J Korean Diabetes.
2024 Mar;25(1):9-15. 10.4093/jkd.2024.25.1.9.
SGLT2 Inhibitors and Diabetes: Where Does It Come from and Where Does It Go?
- Affiliations
-
- 1Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- KMID: 2554116
- DOI: http://doi.org/10.4093/jkd.2024.25.1.9
Abstract
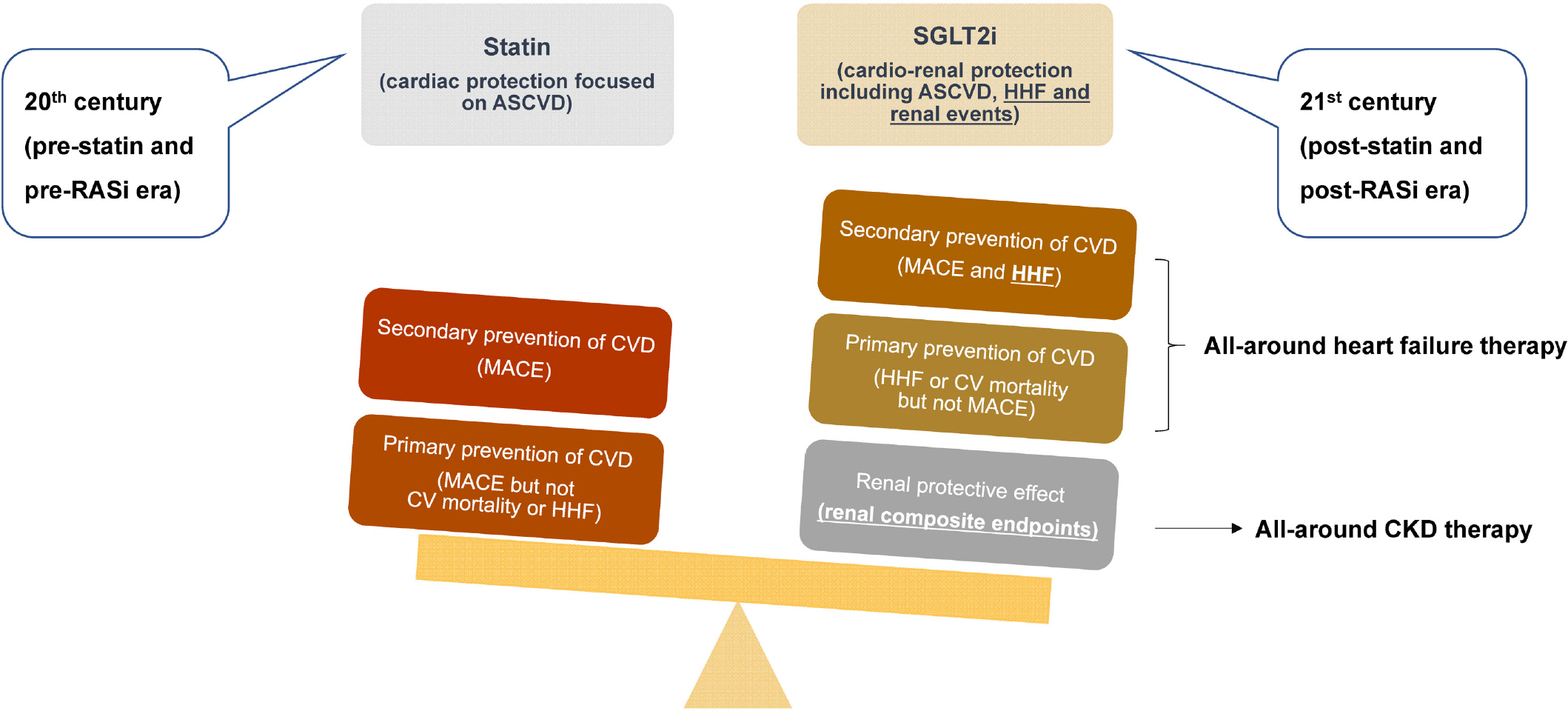
- Sodium glucose cotransporter 2 (SGLT2) inhibitors have emerged as powerful medications in the past decade. Numerous clinical trials have reported their cardio-renal protective effects and associated reductions in mortality. The beneficial effects of SGLT2 inhibitors in mediating heart failure and chronic kidney disease progression have been consistent across patients with and without diabetes regardless of ejection fraction. Therefore, SGLT2 inhibitors are not only antidiabetic drugs but also medications for heart failure and chronic kidney disease. However, adverse events such as genital infections and diabetic ketoacidosis should be considered. In this review, we explore the journey of SGLT2 inhibitors, often referred to as the “statins of the 21st century,” from their inception to the present day. We introduce the strengths and weaknesses of this medication and discuss unresolved issues that should be taken into considerations when prescribing SGLT2 inhibitors.
