J Korean Med Sci.
2024 Mar;39(11):e102. 10.3346/jkms.2024.39.e102.
Validation of the Pandemic Grief Risk Factors and Its Relationship With Work-Related Stress and Grief Reaction Among Healthcare Workers Who Witnessed Patient Deaths
- Affiliations
-
- 1Department of Psychiatry, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Digital Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 3Department of Psychology, University of Chittagong, Chattogram, Bangladesh
- 4National Centre for Epidemiology and Population Health, Australian National University, Canberra, Australia
- 5Department of Psychology, Christopher Newport University, Newport News, VA, USA
- KMID: 2554201
- DOI: http://doi.org/10.3346/jkms.2024.39.e102
Abstract
- Background
The Pandemic Grief Risk Factors (PGRFs) was developed as a self-report tool to compile a comprehensive list of unique risk factors related to grief when experiencing a coronavirus disease 2019 (COVID-19) loss. We explored the reliability and validity of the PGRF among healthcare workers who witnessed their patients’ deaths during the COVID-19 pandemic. Further, we examined whether the general severity of PGRF may have been associated with work-related stress and pandemic grief reactions.
Methods
An online survey was conducted among tertiary hospital healthcare workers (doctors and nursing professionals) who had witnessed the deaths of patients they cared for. Pandemic Grief Scale for healthcare workers, the Stress and Anxiety to Viral Epidemics-3 items, the Patient Health Questionnaire-9, and the Generalized Anxiety Disorder-7 responses were collected.
Results
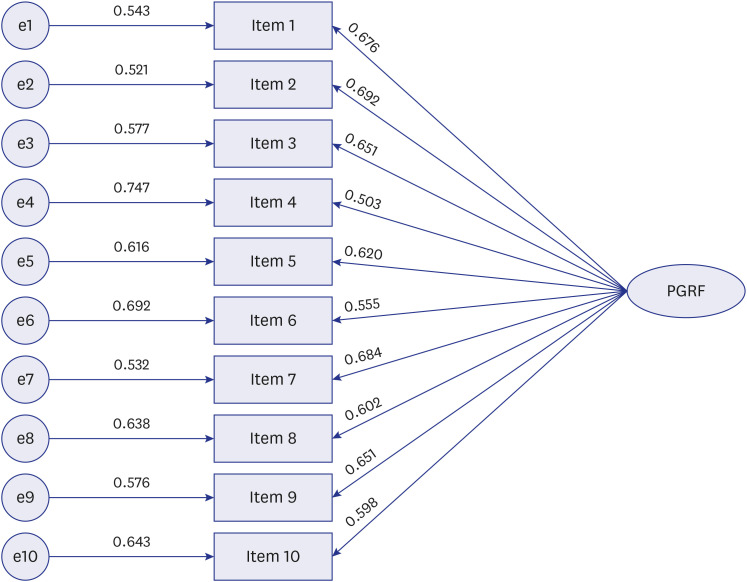
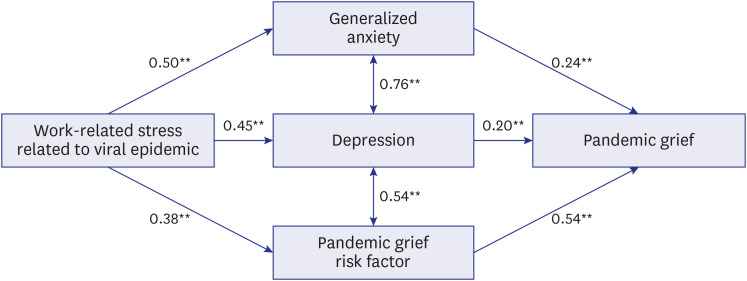
In total, 267 responses were analyzed. The single-factor structure of the Korean version of the PGRF showed a good fit for the model. The scale demonstrated good internal consistency and convergent validity with other depression and anxiety rating scales. The mediation analysis revealed that work-related stress directly influenced pandemic grief reactions positively, and depression, anxiety, and general severity of grief risk factors partially mediated the association positively.
