the over %fat group. Lean parameters strongly correlated with LS and WB in the normal %fat group, whereas both lean mass (LM) and fat mass (FM) were positively correlated with BMC in the excess %fat group. The predictive factors of bone mass differed among the groups, as follows: lean body mass was predictive of BMD and BMC at both sites in the normal and over %fat groups; LM and body weight were predictive of LS-BMC and WB-bones, respectively, in the over %fat group; and FM was predictive of WB-bones in the excess %fat group. Body fat and waist circumference were negative predictors of bone mass.
Conclusion
Predictive factors of bone strength appear to depend on the amount of body fat in adolescent girls.
Keyword
Figure
Reference
-
References
1. Mazidi M, Banach M, Kengne AP. Prevalence of childhood and adolescent overweight and obesity in Asian countries: a systematic review and meta-analysis. Arch Med Sci. 2018; 14:1185–203.2. de Onis M, Onyango AW, Borghi E, Siyam A, Nishida C, Siekmann J. Development of a WHO growth reference for school-aged children and adolescents. Bull World Health Organ. 2007; 85:660–7.
Article3. Puwanant M, Mo-Suwan L, Jaruratanasirikul S, Jessadapakorn W. Body-fat-percentile curves for Thai children and adolescents. Nutrients. 2023; 15:448.4. de Morais NS, Azevedo FM, de Freitas Rocha AR, Morais DC, Ribeiro SAV, Gonçalves VSS, et al. Body fat is superior to body mass index in predicting cardiometabolic risk factors in adolescents. Int J Environ Res Public Health. 2023; 20:2074.5. Cota BC, Suhett LG, Leite NN, Pereira PF, Ribeiro SAV, Franceschini S. Cardiometabolic risk and health behaviours in adolescents with normal-weight obesity: a systematic review. Public Health Nutr. 2021; 24:870–81.6. Sung RY, So HK, Choi KC, Li AM, Yin J, Nelson EA. Body fat measured by bioelectrical impedance in Hong Kong Chinese children. Hong Kong Med J. 2009; 15:110–7.7. Achamrah N, Colange G, Delay J, Rimbert A, Folope V, Petit A, et al. Comparison of body composition assessment by DXA and BIA according to the body mass index: a retrospective study on 3655 measures. PLoS One. 2018; 13:e0200465.8. Marra M, Sammarco R, De Lorenzo A, Iellamo F, Siervo M, Pietrobelli A, et al. Assessment of body composition in health and disease using bioelectrical impedance analysis (BIA) and dual energy X-Ray absorptiometry (DXA): a critical overview. Contrast Media Mol Imaging. 2019; 2019:3548284.9. Lee K, Lee S, Kim SY, Kim SJ, Kim YJ. Percent body fat cutoff values for classifying overweight and obesity recommended by the International Obesity Task Force (IOTF) in Korean children. Asia Pac J Clin Nutr. 2007; 16:649–55.10. Dong H, Yan Y, Liu J, Cheng H, Zhao X, Shan X, et al. Reference centiles for evaluating total body fat development and fat distribution by dual-energy x-ray absorptiometry among children and adolescents aged 3-18 years. Clin Nutr. 2021; 40:1289–95.11. Cao JJ. Effects of obesity on bone metabolism. J Orthop Surg Res. 2011; 6:30.12. Faienza MF, D'Amato G, Chiarito M, Colaianni G, Colucci S, Grano M, et al. Mechanisms involved in childhood obesity-related bone fragility. Front Endocrinol. 2019; 10:269.13. Fintini D, Cianfarani S, Cofini M, Andreoletti A, Ubertini GM, Cappa M, et al. The bones of children with obesity. Front Endocrinol. 2020; 11:200.14. Kessler J, Koebnick C, Smith N, Adams A. Childhood obesity is associated with increased risk of most lower extremity fractures. Clin Orthop Relat Res. 2013; 471:1199–207.15. Mo Y, Wang D. Clinical and epidemiological features of tibial tubercle avulsion fracture in Chinese adolescents. World J Pediatr Surg. 2020; 3:e000169.16. Franceschi R, Radetti G, Soffiati M, Maines E. Forearm fractures in overweight-obese children and adolescents: a matter of bone density, bone geometry or body composition? Calcif Tissue Int. 2022; 111:107–15.17. Duque G. Bone and fat connection in aging bone. Curr Opin Rheumatol. 2008; 20:429–34.18. Yao W, Luo J, Ao L, Cheng H, Lu S, Liu J, et al. Association of total body fat and fat distribution with bone mineral density among children and adolescents aged 6-17 years from Guangzhou, China. Eur J Pediatr. 2023; 182:1115–26.19. Gállego Suárez C, Singer BH, Gebremariam A, Lee JM, Singer K. The relationship between adiposity and bone density in U.S. children and adolescents. PLoS One. 2017; 12:e0181587.20. Deng KL, Li H, Yang WY, Hou JL, Xu Y, Xiao SM. Analysis of the association between fat mass distribution and bone mass in Chinese male adolescents at different stages of puberty. Nutrients. 2021; 13:2163.21. Jeddi M, Ardalan A, Heydari ST, Dabbaghmanesh MH. Non-linear association of body composition and its components with bone density in Iranian children and adolescents. Arch Osteoporos. 2021; 16:77.22. Kim HY, Jung HW, Hong H, Kim JH, Shin CH, Yang SW, et al. The role of overweight and obesity on bone health in Korean adolescents with a focus on lean and fat mass. J Korean Med Sci. 2017; 32:1633–41.23. López-Peralta S, Romero-Velarde E, Vásquez-Garibay EM, González-Hita M, Robles-Robles LC, Ruiz-González FJ, et al. Bone mineral density and body composition in normal weight, overweight and obese children. BMC Pediatr. 2022; 22:249.24. Winther A, Jørgensen L, Ahmed LA, Christoffersen T, Furberg AS, Grimnes G, et al. Bone mineral density at the hip and its relation to fat mass and lean mass in adolescents: the Tromsø Study, Fit Futures. BMC Musculoskelet Disord. 2018; 19:21.25. Duran I, Martakis K, Hamacher S, Stark C, Semler O, Schoenau E. Are there effects of age, gender, height, and body fat on the functional muscle-bone unit in children and adults? Osteoporos Int. 2018; 29:1069–79.26. Khwanchuea R, Punsawad C. Association between anthropometric indices, body composition and bone parameters in Thai female adolescents. Indian J Pediatr. 2017; 84:908–14.
