Clin Endosc.
2024 Mar;57(2):246-252. 10.5946/ce.2023.075.
Safety of endoscopic ultrasound-guided hepaticogastrostomy in patients with malignant biliary obstruction and ascites
- Affiliations
-
- 1Department of Gastroenterology, Aichi Cancer Center Hospital, Nagoya, Japan
- KMID: 2553762
- DOI: http://doi.org/10.5946/ce.2023.075
Abstract
- Background/Aims
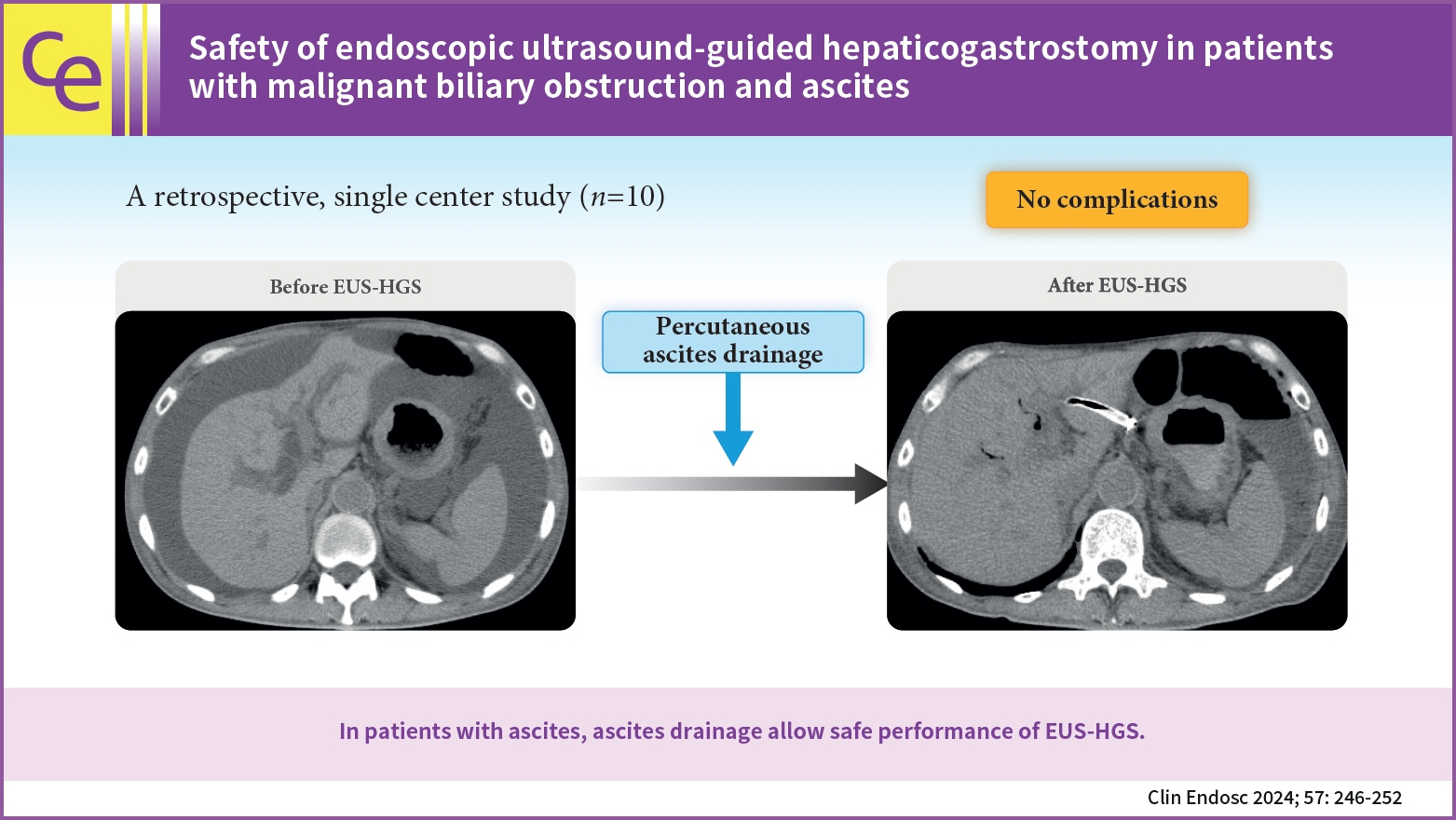
Endoscopic ultrasound (EUS)-guided hepaticogastrostomy (EUS-HGS) is useful for patients with biliary cannulation failure or inaccessible papillae. However, it can lead to serious complications such as bile peritonitis in patients with ascites; therefore, development of a safe method to perform EUS-HGS is important. Herein, we evaluated the safety of EUS-HGS with continuous ascitic fluid drainage in patients with ascites.