Conclusion
Among healthcare workers who witnessed the deaths of their patients due to COVID-19, the Korean version of the PGRF was valid and reliable for measuring the overall severity of PGRF. The PGRF can be used to identify individuals at risk for dysfunctional grief.
Figure
Reference
-
1. World Health Organization. WHO COVID-19 dashboard. Updated 2023. Accessed August 21, 2023. https://covid19.who.int/ .2. Xiong J, Lipsitz O, Nasri F, Lui LM, Gill H, Phan L, et al. Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J Affect Disord. 2020; 277:55–64. PMID: 32799105.3. Salari N, Hosseinian-Far A, Jalali R, Vaisi-Raygani A, Rasoulpoor S, Mohammadi M, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Global Health. 2020; 16(1):57. PMID: 32631403.4. Uphoff EP, Lombardo C, Johnston G, Weeks L, Rodgers M, Dawson S, et al. Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreaks: a rapid systematic review. PLoS One. 2021; 16(8):e0254821. PMID: 34347812.5. Saragih ID, Tonapa SI, Saragih IS, Advani S, Batubara SO, Suarilah I, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nurs Stud. 2021; 121:104002. PMID: 34271460.6. Dragioti E, Tsartsalis D, Mentis M, Mantzoukas S, Gouva M. Impact of the COVID-19 pandemic on the mental health of hospital staff: an umbrella review of 44 meta-analyses. Int J Nurs Stud. 2022; 131:104272. PMID: 35576637.7. Eisma MC, Tamminga A, Smid GE, Boelen PA. Acute grief after deaths due to COVID-19, natural causes and unnatural causes: an empirical comparison. J Affect Disord. 2021; 278:54–56. PMID: 32950843.8. Boelen PA, Lenferink LI. Symptoms of prolonged grief, posttraumatic stress, and depression in recently bereaved people: symptom profiles, predictive value, and cognitive behavioural correlates. Soc Psychiatry Psychiatr Epidemiol. 2020; 55(6):765–777. PMID: 31535165.9. Bonanno GA, Keltner D. Facial expressions of emotion and the course of conjugal bereavement. J Abnorm Psychol. 1997; 106(1):126–137. PMID: 9103724.10. Bonanno GA, Keltner D, Holen A, Horowitz MJ. When avoiding unpleasant emotions might not be such a bad thing: verbal-autonomic response dissociation and midlife conjugal bereavement. J Pers Soc Psychol. 1995; 69(5):975–989. PMID: 7473042.11. Rabow MW, Huang CS, White-Hammond GE, Tucker RO. Witnesses and victims both: healthcare workers and grief in the time of COVID-19. J Pain Symptom Manage. 2021; 62(3):647–656. PMID: 33556494.12. El Sayed S, Gomaa S, Aboelfotoh S, El Wasify M. Pandemic Grief Scale in detection of grief reaction among physicians in COVID-19 era. Middle East Curr Psychiatry. 2021; 28(1):1–8.13. Murata S, Rezeppa T, Thoma B, Marengo L, Krancevich K, Chiyka E, et al. The psychiatric sequelae of the COVID-19 pandemic in adolescents, adults, and health care workers. Depress Anxiety. 2021; 38(2):233–246. PMID: 33368805.14. Kustanti CY, Jen HJ, Chu H, Liu D, Chen R, Lin HC, et al. Prevalence of grief symptoms and disorders in the time of COVID-19 pandemic: a meta-analysis. Int J Ment Health Nurs. 2023; 32(3):904–916. PMID: 36880520.15. Rahmani F, Hosseinzadeh M, Gholizadeh L. Complicated grief and related factors among nursing staff during the Covid-19 pandemic: a cross-sectional study. BMC Psychiatry. 