Article27. Zadik Z, Price D, Diamond G. Pediatric reference curves for multi-site quantitative ultrasound and its modulators. Osteoporos Int. 2003; 14:857–62.28. Rivas-Ruiz R, Méndez-Sánchez L, Castelán-Martínez OD, Clark P, Tamayo J, Talavera JO, et al. Comparison of international reference values for bone speed of sound in pediatric populations: meta-analysis. J Clin Densitom. 2016; 19:316–25.
Article29. Williams KD, Blangero J, Mahaney MC, Subedi J, Jha B, Williams-Blangero S, et al. Axial quantitative ultrasound assessment of pediatric bone quality in eastern Nepal. Osteoporos Int. 2015; 26:2319–28.30. Nalda E, Mahadea KK, Dematteï C, Kotzki PO, Pouget JP, Boudousq V. Assessment of the Stratos, a new pencil-beam bone densitometer: dosimetry, precision, and cross calibration. J Clin Densitom. 2011; 14:395–406.31. Binkovitz LA, Henwood MJ. Pediatric DXA: technique and interpretation. Pediatr Radiol. 2007; 37:21–31.32. McGregor PC, Lyons MM, Wozniak A, Linko K, Fishman F, Cappello T. The effect of obesity on pediatric tibia fractures. Iowa Orthop J. 2022; 42:41–6.33. Falk B, Bronshtein Z, Zigel L, Constantini NW, Eliakim A. Quantitative ultrasound of the tibia and radius in prepubertal and early-pubertal female athletes. Arch Pediatr Adolesc Med. 2003; 157:139–43.34. Eliakim A, Nemet D, Wolach B. Quantitative ultrasound measurements of bone strength in obese children and adolescents. J Pediatr Endocrinol Metab. 2001; 14:159–64.35. Nguyen HG, Pham MT, Ho-Pham LT, Nguyen TV. Lean mass and peak bone mineral density. Osteoporos Sarcopenia. 2020; 6:212–6.
Article36. Baptista F, Barrigas C, Vieira F, Santa-Clara H, Homens PM, Fragoso I, et al. The role of lean body mass and physical activity in bone health in children. J Bone Miner Metab. 2012; 30:100–8.
Article37. Sioen I, Lust E, De Henauw S, Moreno LA, Jiménez-Pavón D. Associations between body composition and bone health in children and adolescents: a systematic review. Calcif Tissue Int. 2016; 99:557–77.38. Schoenau E. From mechanostat theory to development of the "Functional Muscle-Bone-Unit". J Musculoskelet Neuronal Interact. 2005; 5:232–8.39. Torres-Costoso A, López-Muñoz P, Martínez-Vizcaíno V, Álvarez-Bueno C, Cavero-Redondo I. Association between muscular strength and bone health from children to young adults: a systematic review and meta-analysis. Sports Med. 2020; 50:1163–90.40. Khalid AB, Krum SA. Estrogen receptors alpha and beta in bone. Bone. 2016; 87:130–5.
Article41. Rinonapoli G, Pace V, Ruggiero C, Ceccarini P, Bisaccia M, Meccariello L, et al. Obesity and bone: a complex relationship. Int J Mol Sci. 2021; 22:13662.
Article42. Hetherington-Rauth M, Bea JW, Blew RM, Funk JL, Hingle MD, Lee VR, et al. Relative contributions of lean and fat mass to bone strength in young Hispanic and non-Hispanic girls. Bone. 2018; 113:144–50.
Article43. Pereira-da-Silva L, Dias MP, Dionísio E, Virella D, Alves M, Diamantino C, et al. Fat mass index performs best in monitoring management of obesity in prepubertal children. J Pediatr. 2016; 92:421–6.
Article44. Zhu X, Zheng H. Factors influencing peak bone mass gain. Front Med. 2021; 15:53–69.
Article45. Clarke BL, Khosla S. Female reproductive system and bone. Arch Biochem Biophys. 2010; 503:118–28.
Article46. Eastell R. Role of oestrogen in the regulation of bone turnover at the menarche. J Endocrinol. 2005; 185:223–34.47. Itriyeva K. The effects of obesity on the menstrual cycle. Curr Probl Pediatr Adolesc Health Care. 2022; 52:101241.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Body Composition Analysis in Newly Diagnosed Diabetic Adolescent Girls
- Body Composition Changes in Korean Children and Adolescents
- Effects of Body Composition, Leptin, and Adiponectin on Bone Mineral Density in Prepubertal Girls
- Comparisons of 12 Week Combined Exercise Intervention-mediated Changes of Body Composition, Physical Fitness, and Metabolic Syndrome Risk Factors According to IGF-I Gene Polymorphism in Obese Adolescent Boys
- Changes of Bone Metabolic Markers after Exercise Training in 70's Elderly Women