Methods
Patients with moderate or severe ascites who underwent continuous ascites drainage, which was initiated before EUS-HGS and terminated after the procedure at our institution between April 2015 and December 2022, were included in the study. We evaluated the technical and clinical success rates, EUS-HGS-related complications, and feasibility of re-intervention.
Results
Ten patients underwent continuous ascites drainage, which was initiated before EUS-HGS and terminated after completion of the procedure. Median duration of ascites drainage before and after EUS-HGS was 2 and 4 days, respectively. Technical success with EUS-HGS was achieved in all 10 patients (100%). Clinical success with EUS-HGS was achieved in 9 of the 10 patients (90 %). No endoscopic complications such as bile peritonitis were observed.
Conclusions
In patients with ascites, continuous ascites drainage, which is initiated before EUS-HGS and terminated after completion of the procedure, may prevent complications and allow safe performance of EUS-HGS.
Keyword
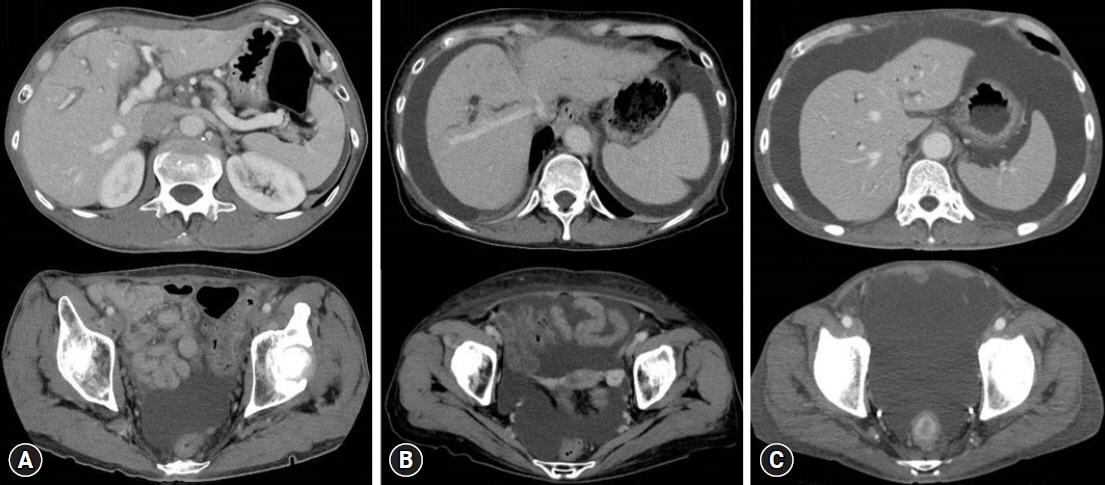
Figure
Reference
-
1. Sharaiha RZ, Kumta NA, Desai AP, et al. Endoscopic ultrasound-guided biliary drainage versus percutaneous transhepatic biliary drainage: predictors of successful outcome in patients who fail endoscopic retrograde cholangiopancreatography. Surg Endosc. 2016; 30:5500–5505.2. Lee TH, Choi JH, Park DH, et al. Similar efficacies of endoscopic ultrasound-guided transmural and percutaneous drainage for malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2016; 14:1011–1019.3. Sharaiha RZ, Khan MA, Kamal F, et al. Efficacy and safety of EUS-guided biliary drainage in comparison with percutaneous biliary drainage when ERCP fails: a systematic review and meta-analysis. Gastrointest Endosc. 2017; 85:904–914.4. Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainage for benign biliary diseases. Clin Endosc. 2019; 52:212–219.5. Giovannini M, Moutardier V, Pesenti C, et al. Endoscopic ultrasound-guided bilioduodenal anastomosis: a new technique for biliary drainage. Endoscopy. 2001; 33:898–900.6. Kawakubo K, Isayama H, Kato H, et al. Multicenter retrospective study of endoscopic ultrasound-guided biliary drainage for malignant biliary obstruction in Japan. J Hepatobiliary Pancreat Sci. 2014; 21:328–334.7. Bang JY, Navaneethan U, Hasan M, et al. Stent placement by EUS or ERCP for primary biliary decompression in pancreatic cancer: a randomized trial (with videos). Gastrointest Endosc. 2018; 88:9–17.8. Paik WH, Lee TH, Park DH, et al. EUS-guided biliary drainage versus ERCP for the primary palliation of malignant biliary obstruction: a multicenter randomized clinical trial. Am J Gastroenterol. 2018; 113:987–997.9. Park JK, Woo YS, Noh DH, et al. Efficacy of EUS-guided and ERCP-guided biliary drainage for malignant biliary obstruction: prospective randomized controlled study. Gastrointest Endosc. 2018; 88:277–282.10. Isayama H, Nakai Y, Itoi T, et al. Clinical practice guidelines for safe performance of endoscopic ultrasound/ultrasonography-guided biliary drainage: 2018. J Hepatobiliary Pancreat Sci. 2019; 26:249–269.11. Hamada T, Isayama H, Nakai Y, et al. Transmural biliary drainage can be an alternative to transpapillary drainage in patients with an indwelling duodenal stent. Dig Dis Sci. 2014; 59:1931–1938.12. Khashab MA, El Zein MH, Sharzehi K, et al. EUS-guided biliary drainage or enteroscopy-assisted ERCP in patients with surgical anatomy and biliary obstruction: an international comparative study. Endosc Int Open. 2016; 4:E1322–E1327.13. Nakai Y, Kogure H, Isayama H, et al. Endoscopic ultrasound-guided biliary drainage for unresectable hilar malignant biliary obstruction. Clin Endosc. 