2023; 23(1):73. PMID: 36703151.16. Neimeyer RA, Lee SA. Circumstances of the death and associated risk factors for severity and impairment of COVID-19 grief. Death Stud. 2022; 46(1):34–42. PMID: 34019471.17. Lee SA, Neimeyer RA. Pandemic Grief Scale: a screening tool for dysfunctional grief due to a COVID-19 loss. Death Stud. 2022; 46(1):14–24. PMID: 33349159.18. Lee D, Kamaleddine I, Cho IK, Ahmed O, Cho E. Validation of the Stress and Anxiety to Viral Epidemics-9 (SAVE-9) scale and relationship with insomnia or depression among healthcare workers who witnessed patient’s death in COVID-19 pandemic. Sleep Med Rev. 2022; 13(3):158–164.19. Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ, USA: Lawrence Erlbaum;1988.20. Lee SA, Neimeyer RA. Pandemic Grief Scale for healthcare workers. Updated 2023. Accessed August 21, 2023. https://drive.google.com/file/d/1dHxW6k8YTWuR3NquLRwsxNr9DM1Fj83F/view .21. Kim JH, Park CH, Ahmed O, Hong Y, Chung S, Park J, et al. Validation of the healthcare workers’ version of the Pandemic Grief Scale among frontline nursing professionals during the COVID-19 pandemic in Korea. Front Psychiatry. 2023; 14:1121546. PMID: 37065896.22. Son HS, Ahn MH, Kim K, Cho IK, Lee J, Suh S, et al. Utility of the stress and anxiety to viral epidemic-3 items as a tool for assessing work-related stress, and relationship with insomnia and burnout of healthcare workers during the COVID-19 pandemic. Sleep Med Res. 2021; 12(2):161–168.23. Chung S, Kim HJ, Ahn MH, Yeo S, Lee J, Kim K, et al. Development of the stress and anxiety to viral epidemics-9 (SAVE-9) scale for assessing work-related stress and anxiety in healthcare workers in response to viral epidemics. J Korean Med Sci. 2021; 36(47):e319. PMID: 34873885.24. Spitzer RL, Kroenke K, Williams JB, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006; 166(10):1092–1097. PMID: 16717171.25. Patient Health Questionnaire-9. Updated 2023. Accessed August 21, 2023. https://www.phqscreeners.com/images/sites/g/files/g10060481/f/201412/PHQ9_Korean%20for%20Korea.pdf .26. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001; 16(9):606–613. PMID: 11556941.27. Brown T. Confirmatory Factor Analysis for Applied Research. New York, NY, USA: The Guilford Press;2006.28. Byrne BM. Structural equation modeling with AMOS, EQS, and LISREL: Comparative approaches to testing for the factorial validity of a measuring instrument. Int J Test. 2001; 1(1):55–86.29. Tennant C. Work-related stress and depressive disorders. J Psychosom Res. 2001; 51(5):697–704. PMID: 11728512.30. Melchior M, Caspi A, Milne BJ, Danese A, Poulton R, Moffitt TE. Work stress precipitates depression and anxiety in young, working women and men. Psychol Med. 2007; 37(8):1119–1129. PMID: 17407618.31. Hong J, Park CH, Kim H, Hong Y, Ahn J, Jun JY, et al. Grief response of nursing professionals is associated with their depression, loneliness, insomnia, and work-related stress while working in COVID-19 inpatients wards. Psychiatry Investig. 2023; 20(4):374–381.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Healthcare Workers and Patient Loss During the COVID-19 Pandemic: Interaction Between Grief, Viral Anxiety, and Depression
- Effect of a Brief Family-Based Treatment on Complicated Grief in Bereaved Older Adults
- Healing Through Loss: Exploring Nurses’ Post-Traumatic Growth After Patient Death
- Pandemic Grief Reaction and Intolerance of Uncertainty on the Cognitive-Behavioral Model of COVID-Related Hypochondriasis Among Firefighters
- Effects of Satisfaction with Social Support on Complicated Grief in Bereaved Dementia Caregivers