Keyword
Figure
Cited by 1 articles
-
Prevalence, Incidence, and Metabolic Characteristics of Young Adults with Type 2 Diabetes Mellitus in South Korea (2010–2020)
Ji Yoon Kim, Jiyoon Lee, Joon Ho Moon, Se Eun Park, Seung-Hyun Ko, Sung Hee Choi, Nam Hoon Kim
Diabetes Metab J. 2025;49(2):172-182. doi: 10.4093/dmj.2024.0826.
Reference
-
1.Kearney PM., Blackwell L., Collins R., Keech A., Simes J., Peto R, et al. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008. 371:117–25.
Article2.Baigent C., Keech A., Kearney PM., Blackwell L., Buck G., Pollicino C, et al. Efficacy and safety of cholesterol-low-ering treatment: prospective meta-analysis of data from 90,056 participants in 14 randomised trials of statins. Lancet. 2005. 366:1267–78.
Article3.Braunwald E. SGLT2 inhibitors: the statins of the 21st century. Eur Heart J. 2022. 43:1029–30.
Article4.Zinman B., Wanner C., Lachin JM., Fitchett D., Bluhmki E., Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015. 373:2117–28.
Article5.Wiviott SD., Raz I., Bonaca MP., Mosenzon O., Kato ET., Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019. 380:347–57.
Article6.Cannon CP., Pratley R., Dagogo-Jack S., Mancuso J., Huyck S., Masiukiewicz U, et al. Cardiovascular outcomes with ertugliflozin in type 2 diabetes. N Engl J Med. 2020. 383:1425–35.
Article7.Rådholm K., Figtree G., Perkovic V., Solomon SD., Mahaffey KW., de Zeeuw D, et al. Canagliflozin and heart failure in type 2 diabetes mellitus: results from the CANVAS program. Circulation. 2018. 138:458–68.
Article8.Kato ET., Silverman MG., Mosenzon O., Zelniker TA., Cahn A., Furtado RHM, et al. Effect of dapagliflozin on heart failure and mortality in type 2 diabetes mellitus. Circulation. 2019. 139:2528–36.
Article9.McMurray JJV., Solomon SD., Inzucchi SE., Køber L., Kosi-borod MN., Martinez FA, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019. 381:1995–2008.10.Anker SD., Butler J., Filippatos G., Ferreira JP., Bocchi E., Böhm M, et al. Empagliflozin in heart failure with a pre-served ejection fraction. N Engl J Med. 2021. 385:1451–61.11.Wanner C., Inzucchi SE., Zinman B. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016. 375:1801–2.
Article12.Heerspink HJL., Stefánsson BV., Correa-Rotter R., Chertow GM., Greene T., Hou FF, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020. 383:1436–46.
Article13.Herrington WG., Staplin N., Wanner C., Green JB., Hauske SJ., Emberson JR, et al. Empagliflozin in patients with chronic kidney disease. N Engl J Med. 2023. 388:117–27.
Article14.Packer M., Anker SD., Butler J., Filippatos G., Pocock SJ., Carson P, et al. Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med. 2020. 383:1413–24.15.McDonagh TA., Metra M., Adamo M., Gardner RS., Baum-bach A., Böhm M, et al. 2023 focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023. 44:3627–39.16.Navaneethan SD., Zoungas S., Caramori ML., Chan JCN., Heerspink HJL., Hurst C, et al. Diabetes management in chronic kidney disease: synopsis of the KDIGO 2022 clinical practice guideline update. Ann Intern Med. 2023. 176:381–7.
Article17.Jörgens V. The roots of SGLT inhibition: Laurent-Guil-laume de Koninck, Jean Servais Stas and Freiherr Josef von Mering. Acta Diabetol. 2019. 56:29–31.