2019; 52:220–225.14. Kongkam P, Tasneem AA, Rerknimitr R. Combination of endoscopic retrograde cholangiopancreatography and endoscopic ultrasonography-guided biliary drainage in malignant hilar biliary obstruction. Dig Endosc. 2019; 31 Suppl 1:50–54.15. Poincloux L, Rouquette O, Buc E, et al. Endoscopic ultrasound-guided biliary drainage after failed ERCP: cumulative experience of 101 procedures at a single center. Endoscopy. 2015; 47:794–801.16. Paik WH, Park DH. Outcomes and limitations: EUS-guided hepaticogastrostomy. Endosc Ultrasound. 2019; 8(Suppl 1):S44–S49.17. Martins FP, Rossini LG, Ferrari AP. Migration of a covered metallic stent following endoscopic ultrasound-guided hepaticogastrostomy: fatal complication. Endoscopy. 2010; 42 Suppl 2:E126–E127.18. Prachayakul V, Thamtorawat S, Siripipattanamongkol C, et al. Bleeding left hepatic artery pseudoaneurysm: a complication of endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2013; 45 Suppl 2 UCTN:E223–E224.19. Nakajima TE, Yamaguchi K, Boku N, et al. Randomized phase II/III study of 5-fluorouracil/l-leucovorin versus 5-fluorouracil/l-leucovorin plus paclitaxel administered to patients with severe peritoneal metastases of gastric cancer (JCOG1108/WJOG7312G). Gastric Cancer. 2020; 23:677–688.20. Hara H, Kadowaki S, Asayama M, et al. First-line bolus 5-fluorouracil plus leucovorin for peritoneally disseminated gastric cancer with massive ascites or inadequate oral intake. Int J Clin Oncol. 2018; 23:275–280.21. Cotton PB, Eisen GM, Aabakken L, et al. A lexicon for endoscopic adverse events: report of an ASGE workshop. Gastrointest Endosc. 2010; 71:446–454.22. Maranki J, Hernandez AJ, Arslan B, et al. Interventional endoscopic ultrasound-guided cholangiography: long-term experience of an emerging alternative to percutaneous transhepatic cholangiography. Endoscopy. 2009; 41:532–538.23. Chantarojanasiri T, Ratanachu-Ek T, Pausawasdi N. What you need to know before performing endoscopic ultrasound-guided hepaticogastrostomy. Clin Endosc. 2021; 54:301–308.24. Ogura T, Higuchi K. Technical tips for endoscopic ultrasound-guided hepaticogastrostomy. World J Gastroenterol. 2016; 22:3945–3951.25. Sportes A, Camus M, Greget M, et al. Endoscopic ultrasound-guided hepaticogastrostomy versus percutaneous transhepatic drainage for malignant biliary obstruction after failed endoscopic retrograde cholangiopancreatography: a retrospective expertise-based study from two centers. Therap Adv Gastroenterol. 2017; 10:483–493.26. Marx M, Caillol F, Sfumato P, et al. EUS-guided hepaticogastrostomy in the management of malignant biliary obstruction: Experience and learning curve in a tertiary referral center. Dig Liver Dis. 2022; 54:1236–1242.27. Okuno N, Hara K, Mizuno N, et al. Infectious peritonitis after endoscopic ultrasound-guided biliary drainage in a patient with ascites. Gastrointest Interv. 2018; 7:40–43.28. Ogura T, Yamamoto K, Sano T, et al. Stent length is impact factor associated with stent patency in endoscopic ultrasound-guided hepaticogastrostomy. J Gastroenterol Hepatol. 2015; 30:1748–1752.29. Okuno N, Hara K, Mizuno N, et al. Stent migration into the peritoneal cavity following endoscopic ultrasound-guided hepaticogastrostomy. Endoscopy. 2015; 47 Suppl 1 UCTN:E311.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic ultrasound-guided biliary drainage in malignant distal biliary obstruction
- Endoscopic Ultrasound-Guided Hepaticogastrostomy: Technical Review and Tips to Prevent Adverse Events
- Endoscopic ultrasound-guided biliary drainage in malignant hilar obstruction
- Recent development of endoscopic ultrasound-guided biliary drainage
- Technical Review of Developments in Endoscopic Ultrasound-Guided Hepaticogastrostomy