Article18.Hediger MA., Turk E., Pajor AM., Wright EM. Molecular genetics of the human Na+/glucose cotransporter. Klin Wochenschr. 1989. 67:843–6.
Article19.Oku A., Ueta K., Arakawa K., Ishihara T., Nawano M., Kuro-numa Y, et al. T-1095, an inhibitor of renal Na+-glucose cotransporters, may provide a novel approach to treating diabetes. Diabetes. 1999. 48:1794–800.
Article20.Adachi T., Yasuda K., Okamoto Y., Shihara N., Oku A., Ueta K, et al. T-1095, a renal Na+-glucose transporter inhibitor, improves hyperglycemia in streptozotocin-induced dia-betic rats. Metabolism. 2000. 49:990–5.
Article21.Kim NH., Kim NH. Renoprotective mechanism of sodi-um-glucose cotransporter 2 inhibitors: focusing on renal hemodynamics. Diabetes Metab J. 2022. 46:543–51.
Article22.Dharia A., Khan A., Sridhar VS., Cherney DZI. SGLT2 inhibitors: the sweet success for kidneys. Annu Rev Med. 2023. 74:369–84.
Article23.Saucedo-Orozco H., Voorrips SN., Yurista SR., de Boer RA., Westenbrink BD. SGLT2 inhibitors and ketone metabo-lism in heart failure. J Lipid Atheroscler. 2022. 11:1–19.
Article24.Staels B. Cardiovascular protection by sodium glucose cotransporter 2 inhibitors: potential mechanisms. Am J Med. 2017. 130:S30–9.
Article25.Packer M. Critical reanalysis of the mechanisms underlying the cardiorenal benefits of SGLT2 inhibitors and reaf-firmation of the nutrient deprivation signaling/autophagy hypothesis. Circulation. 2022. 146:1383–405.
Article26.Zaccardi F., Webb DR., Htike ZZ., Youssef D., Khunti K., Da-vies MJ. Efficacy and safety of sodium-glucose co-trans-porter-2 inhibitors in type 2 diabetes mellitus: systematic review and network meta-analysis. Diabetes Obes Metab. 2016. 18:783–94.
Article27.Should all patients with type 2 diabetes mellitus and cardiovascular disease receive an SGLT2 inhibitor? Can J Hosp Pharm. 2018. 71:282–5.28.Chung MC., Hung PH., Hsiao PJ., Wu LY., Chang CH., Hsiao KY, et al. Sodium-glucose transport protein 2 inhibitor use for type 2 diabetes and the incidence of acute kidney injury in Taiwan. JAMA Netw Open. 2023. 6:e230453.
Article29.Korean Diabetes Association. Clinical practice guidelines for diabetes. 8th ed.Seoul: Korean Diabetes Association;2023.30.Neal B., Perkovic V., Mahaffey KW., de Zeeuw D., Fulcher G., Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017. 377:644–57.
Article31.Fralick M., Schneeweiss S., Patorno E. Risk of diabetic ketoacidosis after initiation of an SGLT2 Inhibitor. N Engl J Med. 2017. 376:2300–2.
Article32.McGovern A., Feher M., Munro N., de Lusignan S. Sodi-um-glucose co-transporter 2 (SGLT2) inhibitor: comparing trial data and real-world use. Diabetes Ther. 2017. 8:365–76.
Article33.Hill-Briggs F., Adler NE., Berkowitz SA., Chin MH., Gary-Webb TL., Navas-Acien A, et al. Social determinants of health and diabetes: a scientific review. Diabetes Care. 2020. doi: 10.2337/dci20-0053. [Epub ahead of print].
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Fasting is not always good: perioperative fasting leads to pronounced ketone body production in patients treated with SGLT2 inhibitors: a case report
- SGLT2 Inhibitors: Emerging Drugs in Heart Failure
- Chronic Kidney Disease and SGLT2 Inhibitors
- Emerging Safety Issues of Dipeptidyl Peptidase-4 Inhibitors and Sodium Glucose Cotransporter 2 Inhibitors: How to Interpret and Apply in Clinical Practice
- Glucose Lowering Effect of SGLT2 Inhibitors: A Review of Clinical Studies